Musculoskeletal Pathology Discussion-Functional Anatomy & Physiology
Copyright November 2003 Ted Nissen
TABLE OF
CONTENTS
1 Embryology of the Musculoskeletal
System
4 Assessment of Musculoskeletal
Disorders
6 Peripheral Joint Mobilization
Techniques
7 Automobilization Techniques for
the Extremities
10 Shoulder and Shoulder Girdle
18 Spine-General Structure and
Biomechanical Considerations Kessler
1 Embryology of the Musculoskeletal System
2 Arthrology
2.1
2.2 Kinematics
2.2.1 Classification of Joint Surfaces and Movements
2.2.2 Joint Surfaces
2.2.3 Anatomical Position, Axes, and
Planes
Kendall 11
Back Table of Contents References
2.2.3.1 Anatomical Position
2.2.3.1.1 The neutral or zero position for measuring
joint motion is as follows.
2.2.3.1.1.1 Erect posture
2.2.3.1.1.2 Face forward
2.2.3.1.1.3 Palms of hands forward
2.2.3.1.1.4 Fingers and thumbs in extension
2.2.3.1.1.5 Feet flat on the floor
2.2.3.1.2 The sections below on planes and axes will
use this position as reference.
2.2.3.2
Axes
2.2.3.2.1 An axis is a straight line about which the
joint rotates. The three basic axes described below are at right angles to each
other.
2.2.3.2.1.1 Sagittal axis
2.2.3.2.1.1.1
Placed on the
Sagittal plane it runs horizontally from anterior to posterior. The movements
of abduction and adduction occur around this axis in a coronal plane.
2.2.3.2.1.2 Coronal (Frontal) Axis
2.2.3.2.1.2.1
A horizontal
line in the coronal plane situated from side to side. Flexion and extension
occur about this axis in the Sagittal plane.
2.2.3.2.1.3 Longitudinal Axis
2.2.3.2.1.3.1
This is a
vertical line extending in a superior –inferior direction. Medial and lateral
rotation, and horizontal abduction and adduction occur in the transverse plane.
2.2.3.2.1.4 Exceptions
2.2.3.2.1.4.1
These
exceptions are explained in the sections for the thumb and scapula.
2.2.3.3
Planes
Back Table of Contents References
2.2.3.3.1 The three basic planes of reference are
derived from the dimensions in space and are at right angles to each other.
2.2.3.3.2 Sagittal Plane
2.2.3.3.2.1 The Sagittal plane is vertical and extends
from front to back, deriving its name from the direction of the Sagittal suture
of the skull. It may also be called an anterior-posterior plane. The median
Sagittal plane, midsagittal, divides the body into right and left halves.
2.2.3.3.3 Coronal (Frontal) Plane
2.2.3.3.3.1 The coronal plane is vertical and extends
from side to side, deriving its name from the direction of the coronal suture
of the skull. It is also called the frontal or lateral plane, and divides the
body into an anterior and a posterior portion.
2.2.3.3.4 Transverse (Horizontal) Plane
2.2.3.3.4.1 A transverse plane is horizontal and
divides the body into upper (cranial) and lower (caudal) portions
2.2.3.4
Center
of Gravity
2.2.3.4.1 The point at which the three midplanes of
the body intersect is the center of gravity which in an ideally aligned posture
in a so-called average adult human being, slightly anterior to the first or
second sacral segment.
2.2.3.5
Line
of Gravity
2.2.3.5.1 The line of gravity is a vertical line
through the center of gravity
2.2.4 Joint Movements
Back Table of Contents References
2.2.4.1
Basic
Joint Movements
Kendall 13
2.2.4.1.1 Flexion and Extension
2.2.4.1.1.1
Coronal Axis
2.2.4.1.1.1.1
2.2.4.1.1.2
Flexion
2.2.4.1.1.2.1
2.2.4.1.1.3
Extension
2.2.4.1.1.3.1
2.2.4.1.1.4
Embryonic
Development
2.2.4.1.1.4.1
2.2.4.1.2
Hyperextension
Back Table
of Contents References
2.2.4.1.2.1
2.2.4.1.3
Abduction and
Adduction
2.2.4.1.3.1
Sagittal Axis
2.2.4.1.3.1.1
2.2.4.1.3.2
Abduction and
Adduction
2.2.4.1.3.2.1
2.2.4.1.4
Lateral
Flexion
2.2.4.1.4.1
2.2.4.1.5
Gliding
2.2.4.1.5.1
2.2.4.1.6
Circumduction
2.2.4.1.6.1
2.2.4.1.7 Rotation
Back Table of Contents References
2.2.4.1.7.1 Longitudinal Axis
2.2.4.1.7.1.1
2.2.4.1.7.2 Lower Extremities
2.2.4.1.7.2.1
2.2.4.1.7.3 Upper Extremities
2.2.4.1.7.3.1
2.2.4.1.8
Tilt
2.2.4.1.8.1
2.2.4.1.8.2 Head and Pelvis Anterior and Posterior Tilt
2.2.4.1.8.2.1
2.2.4.1.8.3
Head and
Pelvis Lateral Tilt
2.2.4.1.8.3.1
2.2.4.1.8.4
Scapula
2.2.4.1.8.4.1
2.2.4.2 Movements of Specific Joints
2.2.4.2.1 Metacarpophalangeal Joints of Fingers
2.2.4.2.1.1 Abduction and Adduction
2.2.4.2.1.1.1 Occurs about a Sagittal axis. The line of reference for abduction and adduction of the fingers is the axial line through the third digit.
2.2.4.2.1.2 Abduction
2.2.4.2.1.2.1 Abduction is movement in the plane of the palm away from the axial line, spreading fingers wide apart. The third digit may move in abduction both ulnarly and radially from the axial line.
2.2.4.2.1.2.2 Movement in the plane of the palm away from a axial line of reference through the third metacarpal & digit
2.2.4.2.1.2.3 Simply movement away from the third finger
2.2.4.2.1.3 Adduction
2.2.4.2.1.3.1 Adduction is movement in the plane of the palm toward the axial line, that is, closing the extended fingers together sideways.
2.2.4.2.1.4 Circumduction
2.2.4.2.1.4.1 Circumduction is the combination of flexion, abduction, extension, and adduction movements performed consecutively, in either direction, at the Metacarpophalangeal joints of the fingers. Extension in these condyloid joints is somewhat limited so that the base of the cone described by the fingertip is relatively small.
2.2.4.2.2 Ankle Joint
2.2.4.2.2.1 The ankle joint is a ginglymus or hinge joint formed by the articulation of the tibia and fibula with the talus. The axis about which motion takes place extends obliquely from the posterolateral aspect of the fibular malleolus to the Anteromedial aspect of the tibial malleolus.
2.2.4.2.2.2 Flexion and Extension
2.2.4.2.2.2.1 These movements occur about the oblique axis. Flexion (plantarflexion) is movement of the foot in which the plantar surface moves in a caudal and posterior direction. Extension (dorsiflexion) is movement of the foot in which the dorsal surface moves in an anterior and cranial direction.
2.2.4.2.2.2.2 The knee should be flexed when measuring dorsiflexion. With the knee flexed, the ankle joint can be dorsiflexed about 20°. If the knee is extended, the gastrocnemius will limit the range of motion to about 10° of dorsiflexion. The range of motion in plantar flexion is approximately 45°.
2.2.4.2.3 Subtalar Joint (Talocalcaneonavicular)
2.2.4.2.3.1 The subtalar joint is a modified plane or gliding joint formed by the articulation of the talus and the calcaneus. The talus also articulates with the navicular, and the talonavicular joint is involved in the movements ascribed to the subtalar joint.
2.2.4.2.3.2 Supination and Pronation
2.2.4.2.3.2.1 Movements permitted by the subtalar and talocalcaneonavicular joints. Supination is rotation of the foot in which the sole of the foot moves in a medial direction; pronation is rotation in which the sole of the foot moves in a lateral direction.
2.2.4.2.4 Transverse Tarsal Joints
2.2.4.2.4.1 The transverse tarsal joints are formed by the articulations of the talus with the navicular, and the calcaneus with the cuboid.
2.2.4.2.4.2 Adduction and Abduction
2.2.4.2.4.2.1 Movements of the forefoot permitted by the transverse tarsal joints, adduction is movement of the forefoot in a medial direction and abduction is movement in a lateral direction.
2.2.4.2.4.3 Inversion
2.2.4.2.4.3.1 A combination of supination and forefoot adduction. It is more free in plantar flexion than in dorsiflexion.
2.2.4.2.4.3.2 Rotation of the foot and movement of the forefoot in a medial direction
2.2.4.2.4.4 Eversion
2.2.4.2.4.4.1 A combination of pronation and forefoot abduction. It is more free in dorsiflexion than in plantar flexion.
2.2.4.2.4.4.2 Rotation of the foot and movement of the forefoot in a lateral direction
2.2.4.2.5 Metatarsophalangeal Joints
2.2.4.2.5.1 The metatarsophalangeal joints are condyloid, formed by the articulation of the distal ends of the metatarsals with the adjacent ends of the proximal phalanges.
2.2.4.2.5.2 Flexion and extension
2.2.4.2.5.2.1 Movements about a coronal axis. Flexion is movement in a caudal direction, extension is movement in a cranial direction. The range of motion in adults is variable, but 30° flexion and 40° extension may be considered an average range for good function of the toes.
2.2.4.2.5.3 Adduction and Abduction
2.2.4.2.5.3.1 Movements about a sagittal axis. The line of reference for adduction and abduction of the toes is the axial line projected distally in line with the second metatarsal and extending through the second digit.
2.2.4.2.5.3.2 Abduction is movement away from a Sagittal line of reference through the second metatarsal & digit.
2.2.4.2.5.3.3 Simply abduction is movement away from the second toe.
2.2.4.2.5.3.4 Adduction is movement toward the axial line, and abduction is movement away from it, as in spreading the toes apart. Because abduction of the toes is restricted by the wearing of shoes, this movement is markedly limited in most adults and little attention is paid to the ability to abduct.
2.2.4.2.5.4 Interphalangeal Joints of toes
2.2.4.2.5.4.1 The Interphalangeal joints are ginglymus or hinge joints formed by the articulations of adjacent surfaces of phalanges.
2.2.4.2.5.4.2 Flexion and extension are movements about a coronal axis with flexion being movement in a caudal direction and extension movement in a cranial direction.
2.2.5 Arthrokinematics
2.2.6 Joint Play
2.2.7 Conjunct rotation
2.2.8 Summary of Joint Function
2.3 Clinical Applications
2.3.1 Terminology
2.3.2 Analysis of Accessory Joint Motions
2.4 Neurology
2.4.1
2.4.2 Innervation
2.4.3 Receptors
2.4.3.1
2.4.3.2 Type 1
2.4.3.3 Type 2
2.4.3.4 Type 3
2.4.3.5 Type 4
2.4.4 Clinical Considerations
2.5 Joint Nutrition
2.6 Lubrication
2.6.1
2.6.2 Models of Joint Lubrication
2.6.3 Resolving Problems of Joint-Surface Wear
2.7 Approach to Management of Joint Dysfunction
2.7.1 Pathologic Considerations
2.7.1.1 Increased Rate of Tissue Breakdown
2.7.1.2 Reduced Rate of Tissue Breakdown
2.7.1.3 Increased Rate of Tissue Production
2.7.1.4 Reduced Rate of Tissue Production and Repair
2.7.1.5 Intervention and Communication
2.7.1.6 Arthrosis
2.7.1.7 The Degenerative Cycle
2.7.1.8 Capsular Tightness
2.7.1.9 Joint Effusion
2.7.1.10 Relative Capsular Fibrosis
2.7.1.11 Clinical Considerations
3 Pain
3.1 Melzack-Wall Gate Theory AK Synopsis 259
3.1.1 Melzack and Wall[1] [2] state that nerve impulses are brought from the receptors to both large fibers and small fibers. These two types of fibers have different characteristics.
3.1.1.1 Large Fibers
3.1.1.1.1 Myelinated A Fibers
3.1.1.1.2 Fast conduction (up to 120 Meters/second)
3.1.1.1.3 Have receptors that react to low and moderate intensity stimuli
3.1.1.2 Small Fibers
3.1.1.2.1 Unmyelinated C Fibers
3.1.1.2.2 Slow conduction (down to 1 meter/second)
3.1.1.2.3 Have receptors that react to low, moderate, and high intensity stimuli
3.1.2 When there is a stimulus to a receptor field, both large and small fibers conduct impulses. As the stimulation becomes noxious (such as a pain stimulus), the small fibers conduct with greater intensity due to their receptors’ characteristic reaction to high intensity stimuli.
3.1.3 The large and small fibers activate the transmission cells (T cells), which project the information to the brain. The T cells are located in the spinal cord dorsal horns, apparently in lamina 5. They fire when a certain threshold of stimulation is reached.
3.1.4 The large diameter fibers and the small diameter fibers give off branches to the substantia gelatinosa. The substantia gelatinosa is located in the dorsal horn lamina 2 and 3. As a functional unit it extends the length of the spinal cord on each side. Its cells connect with one another by short fibers; they influence each other at distant sites on the same side by means of Lissauer’s tract, and on the opposite side by means of commissural fibers that cross the cord. The substantia gelatinosa therefore receives afferent input from large and small fibers. Its cells connect with one another to different levels of the spinal cord and they communicate with the contralateral side. The spinal gate mechanism appears to be at the substantia gelatinosa.
3.1.5 Activity in the large fibers stimulates the substantia gelatinosa; activity of the small fibers inhibits it; Activity of the substantia gelatinosa inhibits activity of the T cell. Thus the balance of activity between the large and small fibers either activates or deactivates the substantia gelatinosa which, in turn, either allows activity at the T cell of inhibits activity there. When the T cell is inhibited, information received by the cell cannot be transmitted to the brain.
3.1.6 Adaptation to mild and moderate stimuli, primarily conducted by the large nerve fibers, is accomplished by this gate mechanism. For example, when you sit down in a chair to read a book, your nervous system soon adapts to the pressure of sitting in the chair, your hand lying in your lap, and the pressure of the book in your hand. These mild pressure stimuli are conducted primarily by the large fibers to both the substantia gelatinosa and the T cells. Upon first conduction, the T cells transmit information to the brain, which is interpreted as pressure. With continued stimulation, the substantia gelatinosa sends impulses of an inhibiting nature to the T cells. This reduces the information about the sitting position, which is being transmitted to the brain, so the body (large fibers) adapts to the stimulation. If, on the other hand, you sit on a sharp tack, there would not only be transmission by the large fibers but also increased transmission by the small fibers, which are activated more by high intensity stimulation. The activity of the small fibers stimulates the substantia gelatinosa and the AT cells. The immediate response is transmission by the T cells to the brain, informing it of the noxious stimuli. The continued inhibitory stimulation of the substantia gelatinosa would turn its activity off, giving no inhibitory action to the T cells; consequently, the T cells would continue to transmit information of a pain stimulus to the brain. This is the manner in which the gate is held open by pain stimuli
3.1.7 Continued sitting on the tack and the subsequent transmission of the T cells trigger the action system required by the pain. The activity will be as follows;
3.1.7.1 Perceptual information, giving location, magnitude, and spatiotemporal properties of the noxious stimulus
3.1.7.2 Motivational tendency toward escape or attack
3.1.7.3 Cognitive information based on analysis of past experience and probable outcome of different response strategies.
3.1.8 The interplay of these three activities could then influence motor mechanisms responsible for the complex pattern of overt responses that characterize pain.
3.1.9 Also added to the model is the central control mechanism. By this mechanism central activities, such as anxiety or excitement, may open or close the gate for inputs from any part of the body. The central control cortical projections and reticular projections explain how higher central nervous system processes- such as attention, anxiety, anticipation, and past experience- exert a powerful influence on pain processes.
4 Assessment of Musculoskeletal Disorders
5 Concepts of Management
6 Peripheral Joint Mobilization Techniques
7 Automobilization Techniques for the Extremities
8 Friction Massage
8.1 Introduction
8.1.1 A particularly important massage technique in the management of many, musculoskeletal disorders is deep transverse friction massage. Its importance and the rationale and technique of application have not been well described in the traditional literature.
8.1.2 Many of the chronic musculoskeletal disorders seen clinically are manifestations of the body's response to the fatigue stresses. Tissues tend to respond to fatigue stresses by increasing the rate of tissue production. Thus, prolonged abnormal stresses to a tissue will lead to tissue hypertrophy, provided that the nutritional status of the tissue is not compromised and that the stress rate (the rate of tissue breakdown) does not exceed the rate at which this tissue can repair the microdamage. Under continuing stress, if nutrition to the tissue is affected or if the rate of tissue breakdown is excessive, the tissue will gradually atrophy and weaken to the point of eventual failure. Tissues that normally have a low metabolic rate (usually those that are relatively poorly vascularized) are most susceptible to such degeneration. Such tissues include articular cartilage, inter-articulate fibrocartilage, tendons, and some ligaments. On the other hand, those tissues with good vascularity and a normally high rate of turnover, such as cancellous bone, muscle, capsular tissue, and some ligaments, are more likely to respond by undergoing hypertrophy. This results in increased density of the structural elements. Of course, even the structures may not be able to keep up with the rate of tissue breakdown is the stress rate is two or under conditions of reduced nutrition (E.G., hypovascularity)
8.1.3 Under conditions of mildly increased stress rates, the body has the ability to adapt adequately, and no pathological state (i.e. pain, inflammation, or dysfunction) results. Such conditions might even include situations of high magnitude stresses if the high stress levels are induced gradually and the stresses are intermittent enough to allow an interval for adequate repair to take place. A typical example is the individual engaging in vigorous athletic activities who goes through a period of gradual training. The training period allows for adequate maturation of new tissue so that structural elements become oriented in ways that best attenuate energy without yielding. Such energy attenuation requires that there be a sufficient mass of tissue to provide some resistance to deformation, but it also requires that the structure be adequately extensible to minimize the strain on individual structural elements. To increase the ability of a structure to attenuate the energy of work done on it (a force tending to deform the structure), new collagen is produced to increase the tissues total ability to resist the force. However, this new collagen must be sufficiently mobile to permit some deformation. The less it deforms, the greater the resistance the tissue must offer. The greater the resistance it must offer, the greater will be the internal strain on individual collagen fibers or bony trabeculae. The greater the strain on individual structural elements, the greater the rate of microdamage. As the rate of microdamage increases, so does likelihood of pain and inflammation. As you can see, a more massive tissue is not necessarily one that will permit normal functioning under increased stress. It must also be deformable, and deformability requires time for the new structural elements (collagen fibers and bony trabeculae) to assume the proper "weave."
8.1.4 The effects of the weave, or orientation, a structural elements in contributing to the extensibility of a structure as a whole can be appreciated by examining a Chinese "finger trap". You can lengthen and shorten the finger trap without changing the length of any of the individual fibers composing it. Its extensibility is due entirely to the weave of the fibers and interfiber mobility. Thus, you can apply an extending force to the structure without inducing internal strain on any of the individual fibers. If the fibers were not in the proper weave or if they were to stick to one another, the deforming force would be met with greater resistance by the structure and greater internal strain to individual fibers. The body adapts to mildly increased stress rates by laying down collagen precursors, which, in response to imposed stresses, polymerize into collagen fibers. The fibers become oriented in the proper weave to allow deformability of the tissue.
8.1.5 Under abnormally high stress levels or altered nutritional conditions, the body’s ability to adapt may be inadequate. The particular structure may not be able to produce new tissue fast enough, or the new tissue that is produced may not have sufficient time or proper inducement to mature. In the former situation, the tissue will degenerate, whereas in the latter, pain and inflammation are likely to result if stresses continue. Tissue degeneration must be treated by reducing stress levels and/or increasing nutrition to the tissue, depending on the underlying cause. Typical examples of such tissue degeneration would include the degradation of articular cartilage in degenerative joint disease, and the lesions that commonly affect the soft tissues of the diabetic foot. Articular cartilage, being avascular and having a normally low metabolic turnover, does not adapt well to increased stress levels and is thus susceptible to the fatigue degeneration. The diabetic foot may have a nutritional deficit because of vascular changes and possibly increased stresses secondary to reduced sensory feedback, leaving it abnormally susceptible to tissue breakdown.
8.1.6 Situations in which the new tissue does not mature adequately are typically those in which the stress levels are not sufficient to cause degeneration but are too excessive to allow time for normal tissue modelling. In bone, the condition is referred to as sclerosis; in capsules, ligaments, and tendons, in may be referred to as fibrosis. In both situations there is often a normal or increased amount of tissue, but the tissue is not sufficiently deformable to attenuate the energy of loading from use of the part. This can cause pain, inflammation, and/or increased stresses to adjacent tissues. Correction of such conditions requires that stress levels be reduced while stresses sufficient to stimulate normal tissue modelling are maintained. In addition, normal extensibility of the structure must be restored. This requires that interfiber mobility be increased. The nutritional status of the tissue must also be considered.
8.1.7 There are many common musculoskeletal disorders that may be related to abnormal or inadequate tissue modelling. Bony sclerosis typically occurs in degenerative joint disease when there are abnormal compressive stresses to a joint. Most tendonitis can be attributed to continued abnormal stresses to a tendon, which preclude adequate tissue modelling and create a structure that is not sufficiently deformable. This is especially true of the condition often referred to as tennis elbow, in which the origins of the extensor carpi radialis brevis becomes fibrosed, and a chronic inflammatory process arises. Rotator cuff tendonitis, usually involving the supraspinatus or infraspinatus regions of the tendinous cuff, is a very common disorder in which normal modelling is compromised by hypovascularity to the area of involvement. Often these lesions at the shoulder progress to stage at which gradual degeneration and eventual failure ensue. It is likely that the capsular fibrosis associated with "frozen shoulder" is a similar disorder of tissue modelling; the joint capsule hypertrophies in response to increase stress levels, but in doing so loses its extensibility. Abnormal tissue modelling will also result when a tissue is immobilized during the repair phase of an inflammatory process. Thus, a fracture may "heal," but normal modelling bony trabecula requires resumption of normal stress levels. Similarly, a joint capsule will become fibrosed when the joint is immobilized following arthrotomy; collagen is laid down in response to the traumatic inflammatory process affecting the synovium, but the lack of movement permits in an organized network of fibers that forms abnormal interfiber bonds (adhesions) that do not extend normally when the part is moved.
8.1.8 The approach to treatment of conditions in which continued stresses have not allowed the structure to mature adequately must include measures to reduce stresses to the part. We must consider means of reducing loading of the part as well as means of preventing excessive internal strain. Reduced loading might be accomplished through control of activities, the use of orthotic devices to control alignment or movement, or the use of assistive devices such as crutches. Also, to reduce loading of a particular tissue, the capacity of other tissues to attenuate more of the energy of loading might be increased. Increasing the strength and activities of related muscles often does this. Thus, if we wish to reduce the likelihood of excessive loading of the anterior talofibular ligament, the peroneal muscles should be strengthened. However, we can also strap the ankle to provide additional afferent input to reflexively enhance the ability of the peroneals to contract.
8.1.9 Reduction in stress levels alone, however, will not assure that adequate maturation will take place. As mentioned earlier, stress to the part is a necessary stimulus for the restoration of normal alignment of structural elements. This apparent paradox is understood when we consider that reducing stress is necessary in order to allow new tissue to be laid down and reconstituted, while at the same time some stress is necessary to optimise the nutritional status of the part and to effect proper orientation and mobility of the new tissue. Consequently, in the case of most chronic musculoskeletal disorders, resolution is not likely to take place with either complete rest of the part or unrestricted use. A judgment must be made, then, as to the appropriate activity level for a particular disorder and the rate at which normal activities can be resumed. This judgment must be based on data gained from an examination that reflects the nature and extent of the pathologic process as well as etiologic considerations. Knowledge of the healing responses of musculoskeletal tissues and of their responses to various stress conditions must also be applied.
8.1.10 In situations in which significant reduction of activities is necessary in order to allow healing to current, there are measures that the therapist can, and should take. The practitioner must help prevent undue dysfunction that may result from a mass of tissue being laid down as unorganized, adherent cicatrix, and from the atrophy of related muscle groups that is likely to take place. There a few conditions, even of an acute inflammatory nature, in which some gentle range of motion and isometric muscle exercises cannot be performed during the healing process without detrimental effects.
8.1.11 Some of the chronic disorders that can to be the most persistent are minor lesions of tendons and ligaments. These are often refractory to treatments such as rest and anti-inflammatory therapy because they are not chronic inflammatory lesions per se, but pathological processes resulting from abnormal modelling of tissue in response to fatigue stresses. Therefore, while rest allows new tissue to be produced, that which is produced is not of normal extensibility because of lack of a proper orientation of structural elements, abnormal adherence of structural elements to one another, and adherent to adjacent tissues. In some situations, most notably rotator cuff tendonitis, inadequate tissue nutrition is also a factor. Because the lack of extensibility that accompanies "healing" of these lesions, the structure becomes more susceptible to internal strain when stresses are resumed and less able to attenuate the energy of loads applied to it. The result is recurrence of a low-grade inflammatory process each time use of the part is resumed. The most common these disorders are supraspinatus tendonitis at the shoulder, tendonitis of the origin of the extensor carpi radialis brevis (tennis elbow), tendonitis of the abductor pollicis longus or extensor pollicis brevis tendons that the wrist (de Quervain’s disease), coronary ligament sprain at the knee, and anterior talofibular ligament sprain.
8.1.12 In such chronic, persistent lesions of tendons and ligaments- and occasionally muscle- procedures to promote normal mobility and extensibility of the involved structure are important components of the treatment program. Passive or active exercises that impose a longitudinal strain on the involved structure may be incorporated. However, this creates the risk of maintaining the weakened or unresolved state of healing by contributing to the rate of tissue micro damage. That is probably why these disorders can not to resolve spontaneously with varying degrees of activity. Too little activity results in loss of extensibility; too much activity does not allow for adequate healing. The appropriate compromise is difficult to judge.
8.1.13 Another method of promoting increased extensibility and mobility of the structure, while reducing stress levels and allowing healing to take place, is the use of deep transverse friction massage. This is a form of treatment advocated primarily Cyriax, but unfortunately not widely adopted to date. It involves applying a deep massage directly to the site of the lesion in an direction perpendicular to normal orientation of fibrous elements. This maintains mobility of the structure with respect to adjacent tissues and probably helps to promote increased interfiber mobility of the structure itself without longitudinally stressing it. It may also promote normal orientation of fibers as they are produced. This effect might be likened to be effective rolling your hand over and unorganized pile of toothpicks; eventually the toothpicks will all become oriented perpendicular the direction in which the hand moves. In some pathological processes, such as rotator cuff tendonitis, in which the etiology may be related to the nutritional deficit arising from hypovascularity, the hyperemia induced by the friction massage may also contribute to the healing response.
8.1.14 Although these effects of friction massage are highly conjectural, they're based on sound physiological and pathological concepts. Further support is provided by the often dramatically favorable results obtained clinically when friction massage is appropriately incorporated in a treatment program. Studies are needed, however, to substantiate the physiological effects and clinical efficacy of friction massage in these chronic disorders. Designing a legitimate clinical study would be difficult because most of the disorders for which friction massage seems to be effective do not present with measurable objective signs, and documentation of subjective improvement is usually unreliable. Basic studies of the effects of friction massage, however may be fashioned after previous investigations into the effects of exercise, immobility, and other variables on the healing and maturation of collagen tissue. Until we have more concrete evidence of the value for should massage succumb its use must be justified on in the considerations combined with "educated empiricism."
9 Relaxation
10 Shoulder and Shoulder Girdle
10.1 Review of Functional Anatomy
10.1.1
Shoulder
Girdle
Kendal 16
Back Table
of Contents References
10.1.1.1 Articulations
10.1.1.1.1
Clavicle
10.1.1.1.1.1
10.1.1.1.2
Scapula
10.1.1.1.2.1
10.1.1.2 Joint Motion
10.1.1.2.1
Sternoclavicular
Joint
10.1.1.2.1.1
10.1.1.3 Scapular Position
10.1.1.3.1
10.1.1.4 Muscular Attachments
10.1.1.4.1
10.1.1.5 Basic Movements
10.1.1.5.1
Adduction
10.1.1.5.1.1
10.1.1.5.2
Abduction
10.1.1.5.2.1
10.1.1.5.3
Lateral
or Upward Rotation
10.1.1.5.3.1
10.1.1.5.4
Medial
or Downward Rotation
10.1.1.5.4.1
10.1.1.5.5
Anterior
Tilt
10.1.1.5.5.1
10.1.1.5.6
Elevation
10.1.1.5.6.1
10.1.1.5.7
Depression
10.1.1.5.7.1
10.1.1.5.8
Note
10.1.1.5.8.1
10.1.2
Shoulder
(Glenohumeral) Joint Kendal 17
Back Table of Contents References
10.1.2.1 Kendall
10.1.2.1.1
Introduction
10.1.2.1.1.1
Type
of Joint
10.1.2.1.1.1.1
Synovial
10.1.2.1.1.1.2
Spheroid
(Ball & Socket)
10.1.2.1.1.2
The
head of the humerus and the glenoid cavity of the scapula form the Glenohumeral
joint.
10.1.2.1.2
Flexion
and Extension
10.1.2.1.2.1
Plane
of Movement
10.1.2.1.2.1.1
Sagittal
10.1.2.1.2.2
Axis
of Movement
10.1.2.1.2.2.1
Coronal
10.1.2.1.2.3
Range
of Movement (Flexion)
10.1.2.1.2.3.1
225°
10.1.2.1.2.3.2
The
arc of movement along the Sagittal plane begins at 45° extension forward
through the zero anatomical position and on to the 180° overhead position.
10.1.2.1.2.3.3
Other
Joint Involvement
10.1.2.1.2.3.3.1
Scapular
10.1.2.1.2.3.3.2
Glenohumeral
flexion accounts for only about 120° and the remaining 60° is achieved as a
result of abduction and lateral rotation of the scapula. The scapula moves in
this way to face the head of the humerus anteriorly to provide for its stable
placement in the joint cavity as it moves thru its arc to a fully vertical position.
10.1.2.1.2.3.3.3
The
scapular motion is at first variable but remains constant after about 60°
10.1.2.1.2.3.3.4
Inman
et al.[3]
observed that between 30° and 170° flexion the Glenohumeral joint moved 10° and
the scapula rotated 5° for every 15° of motion.
10.1.2.1.2.4
Range
of Movement (Extension)
Back Table of Contents References
10.1.2.1.2.4.1
225°
10.1.2.1.2.4.2
The
arc of movement along the Sagittal plane begins at 180° flexion backward
through the zero anatomical position and on to the 45° to the extended
position.
10.1.2.1.2.4.3
If the
elbow joint is flexed the range of shoulder joint extension will be increased
because the tension of the biceps will be released.
10.1.2.1.3
Abduction
and Adduction
10.1.2.1.3.1
10.1.2.1.3.2
Abduction
10.1.2.1.3.2.1
10.1.2.1.3.3
Adduction
10.1.2.1.3.3.1
10.1.2.1.4
Horizontal
Abduction and Adduction
10.1.2.1.4.1
10.1.2.1.4.2
Horizontal
Abduction
10.1.2.1.4.2.1
10.1.2.1.4.3
Horizontal
Adduction
10.1.2.1.4.3.1
10.1.2.1.5
Medial
and Lateral Rotation
10.1.2.1.5.1
10.1.2.1.5.2
Medial
Rotation
10.1.2.1.5.2.1
10.1.2.1.5.3
Lateral
Rotation
10.1.2.1.5.3.1
10.1.2.1.6
Circumduction
10.1.2.1.6.1
10.1.3 Osseous Structures Kessler 169
10.1.3.1 Glenohumeral Joint
10.1.3.1.1
Spinal
stability is essential for the adequate functioning of the shoulder girdle
complex, which includes the following osseous structures.
10.1.3.1.1.1
Upper
thoracic vertebrae
10.1.3.1.1.2
1st
and 2nd ribs
10.1.3.1.1.3
Manubrium
10.1.3.1.1.4
Scapula
10.1.3.1.1.5
Clavicle
10.1.3.1.1.6
Humerus
10.1.3.1.2
Full
Arm Elevation Essentials
10.1.3.1.2.1
Full
arm elevation can only be achieved when the upper thoracic vertebrae is able to
do the following on the ipsilateral side.
10.1.3.1.2.1.1
Extend
10.1.3.1.2.1.2
Rotate
10.1.3.1.2.1.3
Sidebend
10.1.3.1.2.2
The
first and second ribs must be able to descend and move posteriorly (with
vertebral rotation).
10.1.3.1.2.3
The following
joint structures must permit the Manubrium to sidebend and rotate to the
ipsilateral side.
10.1.3.1.2.3.1
Manubriosternal
10.1.3.1.2.3.2
Costomanubrial
10.1.3.1.2.3.3
Sternoclavicular
10.1.3.1.2.4
Mobility
of the scapulothoracic mechanism is dependant of the mobility of the following
joints.
10.1.3.1.2.4.1
Acromioclavicular
10.1.3.1.2.4.2
Sternoclavicular
10.1.3.1.2.5
The
Glenohumeral joint moves between 90° (active) and 120° (passive) elevation.
10.1.3.1.2.6
Full
arm elevation is accomplished in concert with the movement of the following
structures.
10.1.3.1.2.6.1
Scapular
rotation
10.1.3.1.2.6.2
Clavicular
elevation
10.1.3.1.2.6.3
Thoracic
extension
10.1.3.1.2.7
The
lower thoracic vertebrae must sidebend away from the side of motion.
10.1.3.1.2.8
Exaggeration
of lumbar Lordosis must accompany full arm elevation and is achieved by the
action of the spinal muscles.[4]
10.1.3.2 Acromioclavicular Joint
10.1.3.3 Sternoclavicular Joint
10.1.3.4 Scapulothoracic Mechanism
10.1.4 Ligaments
10.1.4.1 Glenohumeral Joint
10.1.4.2 Acromioclavicular Joint
10.1.4.3 Sternoclavicular Joint
10.1.5 Bursae
10.1.5.1
10.1.5.2 Subacromial or Subdeltoid Bursa
10.1.5.3 Subscapular Bursa
10.1.6 Vascular Anatomy of Rotator Cuff Tendons
10.1.6.1
10.2 Biomechanics
10.2.1 Joint Stabilization
10.2.2 Influence of the Glenohumeral Joint Capsule on Movement
10.2.3 Muscular Force Couple
10.2.4 Analysis of Shoulder Abduction
11 Elbow
11.1
Elbow
Joint
Kendall 18
Back Table of Contents References
11.1.1.1 Type of Joint
11.1.1.1.1
11.1.1.2 Movements Permitted
11.1.1.2.1
11.1.1.3 Description
11.1.1.3.1
11.1.2
Flexion
11.1.2.1
11.1.3
Extension
11.1.3.1
11.2
Radioulnar
Joint
Kendall 18
Back Table of Contents References
11.2.1 Type of Joint
11.2.1.1
11.2.2 Movements Permitted
11.2.2.1
11.2.3 Description
11.2.3.1
11.2.4
Supination
and Pronation
11.2.4.1
Supination
11.2.4.1.1
11.2.4.2
Pronation
11.2.4.2.1
11.2.4.3
Shoulder
Rotation
11.2.4.3.1
11.2.4.4
Neutral
or Zero Position
11.2.4.4.1
12 Wrist and Hand Complex
12.1
Wrist
Joint
Kendall 18
Back Table of Contents References
12.1.1
12.1.2
Flexion
and Extension
12.1.2.1
12.1.2.2
Flexion
12.1.2.2.1
12.1.2.3
Extension
12.1.2.3.1
12.1.3
Abduction
(Radial Deviation) and Adduction
12.1.3.1
12.1.3.2
Adduction
12.1.3.2.1
12.1.3.3
Abduction
12.1.3.3.1
12.1.4
Circumduction
12.1.4.1
12.2
Fingers Kendall 18
Back Table of Contents References
12.2.1 Carpometacarpal Joints of Fingers
12.2.1.1 Type of Joint
12.2.1.1.1
12.2.1.2 Movements Permitted
12.2.1.2.1
12.2.1.3 Description
12.2.1.3.1
12.2.2
Metacarpophalangeal
Joints of Fingers
12.2.2.1 Type of Joint
12.2.2.1.1
12.2.2.2 Movements Permitted
12.2.2.2.1
12.2.2.3 Description
12.2.2.3.1
12.2.2.4
Flexion
and Extension
12.2.2.4.1
12.2.2.4.2 Flexion
12.2.2.4.2.1
12.2.2.4.3 Extension
12.2.2.4.3.1
12.2.2.5
Abduction
and Adduction
12.2.2.5.1
12.2.2.5.2 Abduction
12.2.2.5.2.1
12.2.2.5.3 Adduction
12.2.2.5.3.1
12.2.2.6
Circumduction
12.2.2.6.1
12.2.3
Interphalangeal
Joints of Fingers
Back Table of Contents References
12.2.3.1 Type of Joint
12.2.3.1.1
12.2.3.2 Movements Permitted
12.2.3.2.1
12.2.3.3 Description
12.2.3.3.1
12.2.4
Carpometacarpal
Joint of Thumb
12.2.4.1 Type of Joint
12.2.4.1.1
12.2.4.2 Movements Permitted
12.2.4.2.1
12.2.4.3 Description
12.2.4.3.1
12.2.4.4 Adduction and Abduction
12.2.4.4.1
12.2.4.4.2 Adduction
12.2.4.4.2.1
12.2.4.4.3 Abduction
12.2.4.4.3.1
12.2.4.5 Rotation
12.2.4.5.1
12.2.4.6 Opposition
12.2.4.6.1
12.2.4.6.2 Muscles
12.2.4.6.2.1
12.2.4.7 Circumduction
12.2.4.7.1
12.2.5
Metacarpophalangeal
and Interphalangeal Joint of Thumb
Back Table of Contents References
12.2.5.1 Type of Joint
12.2.5.1.1
12.2.5.2 Movements Permitted
12.2.5.2.1
12.2.5.3 Description
12.2.5.3.1
12.2.5.4 Flexion and Extension
12.2.5.4.1
12.2.5.4.2 Flexion
12.2.5.4.2.1
12.2.5.4.3 Extension
12.2.5.4.3.1
12.2.5.5 Abduction, Adduction, and Rotation
12.2.5.5.1
13 Hip
13.1
Pelvis Kendall 20
Back Table of Contents References
13.1.1.1 Neutral Position
13.1.1.1.1
13.1.1.2 Anterior Pelvic Tilt
13.1.1.2.1
13.1.1.3 Posterior Pelvic Tilt
13.1.1.3.1
13.1.1.4 Lateral Pelvic Tilt
13.1.1.4.1
13.2
Hip
Joint
Kendall 20
13.2.1.1 Type of Joint
13.2.1.1.1
13.2.1.2 Movements Permitted
13.2.1.2.1
13.2.1.3 Range of Movement
13.2.1.3.1
13.2.1.4 Description
13.2.1.4.1
13.2.1.5 Flexion and Extension
13.2.1.5.1
13.2.1.5.2 Flexion
13.2.1.5.2.1
13.2.1.5.3 Extension
13.2.1.5.3.1
13.2.1.6 Abduction and Adduction
Back Table of Contents References
13.2.1.6.1
13.2.1.6.2 Abduction
13.2.1.6.2.1
13.2.1.6.3 Adduction
13.2.1.6.3.1
13.2.1.7 Lateral and Medial Rotation
13.2.1.7.1
13.2.1.7.2 Medial Rotation
13.2.1.7.2.1
13.2.1.7.3 Lateral Rotation
13.2.1.7.3.1
14 Knee
14.1
Knee
Joint
Kendall 21
Back Table of Contents References
14.1.1.1 Type of Joint
14.1.1.1.1
14.1.1.2 Movements Permitted
14.1.1.2.1
14.1.1.3 Range of Movement
14.1.1.3.1
14.1.1.4 Description
14.1.1.4.1
14.1.1.5 Flexion and Extension
14.1.1.5.1
14.1.1.5.2 Flexion
14.1.1.5.2.1
14.1.1.5.3 Extension
14.1.1.5.3.1
14.1.1.6 Hyperextension
14.1.1.6.1
14.1.1.7 Lateral and Medial Rotation
14.1.1.7.1
14.1.1.7.2
15 Ankle and Hindfoot
15.1 Neurology
15.1.1
15.2 Osteology
15.2.1
Introduction
15.2.1.1 The tibia flares at its distal end. As a result, the cross section of the bone changes from triangular, in the region of the shaft, to quadrangular in the area of the distal metaphyseal portion of the bone. Medially there is a distal projection of the tibia, the medial malleolus; located laterally is the fibular notch, which is concave anteroposteriorly for articulation with the distal end of the fibula. Along the medial side of the posterior surface is a groove for the passage of the tibialis posterior tendon. The term posterior malleolus .is often used to refer to the distal overhang of the posterior aspect of the tibia (Fig. 15-1).
15.2.1.2
The lateral surface of the medial
malleolus and the inferior surface of the tibia have a continuous cartilaginous
covering for articulation with the talus. The articular surface of the inferior
end of the tibia is concave anteroposteriorly. Mediolaterally, it is somewhat
convex, having a crest centrally that corresponds to the central groove in
.the trochlear surface of the talus. This, then, is essentially a sellar joint
surface. It is slightly wider anteriorly than posteriorly. The articular
surface of the medial malleolus is comma shaped with the "tail" of
the comma being situated posteriorly (see Fig. 15 -1). .
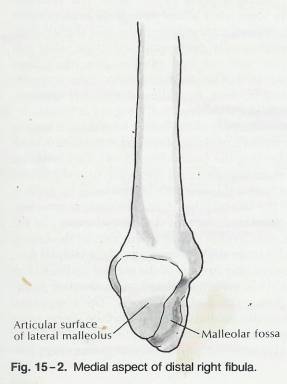
15.2.1.3 The fibula, which is quite narrow in the region of its shaft, becomes bulbous at its distal end (Fig. 152). This distal portion of the bone, the lateral malleolus, is triangular in cross section. When viewed from a lateral aspect, the fibula is somewhat pointed distally. The lateral malleolus extends farther distally and is situated more posteriorly than the medial malleolus. The medial aspect of the lateral malleolus is covered by a triangular cartilaginous surface for articulation with the lateral side of the talus. Above this surface, the fibula contacts the tibia in the fibular notch of the tibia. The apex of this triangular surface points inferiorly. There is a fairly deep depression in the posterior inferior region of the lateral malleolus termed the malleolar fossa .that can be easily palpated. The posterior talofibular ligament attaches in this fossa. There is a groove along the posterior aspect of the lateral malleolus through which the peroneus brevis tendon passes.
15.2.1.4 The talus constitutes the link between the leg and the tarsus (Fig. 15 - 3). It consists of a body, anterior. to which is, the head, The body and head of the talus are connected by a short neck.
15.2.1.5 The superior surface- of the body of the talus is covered with articular cartilage for articulation with the inferior surface of the tibia. This articular surface is continuous with the articular surfaces of the medial and lateral aspects of the talus. The superior surface is somewhat wider anteriorly than posteriorly, It is convex anteroposteriorly and slightly concave mediolaterally, corresponding to the sellar surface of the inferior end of the tibia mentioned previously. In this sense, the superior talar articular surface is trochlear, or pulley-like, and is often referred to as .the trochlea.
15.2.1.6 The lateral aspect of the body of the talus is largely covered by articular cartilage for articulation with the distal end of the fibula (Fig. 15 -4). This articular_ surface is triangular, with the apex situated inferiorly. Just below this apex is a lateral bony projection to which the lateral talocalcaneal ligament attaches.
15.2.1.7 The articular surface of the medial aspect of the talus is considerably smaller than that of the lateral side, and it faces slightly forward (Fig. 15 -5,) It. contacts the articular surface of the medial malleolus on the tibia. It is comma shaped, with the tail of the comma being situated posteriorly. The roughened area below the medial articular surface serves as an attachment for the deltoid ligament. The medial and lateral talar articular surfaces tend to converge posteriorly, leading to the wedge shape of the trochlea. It should be emphasized, however, that the lateral articular surface of the talus is perpendicular to the axis of movement at the ankle joint, whereas the medial surface is not. This has important biomechanical implications, which are discussed in the following section.
15.2.1.8 If one views the profiles of the lateral and medial sides of the trochlea, the lateral profile is seen as a section of a circle, whereas the medial profile may be viewed as sections of several circles of different radii; the medial profile is of smaller radius anteriorly than posteriorly.[5] More precisely stated, the contour medially is of gradually increasing radius anteroposteriorly, forming a cardioid profile. The importance of this is described in the section on biomechanics.
15.2.1.9
Posteriorly the body of the talus is
largely covered by a continuation of the trochlear articular surface as it slopes backward (Fig. 15 - 6).
At the inferior extent of the posterior aspect is the nonarticular posterior
process. The posterior process consists of a lateral and a smaller medial
tubercle, with an intervening groove through which passes the tension of the
flexor hallucis longus.
15.2.1.10
Figure
15-1
15.2.1.10.1
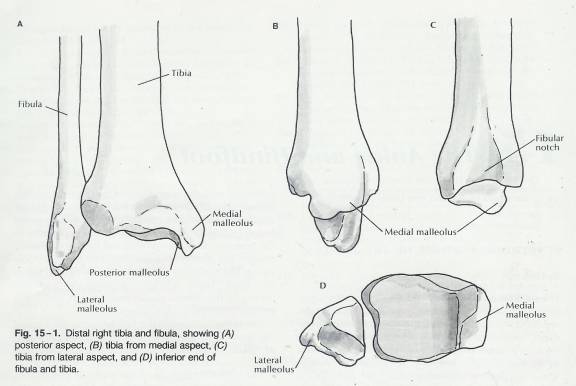
15.2.1.11
Figure
15-2
15.2.1.11.1
15.2.1.12
Figure
15-3 & 15-4
15.2.1.12.1
15.2.1.13
Figure
15-5, 6, & 7
15.2.1.13.1
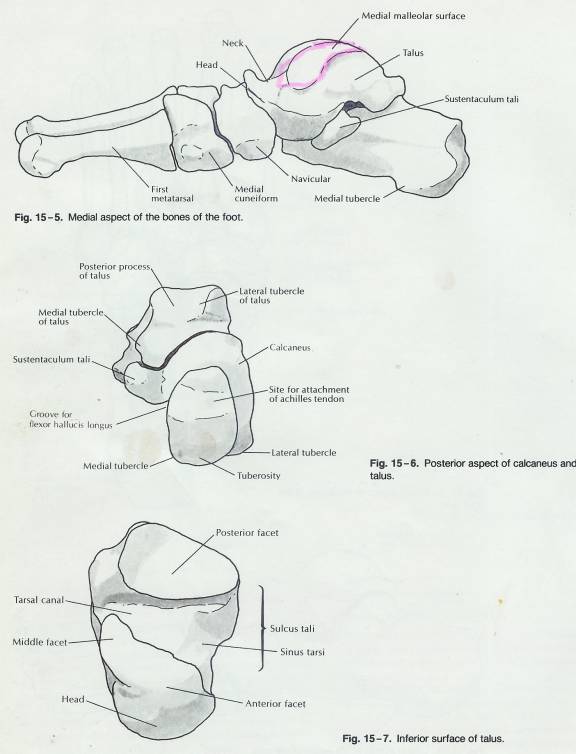
15.2.1.14 The posterior talofibular ligament attaches to the 1ateral tubercle. The medial talocalcaneal ligament and a posterior portion of the deltoid ligament attach to the medial tubercle.
15.2.1.15
The neck and head of the talus are
positioned anteriorly to the body. They are directed slightly medially and
downward with respect to the body. The head is covered with articular cartilage
anteriorly for articulation with the navicular and inferiorly for articulation
with the spring ligament (plantar calcaneonavicular ligament.
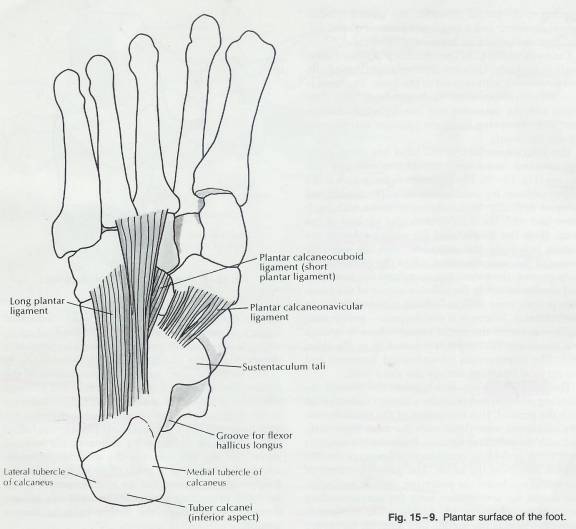
15.2.1.16 The inferior: surface of the talus has three cartilage-covered facets for articulation with the calcaneus (Fig. 15 -7). The posterior facet, which is the largest of these, is concave inferiorly. The medial and anterior articular facets are continuous with each other-and with the inferior articular surface of the head. Both the medial and the anterior facets are convex inferiorly and articulate with the superior aspect of the sustentaculum tali of the calcaneus. A deep groove, the sulcus tali, separates the posterior and medial facets on the inferior aspect of the talus. This groove runs obliquely from posteromedial to anterolateral. Where it is the deepest-posteromedially-it forms the tarsal canal; where it widens and opens out laterally it is referred to as the sinus. Tars. The interosseous talocalcaneal ligament and the cervical ligament occupy the sinus tarsi.
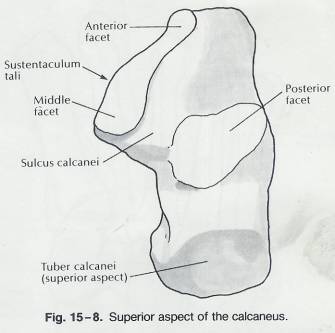
15.2.1.17 The calcaneus is situated beneath the talus in the standing position and provides a major contact point with the ground. It is the largest of the tarsal bones. The calcaneus articulates with the talus superiorly and with the cuboid anteriorly. Posteriorly it projects backward, providing considerable leverage for the plantar flexors of the ankle. The superior aspect of the calcaneus bears the posterior, medial, and anterior facets for articulation with the corresponding facets of the talus (Fig. 15 - 8). The posterior facet is convex whereas the medial and anterior facets are concave. The medial and anterior facets are situated on the superior aspect of the sustentaculum tali, which is a bony projection of the calcaneus that overhangs medially. As with the corresponding facets on the talus, the medial and anterior facets of the calcaneus are usually continuous with each other. The medial and anterior facets are separated' from the posterior facet by the sulcus calcanei, which forms the bottom of the sinus tarsi and tarsal canal, thus corresponding to the sulcus tali of the talus.
15.2.1.18 The posterior aspect of the large posterior projection of the calcaneus contains a smooth superior surface, which slopes upward and forward, and a rough inferior surface, which slopes downward and forward.
15.2.1.19
Figure
15-8
15.2.1.19.1
15.2.1.20
The upper surface is the site of
attachment for the Achilles tendon (see Fig. 15 - 6). The lower surface Blends
inferiorly with the tuber calcanei, which is the point of contact of the
calcaneus with the
ground in the standing position.
15.2.1.21 The tuber calcanei on the inferior aspect of the" calcaneus consists of a medial tubercle and a lateral tubercle, of which the is the larger. Anterior to the tuber calcanei is a roughened surface for the attachment of the long and short plantar ligaments (Fig. 15-9). At the anterior extent of the inferior surface of the calcaneus is the anterior tubercle, which also serves as a point of attachment for the long plantar ligament. On the inferior aspect of the medially projecting sustentaculum tali is a groove through which runs the flexor hallucis .longus tendon.
15.2.1.22 The lateral aspect of the calcaneus is nearly flat. There is a small prominence, the peroneal trochlea that is located just distal to the lateral malleolus (see Fig. 15 - 4). The peroneus brevis tendon travels downward and forward, just superior to this trochlea: while the peroneus longus tendon passes inferior to it. The calcaneofibular ligament attaches just posterior and slightly superior to the peroneal trochlea, at which point there may be a rounded prominence.
15.2.1.23 From the anterosuperior extent of the medial aspect of the calcaneus, the sustentaculum tali projects in a medial direction (see Fig. 15-8) The sustentaculum tali may be palpated just below the medial malleolus. .
15.2.1.24
Figure
15-9
15.2.1.24.1
15.2.1.25 On the narrowed anterior aspect of the calcaneus is the cartage-covered articular surface. that contacts the cuboid bone. This is a sellar joint surface, being concave, superoinferiorly and convex mediolaterally (see Fig. 15-3).
15.2.1.26 The remainder of the tarsus includes the navicular and cuboid bones, which contact the talus and calcaneus, respectively, and the three cuneiforms, which articulate with the first three metatarsals (Fig. 15-3). The cuboid extends distally to contact the remaining two metatarsals. (These bones will not be considered in detail here but will be referred to in the biomechanics section of this chapter).
15.2.2
Tarsals,
Metatarsals, and Phalanges
15.2.2.1
Tarsus
(Tarsals) (7) (tahr’sus)
15.2.2.1.1
The tarsus is
a collective designation for the seven bones of the ankle called tarsals. The
term tarsos pertains to a broad, flat surface.
15.2.2.1.2
Posterior
Tarsus
15.2.2.1.2.1 Talus (astragalus; ankle bone)
15.2.2.1.2.1.1
Summary
15.2.2.1.2.1.1.1
The talus, the uppermost
tarsal bone, is the only bone of the foot that articulates with the fibula and
tibia.
15.2.2.1.2.1.1.2
It is
surrounded on one side by the medial Malleolus of the tibia and on the other
side by the lateral Malleolus of the fibula.
15.2.2.1.2.1.1.3
During walking,
the talus initially bears the entire weight of the body. About half the weight
is then transmitted to the calcaneus. The remainder is transmitted to the other
tarsal bones.
15.2.2.1.2.1.2
Detailed
Description of Osseous Structure
15.2.2.1.2.1.2.1
The talus is
the second largest of the tarsal bones. It occupies the middle and upper part
of the tarsus, supporting the tibia above, resting upon the calcaneus below,
articulating on either side with the malleoli, and in front with the navicular.
It consists of a body, a neck, and a head.
15.2.2.1.2.1.2.2
The Body
(corpus tali)
15.2.2.1.2.1.2.2.1 The superior surface of the body presents, behind, a smooth trochlear surface, the trochlea, for articulation with the tibia. The trochlea is broader in front than behind, convex from before backward, slightly concave from side to side: in front it is continuous with the upper surface of the neck of the bone. The inferior surface presents two articular areas, the posterior and middle calcaneal surfaces, separated from one another by a deep groove, the sulcus tali. The groove runs obliquely forward and lateralward, becoming gradually broader and deeper in front: in the articulated foot it lies above a similar groove upon the upper surface of the calcaneus, and forms, with it, a canal (sinus tarsi) filled up in the fresh state by the interosseous talocalcaneal ligament. The posterior calcaneal articular surface is large and of an oval or oblong form. It articulates with the corresponding facet on the upper surface of the calcaneus, and is deeply concave in the direction of its long axis which runs forward and lateralward at an angle of about 45° with the median plane of the body. The middle calcaneal articular surface is small, oval in form and slightly convex; it articulates with the upper surface of the sustentaculum tali of the calcaneus. The medial surface presents at its upper part a pear-shaped articular facet for the medial malleolus, continuous above with the trochlea; below the articular surface is a rough depression for the attachment of the deep portion of the deltoid ligament of the ankle-joint. The lateral surface carries a large triangular facet, concave from above downward, for articulation with the lateral malleolus; its anterior half is continuous above with the trochlea; and in front of it is a rough depression for the attachment of the anterior talofibular ligament. Between the posterior half of the lateral border of the trochlea and the posterior part of the base of the fibular articular surface is a triangular facet, which comes into contact with the transverse inferior tibiofibular ligament during flexion of the ankle-joint; below the base of this facet is a groove, which affords attachment to the posterior talofibular ligament.
15.2.2.1.2.1.2.2.2
The posterior surface is narrow, and
traversed by a groove running obliquely downward and medialward, and transmitting
the tendon of the Flexor hallucis longus. Lateral to the groove is a prominent
tubercle, the posterior process, to which the posterior talofibular ligament is
attached; this process is sometimes separated from the rest of the talus, and
is then known as the os trigonum. Medial to the groove is a second smaller
tubercle.
15.2.2.1.2.1.2.3
The Neck
(collum tali)
15.2.2.1.2.1.2.3.1 The neck is directed forward and medialward, and comprises the constricted portion of the bone between the body and the oval head. Its upper and medial surfaces are rough, for the attachment of ligaments; its lateral surface is concave and is continuous below with the deep groove for the interosseous talocalcaneal ligament.
15.2.2.1.2.1.2.4 The Head (caput tali)
15.2.2.1.2.1.2.4.1 The head looks forward and medialward; its anterior articular or navicular surface is large, oval, and convex. Its inferior surface has two facets, which are best seen in the fresh condition. The medial, situated in front of the middle calcaneal facet, is convex, triangular, or semi-oval in shape, and rests on the plantar calcaneonavicular ligament; the lateral, named the anterior calcaneal articular surface, is somewhat flattened, and articulates with the facet on the upper surface of the anterior part of the calcaneus.
15.2.2.1.2.1.2.5
Articulations.
15.2.2.1.2.1.2.5.1 The talus articulates with four bones: tibia, fibula, calcaneus, and navicular.
15.2.2.1.2.2 Calcaneus (kal-KĀ-nē-us) (os calcis)
15.2.2.1.2.2.1
Summary
15.2.2.1.2.2.1.1
The calcaneus,
or heel bone, is the largest and strongest tarsal bone.
15.2.2.1.2.2.2
Detailed
Description of Osseous Structure
15.2.2.1.2.2.2.1
Introduction
15.2.2.1.2.2.2.1.1 The calcaneus is the largest of the tarsal bones. It is situated at the lower and back part of the foot, serving to transmit the weight of the body to the ground, and forming a strong lever for the muscles of the calf. It is irregularly cuboidal in form, having its long axis directed forward and lateralward; it presents for examination six surfaces.
15.2.2.1.2.2.2.2
Surfaces
15.2.2.1.2.2.2.2.1 Superior Surface
1.1.1.1.1.1.1.1.1 The superior surface extends behind on to that part of the bone which projects backward to form the heel. This varies in length in different individuals, is convex from side to side, concave from before backward, and supports a mass of fat placed in front of the tendo calcaneus. In front of this area is a large usually somewhat oval-shaped facet, the posterior articular surface, which looks upward and forward; it is convex from behind forward, and articulates with the posterior calcaneal facet on the under surface of the talus. It is bounded anteriorly by a deep depression which is continued backward and medialward in the form of a groove, the calcaneal sulcus. In the articulated foot this sulcus lies below a similar one on the under surface of the talus, and the two form a canal (sinus tarsi) for the lodgment of the interosseous talocalcaneal ligament. In front and to the medial side of this groove is an elongated facet, concave from behind forward, and with its long axis directed forward and lateralward. This facet is frequently divided into two by a notch: of the two, the posterior, and larger is termed the middle articular surface; it is supported on a projecting process of bone, the sustentaculum tali, and articulates with the middle calcaneal facet on the under surface of the talus; the anterior articular surface is placed on the anterior part of the body, and articulates with the anterior calcaneal facet on the talus. The upper surface, anterior and lateral to the facets, is rough for the attachment of ligaments and for the origin of the Extensor digitorum brevis.
15.2.2.1.2.2.2.2.2 Inferior or Plantar surface
1.1.1.1.1.1.1.1.2 The inferior or plantar surface is uneven, wider behind than in front, and convex from side to side; it is bounded posteriorly by a transverse elevation, the calcaneal tuberosity, which is depressed in the middle and prolonged at either end into a process; the lateral process, small, prominent, and rounded, gives origin to part of the Abductor digiti quinti; the medial process, broader and larger, gives attachment, by its prominent medial margin, to the Abductor hallucis, and in front to the Flexor digitorum brevis and the plantar aponeurosis; the depression between the processes gives origin to the Abductor digiti quinti. The rough surface in front of the processes gives attachment to the long plantar ligament, and to the lateral head of the Quadratus plantae while to a prominent tubercle nearer the anterior part of this surface, as well as to a transverse groove in front of the tubercle, is attached the plantar calcaneocuboid ligament. The lateral surface is broad behind and narrow in front, flat and almost subcutaneous; near its center is a tubercle, for the attachment of the calcaneofibular ligament. At its upper and anterior part, this surface gives attachment to the lateral talocalcaneal ligament; and in front of the tubercle it presents a narrow surface marked by two oblique grooves. The grooves are separated by an elevated ridge, or tubercle, the trochlear process (peroneal tubercle), which varies much in size in different bones. The superior groove transmits the tendon of the Peroneus brevis; the inferior groove, that of the Peroneus longus.
15.2.2.1.2.2.2.2.3 Medial Surface
1.1.1.1.1.1.1.1.3 The medial surface is deeply concave; it is directed obliquely downward and forward, and serves for the transmission of the plantar vessels and nerves into the sole of the foot; it affords origin to part of the Quadratus plantae. At its upper and forepart is a horizontal eminence, the sustentaculum tali, which gives attachment to a slip of the tendon of the Tibialis posterior. This eminence is concave above, and articulates with the middle calcaneal articular surface of the talus; below, it is grooved for the tendon of the Flexor hallucis longus; its anterior margin gives attachment to the plantar calcaneonavicular ligament, and its medial, to a part of the deltoid ligament of the ankle-joint. The anterior or cuboid articular surface is of a somewhat triangular form. It is concave from above downward and lateralward, and convex in a direction at right angles to this. Its medial border gives attachment to the plantar calcaneonavicular ligament. The posterior surface is prominent, convex, wider below than above, and divisible into three areas. The lowest of these is rough, and covered by the fatty and fibrous tissue of the heel; the middle, also rough, gives insertion to the tendo calcaneus and Plantaris; while the highest is smooth, and is covered by a bursa which intervenes between it and the tendo calcaneus.
15.2.2.1.2.2.2.2.4 Articulations
1.1.1.1.1.1.1.1.4 The calcaneus articulates with two bones: the talus and cuboid.
15.2.2.1.3
Anterior
Tarsus
15.2.2.1.3.1 The anterior part contains the cuboid, Navicular, and three cuneiform (cuneiform=wedge-shaped) bones called the first (medial), second (intermediate), and third (lateral) cuneiform.
15.2.2.1.3.2 Cuboid Bone (os cuboideum)
15.2.2.1.3.2.1 Introduction
15.2.2.1.3.2.1.1 The cuboid bone is placed on the lateral side of the foot, in front of the calcaneus, and behind the fourth and fifth metatarsal bones. It is of a pyramidal shape, its base being directed medialward.
15.2.2.1.3.2.2 Surfaces
15.2.2.1.3.2.2.1 Dorsal Surface
15.2.2.1.3.2.2.1.1 The dorsal surface, directed upward and lateralward, is rough, for the attachment of ligaments.
15.2.2.1.3.2.2.2 Plantar Surface
15.2.2.1.3.2.2.2.1 The plantar surface presents in front a deep groove, the peroneal sulcus, which runs obliquely forward and medialward; it lodges the tendon of the Peroneus longus, and is bounded behind by a prominent ridge, to which the long plantar ligament is attached. The ridge ends laterally in an eminence, the tuberosity, the surface of which presents an oval facet; on this facet glides the sesamoid bone or cartilage frequently found in the tendon of the Peroneus longus. The surface of bone behind the groove is rough, for the attachment of the plantar calcaneocuboid ligament, a few fibers of the Flexor hallucis brevis, and a fasciculus from the tendon of the Tibialis posterior.
15.2.2.1.3.2.2.3 Lateral Surface
15.2.2.1.3.2.2.3.1 The lateral surface presents a deep notch formed by the commencement of the peroneal sulcus.
15.2.2.1.3.2.2.4 Posterior Surface
15.2.2.1.3.2.2.4.1 The posterior surface is smooth, triangular, and concavo-convex, for articulation with the anterior surface of the calcaneus; its inferior-medial angle projects backward as a process, which underlies and supports the anterior end of the calcaneus.
15.2.2.1.3.2.2.5 Anterior Surface
15.2.2.1.3.2.2.5.1 The anterior surface, of smaller size, but also irregularly triangular, is divided by a vertical ridge into two facets: the medial, quadrilateral in form, articulates with the fourth metatarsal; the lateral, larger and more triangular, articulates with the fifth.
15.2.2.1.3.2.2.6 Medial Surface
15.2.2.1.3.2.2.6.1 The medial surface is broad, irregularly quadrilateral, and presents at its middle and upper part a smooth oval facet, for articulation with the third cuneiform; and behind this (occasionally) a smaller facet, for articulation with the navicular; it is rough in the rest of its extent, for the attachment of strong interosseous ligaments.
15.2.2.1.3.2.2.7 Articulations
15.2.2.1.3.2.2.7.1 The cuboid articulates with four bones: the calcaneus, third cuneiform, and fourth and fifth metatarsals; occasionally with a fifth, the navicular.
15.2.2.1.3.3 Navicular Bone (os naviculare pedis; scaphoid bone)
15.2.2.1.3.3.1 Summary
15.2.2.1.3.3.1.1 The navicular bone is situated at the medial side of the tarsus, between the talus behind and the cuneiform bones in front.
15.2.2.1.3.3.2 Surfaces
15.2.2.1.3.3.2.1 Anterior Surface
15.2.2.1.3.3.2.1.1 The anterior surface is convex from side to side, and subdivided by two ridges into three facets, for articulation with the three cuneiform bones.
15.2.2.1.3.3.2.2 Posterior Surface
15.2.2.1.3.3.2.2.1 The posterior surface is oval, concave, broader laterally than medially, and articulates with the rounded head of the talus.
15.2.2.1.3.3.2.3 Dorsal Surface
15.2.2.1.3.3.2.3.1 The dorsal surface is convex from side to side, and rough for the attachment of ligaments.
15.2.2.1.3.3.2.4 Plantar Surface
15.2.2.1.3.3.2.4.1 The plantar surface is irregular, and also rough for the attachment of ligaments.
15.2.2.1.3.3.2.5 Medial Surface
15.2.2.1.3.3.2.5.1 The medial surface presents a rounded tuberosity, the lower part of which gives attachment to part of the tendon of the Tibialis posterior.
15.2.2.1.3.3.2.6 Lateral Surface
15.2.2.1.3.3.2.6.1 The lateral surface is rough and irregular for the attachment of ligaments, and occasionally presents a small facet for articulation with the cuboid bone.
15.2.2.1.3.3.3 Articulations
15.2.2.1.3.3.3.1 The navicular articulates with four bones: the talus and the three cuneiforms; occasionally with a fifth, the cuboid.
15.2.2.1.3.4 The First Cuneiform Bone (os cuneiform primum; internalcuneiform)
15.2.2.1.3.4.1 Summary
15.2.2.1.3.4.1.1 The first cuneiform bone is the largest of the three cuneiforms. It is situated at the medial side of the foot, between the navicular behind and the base of the first metatarsal in front.
15.2.2.1.3.4.2 Surfaces
15.2.2.1.3.4.2.1 Medial Surface
15.2.2.1.3.4.2.1.1 The medial surface is subcutaneous, broad, and quadrilateral; at its anterior plantar angle is a smooth oval impression, into which part of the tendon of the Tibialis anterior is inserted; in the rest of its extent it is rough for the attachment of ligaments.
15.2.2.1.3.4.2.2 Lateral Surface
15.2.2.1.3.4.2.2.1 The lateral surface is concave, presenting, along its superior and posterior borders a narrow L-shaped surface, the vertical limb and posterior part of the horizontal limb of which articulate with the second cuneiform, while the anterior part of the horizontal limb articulates with the second metatarsal bone: the rest of this surface is rough for the attachment of ligaments and part of the tendon of the Peroneus longus.
15.2.2.1.3.4.2.3 Anterior Surface
15.2.2.1.3.4.2.3.1 The anterior surface, kidney-shaped and much larger than the posterior, articulates with the first metatarsal bone.
15.2.2.1.3.4.2.4 Posterior Surface
15.2.2.1.3.4.2.4.1 The posterior surface is triangular, concave, and articulates with the most medial and largest of the three facets on the anterior surface of the navicular.
15.2.2.1.3.4.2.5 Plantar Surface
15.2.2.1.3.4.2.5.1 The plantar surface is rough, and forms the base of the wedge; at its back part is a tuberosity for the insertion of part of the tendon of the Tibialis posterior. It also gives insertion in front to part of the tendon of the Tibialis anterior.
15.2.2.1.3.4.2.6 Dorsal Surface
15.2.2.1.3.4.2.6.1 The dorsal surface is the narrow end of the wedge, and is directed upward and lateralward; it is rough for the attachment of ligaments.
15.2.2.1.3.4.3 Articulations
15.2.2.1.3.4.3.1 The first cuneiform articulates with four bones: the navicular, second cuneiform, and first and second metatarsals.
15.2.2.1.3.5 Second Cuneiform Bone (os cuneiforme secundum; middle cuneiform)
15.2.2.1.3.5.1 Summary
15.2.2.1.3.5.1.1 The second cuneiform bone, the smallest of the three, is of very regular wedge-like form, the thin end being directed downward. It is situated between the other two cuneiforms, and articulates with the navicular behind, and the second metatarsal in front.
15.2.2.1.3.5.2 Surfaces
15.2.2.1.3.5.2.1 Anterior Surface
15.2.2.1.3.5.2.1.1 The anterior surface, triangular in form, and narrower than the posterior, articulates with the base of the second metatarsal bone.
15.2.2.1.3.5.2.2 Posterior Surface
15.2.2.1.3.5.2.2.1 The posterior surface, also triangular, articulates with the intermediate facet on the anterior surface of the navicular.
15.2.2.1.3.5.2.3 Medial Surface
15.2.2.1.3.5.2.3.1 The medial surface carries an L-shaped articular facet, running along the superior and posterior borders, for articulation with the first cuneiform, and is rough in the rest of its extent for the attachment of ligaments.
15.2.2.1.3.5.2.4 Lateral Surface
15.2.2.1.3.5.2.4.1 The lateral surface presents posteriorly a smooth facet for articulation with the third cuneiform bone.
15.2.2.1.3.5.2.5 Dorsal Surface
15.2.2.1.3.5.2.5.1 The dorsal surface forms the base of the wedge; it is quadrilateral and rough for the attachment of ligaments.
15.2.2.1.3.5.2.6 Plantar Surface
15.2.2.1.3.5.2.6.1 The plantar surface, sharp and tuberculated, is also rough for the attachment of ligaments, and for the insertion of a slip from the tendon of the Tibialis posterior.
15.2.2.1.3.5.3 Articulations
15.2.2.1.3.5.3.1 The second cuneiform articulates with four bones: the navicular, first and third cuneiforms, and second metatarsal.
15.2.2.1.3.6 Third Cuneiform Bone (os cuneiforme tertium; external cuneiform)
15.2.2.1.3.6.1 Summary
15.2.2.1.3.6.1.1 The third cuneiform bone, intermediate in size between the two preceding, is wedge-shaped, the base being uppermost. It occupies the center of the front row of the tarsal bones, between the second cuneiform medially, the cuboid laterally, the navicular behind, and the third metatarsal in front.
15.2.2.1.3.6.2 Surfaces
15.2.2.1.3.6.2.1 Anterior Surface
15.2.2.1.3.6.2.1.1 The anterior surface, triangular in form, articulates with the third metatarsal bone. The posterior surface articulates with the lateral facet on the anterior surface of the navicular, and is rough below for the attachment of ligamentous fibers.
15.2.2.1.3.6.2.2 Medial Surface
15.2.2.1.3.6.2.2.1 The medial surface presents an anterior and a posterior articular facet, separated by a rough depression: the anterior, sometimes divided, articulates with the lateral side of the base of the second metatarsal bone; the posterior skirts the posterior border, and articulates with the second cuneiform; the rough depression gives attachment to an interosseous ligament.
15.2.2.1.3.6.2.3 Lateral Surface
15.2.2.1.3.6.2.3.1 The lateral surface also presents two articular facets, separated by a rough non-articular area; the anterior facet, situated at the superior angle of the bone, is small and semi-oval in shape, and articulates with the medial side of the base of the fourth metatarsal bone; the posterior and larger one is triangular or oval, and articulates with the cuboid; the rough, non-articular area serves for the attachment of an interosseous ligament. The three facets for articulation with the three metatarsal bones are continuous with one another; those for articulation with the second cuneiform and navicular are also continuous, but that for articulation with the cuboid is usually separate.
15.2.2.1.3.6.2.4 Dorsal Surface
15.2.2.1.3.6.2.4.1 The dorsal surface is of an oblong form, its posterior-lateral angle being prolonged backward.
15.2.2.1.3.6.2.5 Plantar Surface
15.2.2.1.3.6.2.5.1 The plantar surface is a rounded margin, and serves for the attachment of part of the tendon of the Tibialis posterior, part of the Flexor hallucis brevis, and ligaments.
15.2.2.1.3.6.3 Articulations
15.2.2.1.3.6.3.1 The third cuneiform articulates with six bones: the navicular, second cuneiform, cuboid, and second, third, and fourth metatarsals.
15.2.2.2
Metatarsus
(5)
15.2.2.2.1
Summary
15.2.2.2.1.1 The metatarsus consists of five metatarsal bones numbered 1-5 from the medial to lateral position.
15.2.2.2.1.2 Like the metacarpals of the palm of the hand, each metatarsal consists of a proximal base, a shaft, with a distal head.
15.2.2.2.1.3 The metatarsals articulate proximally with the first, second and third cuneiform bones and with the cuboid.
15.2.2.2.1.4 Distally, they articulate with the proximal row of phalanges.
15.2.2.2.1.5 The first metatarsal is thicker than the others because it bears more weight.
15.2.2.2.2
Detailed
Description
15.2.2.2.2.1 Introduction
15.2.2.2.2.1.1 The metatarsus consists of five bones which are numbered from the medial side (ossa metatarsalia I.-V.); each presents for examination a body and two extremities.
15.2.2.2.2.2 Common Characteristics of the Metatarsal Bones
15.2.2.2.2.2.1 The body is prismoid in form, tapers gradually from the tarsal to the phalangeal extremity, and is curved longitudinally, so as to be concave below, slightly convex above.
15.2.2.2.2.2.2 Base or Posterior Extremity
15.2.2.2.2.2.2.1 The base or posterior extremity is wedge-shaped, articulating proximally with the tarsal bones, and by its sides with the contiguous metatarsal bones: its dorsal and plantar surfaces are rough for the attachment of ligaments.
15.2.2.2.2.2.3 Head or Anterior Extremity
15.2.2.2.2.2.3.1 The head or anterior extremity presents a convex articular surface, oblong from above downward, and extending farther backward below than above. Its sides are flattened, and on each is a depression, surmounted by a tubercle, for ligamentous attachment. Its plantar surface is grooved anterior-posteriorly for the passage of the Flexor tendons, and marked on either side by an articular eminence continuous with the terminal articular surface.
15.2.2.2.2.2.4 Characteristics of the Individual Metatarsal Bones
15.2.2.2.2.2.4.1 The First Metatarsal Bone (os metatarsale I; metatarsal bone of the great toe)
15.2.2.2.2.2.4.1.1 The first metatarsal bone is remarkable for its great thickness, and is the shortest of the metatarsal bones. The body is strong, and of well-marked prismoid form. The base presents, as a rule, no articular facets on its sides, but occasionally on the lateral side there is an oval facet, by which it articulates with the second metatarsal. Its proximal articular surface is of large size and kidney-shaped; its circumference is grooved, for the tarsometatarsal ligaments, and medially gives insertion to part of the tendon of the Tibialis anterior; its plantar angle presents a rough oval prominence for the insertion of the tendon of the Peronæus longus. The head is large; on its plantar surface are two grooved facets, on which glide sesamoid bones; the facets are separated by a smooth elevation.
15.2.2.2.2.2.4.2 The Second Metatarsal Bone (os metatarsale II)
15.2.2.2.2.2.4.2.1 The second metatarsal bone is the longest of the metatarsal bones, being prolonged backward into the recess formed by the three cuneiform bones. Its base is broad above, narrow and rough below. It presents four articular surfaces: one behind, of a triangular form, for articulation with the second cuneiform; one at the upper part of its medial surface, for articulation with the first cuneiform; and two on its lateral surface, an upper and lower, separated by a rough non-articular interval. Each of these lateral articular surfaces is divided into two by a vertical ridge; the two anterior facets articulate with the third metatarsal; the two posterior (sometimes continuous) with the third cuneiform. A fifth facet is occasionally present for articulation with the first metatarsal; it is oval in shape, and is situated on the medial side of the body near the base.
15.2.2.2.2.2.4.3 The Third Metatarsal Bone (os metatarsale III)
15.2.2.2.2.2.4.3.1 The third metatarsal bone articulates proximally, by means of a triangular smooth surface, with the third cuneiform; medially, by two facets, with the second metatarsal; and laterally, by a single facet, with the fourth metatarsal. This last facet is situated at the dorsal angle of the base.
15.2.2.2.2.2.4.4 The Fourth Metatarsal Bone (os metatarsale IV)
15.2.2.2.2.2.4.4.1 The fourth metatarsal bone is smaller in size than the preceding; its base presents an oblique quadrilateral surface for articulation with the cuboid; a smooth facet on the medial side, divided by a ridge into an anterior portion for articulation with the third metatarsal, and a posterior portion for articulation with the third cuneiform; on the lateral side a single facet, for articulation with the fifth metatarsal.
15.2.2.2.2.2.4.5 The Fifth Metatarsal Bone (os metatarsale V)
15.2.2.2.2.2.4.5.1 The fifth metatarsal bone is recognized by a rough eminence, the tuberosity, on the lateral side of its base. The base articulates behind, by a triangular surface cut obliquely in a transverse direction, with the cuboid; and medially, with the fourth metatarsal. On the medial part of its dorsal surface is inserted the tendon of the Peroneus Tertius and on the dorsal surface of the tuberosity that of the Peroneus brevis. A strong band of the plantar aponeurosis connects the projecting part of the tuberosity with the lateral process of the tuberosity of the calcaneus. The plantar surface of the base is grooved for the tendon of the Abductor digiti quinti, and gives origin to the Flexor digiti quinti brevis.
15.2.2.2.2.3 Articulations
15.2.2.2.2.3.1 The base of each metatarsal bone articulates with one or more of the tarsal bones, and the head with one of the first row of phalanges. The first metatarsal articulates with the first cuneiform, the second with all three cuneiforms, the third with the third cuneiform, the fourth with the third cuneiform and the cuboid, and the fifth with the cuboid.
15.2.2.3
Phalanges
(14)
15.2.2.3.1
Summary
15.2.2.3.1.1 The phalanges of the foot resemble those of the hand both in number and arrangement. Each also consists of a proximal base, a middle shaft, and a distal head.
15.2.2.3.1.2 The Hallux (great or big toe), has two large, heavy phalanges called proximal and distal phalanges.
15.2.2.3.1.3 The other four toes each have three phalanges, proximal, middle, and distal.
15.2.2.3.2
Detailed
Description
15.2.2.3.2.1 Introduction
15.2.2.3.2.1.1 The phalanges of the foot correspond, in number and general arrangement, with those of the hand; there are two in the great toe, and three in each of the other toes. They differ from them, however, in their size, the bodies being much reduced in length, and, especially in the first row, laterally compressed.
15.2.2.3.2.2 First Row
15.2.2.3.2.2.1 The body of each is compressed from side to side, convex above, concave below. The base is concave; and the head presents a trochlear surface for articulation with the second phalanx.
15.2.2.3.2.3 Second Row
15.2.2.3.2.3.1 The phalanges of the second row are remarkably small and short, but rather broader than those of the first row.
15.2.2.3.2.4 The ungual phalanges
15.2.2.3.2.4.1 The ungual phalanges, in form, resemble those of the fingers; but they are smaller and are flattened from above downward; each presents a broad base for articulation with the corresponding bone of the second row, and an expanded distal extremity for the support of the nail and end of the toe.
15.2.2.3.2.5 Articulations
15.2.2.3.2.5.1 In the second, third, fourth, and fifth toes the phalanges of the first row articulate behind with the metatarsal bones, and in front with the second phalanges, which in their turn articulate with the first and third: the ungual phalanges articulate with the second.
15.2.2.4
Total
Bones of Foot=26
15.2.3
Arches
of the Foot
15.2.3.1
The
bones of the foot are arranged in two arches. These arches enable the foot to
support the weight of the body, provide an ideal distribution of body weight
over the hard and soft tissues of the foot, and provide leverage while walking.
15.2.3.2
While
these medial and lateral arches may be readily demonstrated as the component
antero-posterior arches of the foot, yet the fundamental longitudinal arch is
contributed to by both, and consists of the calcaneus, cuboid, third cuneiform,
and third metatarsal: all the other bones of the foot may be removed without
destroying this arch.
15.2.3.3
The
arches are not rigid. They yield as weight is applied and spring back when the
weight is lifted, thus helping to absorb shocks.
15.2.3.4
Longitudinal
Arch
15.2.3.4.1
The
longitudinal arch has two parts. Both consist of tarsal and metatarsal bones
arranged to form an arch from the anterior to the posterior part of the foot.
15.2.3.4.1.1 Medial Longitudinal Arch
15.2.3.4.1.1.1 Originates at the calcaneus, rises to the talus and descends through the Navicular, the three cuneiforms, and the heads of the three medial metatarsals.
15.2.3.4.1.1.2 The talus is the keystone of the arch.
15.2.3.4.1.1.3 Its summit is at the superior articular surface of the talus, and its two extremities or piers, on which it rests in standing, are the tuberosity on the plantar surface of the calcaneus posteriorly and the heads of the first, second, and third metatarsal bones anteriorly.
15.2.3.4.1.1.4 The chief characteristic of this arch is its elasticity, due to its height and to the number of small joints between its component parts.
15.2.3.4.1.1.5 Its weakest part, i. e., the part most liable to yield from overpressure, is the joint between the talus and Navicular, but this portion is braced by the plantar calcaneonavicular ligament, which is elastic and is thus able to quickly restore the arch to its pristine condition when the disturbing force is removed.
15.2.3.4.1.1.6 The ligament is strengthened medially by blending with the deltoid ligament of the ankle-joint, and is supported inferiorly by the tendon of the Tibialis posterior, which is spread out in a fan shaped insertion and prevents undue tension of the ligament or such an amount of stretching as would permanently elongate it.
15.2.3.4.1.1.7 The arch is further supported by the plantar aponeurosis, by the small muscles in the sole of the foot, by the tendons of the Tibialis anterior and posterior and Peronæus longus, and by the ligaments of all the articulations involved.
15.2.3.4.1.2 Lateral Longitudinal Arch
15.2.3.4.1.2.1 Begins at the calcaneus, rises at the cuboid and descends to the heads of the two lateral metatarsals.
15.2.3.4.1.2.2 The cuboid is the keystone of this arch.
15.2.3.4.1.2.3 The calcaneocuboid, possesses a special mechanism for locking, and allows only a limited movement
15.2.3.4.1.2.4 The most marked features of this arch are its solidity and its slight elevation; two strong ligaments, the long plantar and the plantar calcaneocuboid, together with the Extensor tendons and the short muscles of the little toe, preserve its integrity.
15.2.3.4.2
Transverse
Arch
15.2.3.4.2.1 The Navicular, three cuneiforms, cuboid, and the bases of the five metatarsals form the transverse arch.
15.2.3.4.2.2 At the posterior part of the metatarsus and the anterior part of the tarsus the arches are complete, but in the middle of the tarsus they present more the characters of half-domes the concavities of which are directed downward and medial ward, so that when the medial borders of the feet are placed in apposition a complete tarsal dome is formed.
15.2.3.4.2.3 The transverse arches are strengthened by the interosseous, plantar, and dorsal ligaments, by the short muscles of the first and fifth toes (especially the transverse head of the Adductor hallucis), and by the Peroneus longus, whose tendon stretches across between the piers of the arches.
15.2.4
15.3 Arthrology
15.3.1 Tibiofibular Joint
15.3.1.1 Summary
15.3.1.1.1 The superior and inferior tibiofibular joints are separate from the ankle joint but must provide accessory movements for full ankle function.
15.3.1.1.2 The superior Tibiofibular is formed between the proximal ends of the tibia and fibula when the fibular head joins with a facet on the Posterolateral aspect of the rim of the tibial condyle forming a plane synovial joint.
15.3.1.1.3 The inferior Tibiofibular joint is formed between the distal ends of the tibia and fibula forming a Syndesmosis with fibroadipose tissue, and bound together by the Crural Tibiofibular interosseous ligament and the anterior and posterior Tibiofibular ligaments.
15.3.1.1.4 With Dorsiflexion, plantarflexion, inversion, and Eversion there are slight accessory movements of the fibula.
15.3.1.2 Introduction
15.3.1.2.1 Anatomically, the superior and inferior tibiofibular joints are separate from the ankle but provide accessory motions, which allow greater movement at the ankle, fusion or immobility in these joint may impair ankle function.
15.3.1.3 Superior Tibiofibular Joint
15.3.1.3.1 Definition
15.3.1.3.1.1 This joint is formed between the proximal ends of the tibia and fibula
15.3.1.3.1.2 The fibular head joins with a facet on the Posterolateral aspect of the rim of the tibial condyle; the facet faces posteriorly, inferiorly, and laterally.
15.3.1.3.2 Type of Joint
15.3.1.3.2.1 Plane synovial joint
15.3.1.4 Inferior Tibiofibular Joint
15.3.1.4.1 Discussion
15.3.1.4.1.1 The inferior tibiofibular joint is a Syndesmosis and lacks articular cartilage and synovium. The distal fibula is situated in the fibular notch of the lateral aspect of the distal tibia and is bound to it by several ligaments (Figs. 15-10 and 15-11). The anterior and posterior tibiofibular ligaments pass in front of and behind the Syndesmosis. They are both directed downward and inward to check separation of the two bones. The inferior transverse ligament is a thickened band of fibers that is closely related to the posterior tibiofibular ligament. It passes from the posterior margin of the inferior tibial articular surface downward and laterally to the malleolar fossa of the fibula. This ligament is lined inferiorly with articular cartilage where it contacts the posterolateral talar articular surface during extreme plantar flexion. The interosseous ligament is a continuation of the interosseous membrane of the tibia and fibula. It extends between the adjacent surfaces of the bones at the Syndesmosis. The tibia and fibula are separated at the syndesmosis by a fat pad.
15.3.1.4.1.2 The ligaments of the inferior tibiofibular articulation are oriented to prevent widening of the mortise. They are also important in preventing posterior displacement of the fibula at the syndesmosis, which tends to occur when the leg is forcibly internally rotated on the tarsus. It should be realized that complete sectioning of the inferior tibiofibular ligaments alone allows only a minimal increase in. the intermalleolar space. This is because the two bones are indirectly held together by their mutual connections to the talus, by way of the medial and lateral ligaments of the ankle. Significant diastasis, then, is usually accompanied by rupture of one or more of the Talocrural ligaments, usually the deltoid ligament.
15.3.1.4.1.3 Figure 15-10-11
15.3.1.4.1.3.1
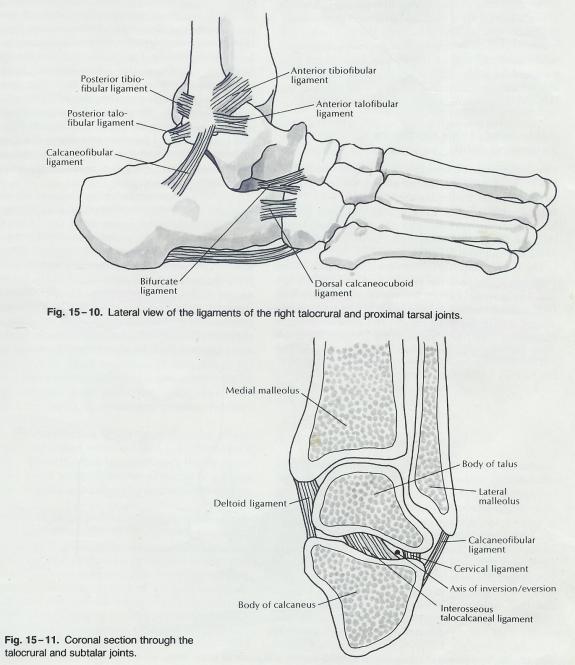
15.3.1.4.2 Definition
15.3.1.4.2.1 This joint is formed between the distal ends of the tibia and fibula
15.3.1.4.3 Type of Joint
15.3.1.4.3.1 Syndesmosis with fibroadipose tissue between the two bony surfaces
15.3.1.4.4 Ligaments
15.3.1.4.4.1 Crural Tibiofibular Interosseous Ligament
15.3.1.4.4.2 Anterior and Posterior Tibiofibular ligaments
15.3.1.5 Movements
15.3.1.5.1 With Dorsiflexion and plantarflexion of the ankle, there are slight accessory movements of the fibula
15.3.1.5.1.1 Plantar Flexion & Dorsiflexion
15.3.1.5.1.2 As the ankle plantarflexes, the lateral Malleolus (fibula) rotates medially and is pulled inferiorly, and the two malleoli approximate.
15.3.1.5.1.3 At the superior joint, the fibula slides inferiorly
15.3.1.5.1.4 The opposite occurs with Dorsiflexion
15.3.1.5.1.5 Supination and Inversion
15.3.1.5.1.6 As the ankle supinates and inverts, the head of the fibula slides distally and posteriorly (external rotation)
15.3.1.5.1.7 Pronation and Eversion
15.3.1.5.1.8 The head of the fibula slides proximally and anteriorly (internal rotation)
15.3.1.6 Nerve Supply
15.3.1.6.1 Proximal (Superior) Tibiofibular Joint
15.3.1.6.1.1 Common Peroneal (Fibular) Nerve
15.3.1.6.1.2 Tibial Nerve
15.3.1.6.2 Distal (Inferior) Tibiofibular Joint
15.3.1.6.2.1 Tibial Nerve
15.3.2 Talocrural (Ankle) Joint (ta’’lo-krōōr’al)
15.3.2.1 Summary
15.3.2.1.1 This Synovial Hinge (Ginglymus) Type joint is formed by the congruous union of the distal end of the tibia and its medial Malleolus and the Lateral Malleolus of the fibula both forming the concave articulating surface of the mortice with the convex talar surface.
15.3.2.1.2 The fibrous capsule is lined by a synovial membrane throughout its entirety and well supported by the deltoid ligament medially and the lateral collateral ligaments (Anterior Talofibular, Posterior Talofibular, and Calcaneofibular).
15.3.2.1.3 Since the axis of movement, (20º Dorsiflexion and 45º plantarflexion) is near the tip of both malleoli these ligaments are not pulled tight during normal movement at the Talocrural joint.
15.3.2.2 Illustration
15.3.2.2.1 Anterior Ankle Tibiofibular Joint
15.3.2.2.2 The Ankle Joint (Talocrural)
15.3.2.2.3 Posterior Ankle Tibiofibular Joint
15.3.2.3 Introduction
15.3.2.3.1 The ankle joint is formed by the superior portion of the body of the talus fitting within the mortise, or cavity, formed by the combined distal ends of the tibia and fibula.
15.3.2.3.2 The medial, superior, and lateral articular surfaces of the talus are continuous, as are those of the medial Malleolus, the distal end of the tibia, and the lateral Malleolus.
15.3.2.3.3 The fibrous capsule attaches at the margins of the articular surfaces of the talus below and to the tibia and fibula above, except anteriorly, where a portion of the dorsal aspect of the neck of the talus is enclosed within the joint cavity.
15.3.2.3.4 The capsule extends somewhat superiorly between the distal ends of the tibia and fibula, to just below the Syndesmosis.
15.3.2.3.5 The fibrous capsule is lined by a synovial membrane throughout its entirety and well supported by ligaments, especially medially and laterally.
15.3.2.3.6 The concave articulating surface is the mortice, which is made up of the distal tibia and the tibial and fibular malleoli. The fibular Malleolus extends further distally than the tibial Malleolus. The combined surfaces are congruent with the body of the talus.
15.3.2.3.7 Integrity of the mortice is provided by the tibiofibular joints and their associated ligaments
15.3.2.3.8 The convex articulating surface is the body of the talus.
15.3.2.3.9 The medial ligaments are collectively referred to as the deltoid ligament (Fig. 15-12). The anterior portion of the deltoid ligament consists of the Tibionavicular ligament, superficially, and the deeper anterior Tibiotalar fibers. The Tibionavicular ligament blends with the plantar calcaneonavicular (spring) ligament inferiorly. The middle fibers of the deltoid ligament constitute the tibiocalcaneal ligament, with some Tibiotalar fibers deep to it. The posterior Tibiotalar ligament forms the posterior portion of the deltoid ligament. The deltoid ligament as a whole attaches proximally to the medial aspect of the medial malleolus and fans out to achieve the distal attachments described above. In this way, it is somewhat triangular, with the apex at its proximal attachment.
15.3.2.3.10 The lateral ligaments, unlike those of the medial side, are separate bands of fibers diverging from their proximal attachment at the distal end of the fibula (see Fig. 15 - 10). The anterior talofibular ligament the most frequently injured ligament about the ankle-passes medially, forward and downward, from the anterior aspect of the fibula to the lateral aspect of the neck of the talus. The calcaneofibular ligament runs from the tip of the lateral malleolus downward and backward to a small prominence on the upper lateral surface of the calcaneus. It is longer and narrower than the anterior and posterior talofibular ligaments. The posterior talofibular ligament passes from the malleolar fossa medially and slightly downward and backward to the lateral tubercle of the posterior aspect of the talus.
15.3.2.3.11
It should be noted that the proximal attachments of
both the medial and lateral ligaments of the ankle are near the axis of
movement for dorsiflexion and plantar flexion. For this reason, these ligaments
are not pulled tight to any significant extent during normal movement at the
Talocrural joint.[6]
Also, the calcaneofibular ligament, which crosses both the talocrural and the
talocalcaneal joints, runs parallel to, and inserts close to, the axis of
movement at the subtalar joint. It, then, plays little or no role in
restricting inversion at the subtalar joint. This is true in all positions of
dorsiflexion and plantar flexion, since it maintains a parallel orientation to the
subtalar axis throughout the range.
15.3.2.3.12 The ligaments about the talocrural joint primarily function to restrict titling and rotation of the talus within the mortise and to restrict forward or backward displacement of the leg on the tarsus. The main exception to this is the tibiocalcaneal portion of the deltoid ligament, which is so oriented as to help check eversion at the subtalar joint as well as an "eversion tilt" of the talus in the mortise.
15.3.2.3.13 In the neutral position, the anterior talofibular ligament can check posterior movement of the leg on the tarsus and external rotation of the leg on the tarsus because it is directed forward and medially. With the foot in plantar flexion, the anterior talofibular ligament becomes more vertically oriented and is in a position to check inversion of the talus in. the mortise. This ligament is the most commonly injured of the ligaments of the ankle, the mechanism of injury usually being a combined plantar flexion inversion strain.
15.3.2.3.14 The calcaneofibular ligament is directed downward and backward when the foot is in the neutral position. When the foot is dorsiflexed, the ligament becomes more vertically oriented and is in a better position to check inversion of the tarsus with respect to the leg.
15.3.2.3.15 The posterior talofibular ligaments oriented so as to check internal rotation of the leg on the tarsus and forward displacement of the leg on the tarsus.
15.3.2.3.16 The deltoid ligament, considered as a whole, contributes to restriction of eversion, internal rotation, and external rotation, as well as forward and backward displacement of the tarsus. However, sectioning of the deltoid ligament alone apparently results primarily in instability into eversion of the tarsus on the tibia, the other motions being checked by other ligaments, as described previously.
15.3.2.3.17
Figure 15-12
15.3.2.3.17.1
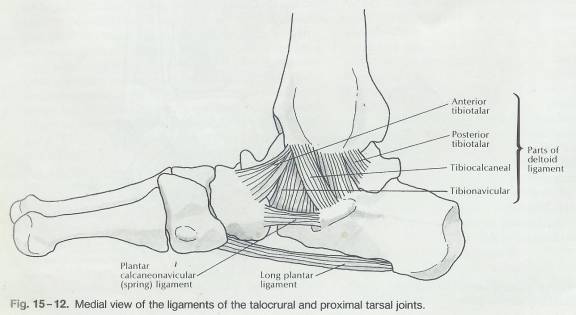
15.3.2.3.18 Figure 15-13
15.3.2.3.18.1
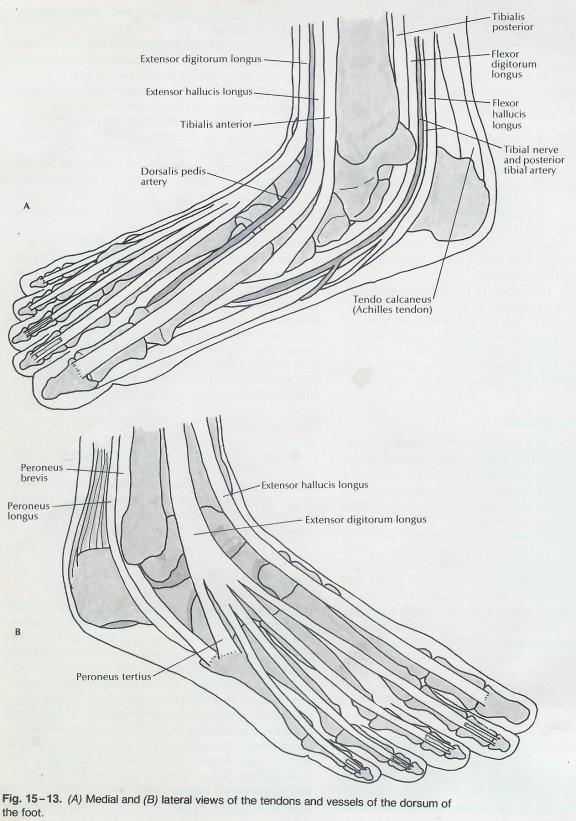
15.3.2.4 Definition
15.3.2.4.1 This joint is formed between the Talus and two bones
15.3.2.4.1.1 Distal end of the tibia and its medial Malleolus
15.3.2.4.1.2 Lateral Malleolus of the fibula
15.3.2.5 Type of Joint
15.3.2.5.1 Synovial
15.3.2.5.2 Hinge (Ginglymus) Type
15.3.2.6 Movements
15.3.2.6.1 Axis of Movement
15.3.2.6.1.1 Extends obliquely from the Posterolateral aspect of the fibular Malleolus to the Anteromedial aspect of the tibial Malleolus.
15.3.2.6.2 Degree of Movement
15.3.2.6.2.1 With the knee flexed, the ankle joint can be dorsiflexed about 20º.
15.3.2.6.2.2 If the knee is extended, the Gastrocnemius will limit the range of motion to about 10º.
15.3.2.6.2.3 The range of motion in plantar flexion is approximately 45º
15.3.2.6.3 Dorsiflexion 20º
15.3.2.6.3.1 Body of the talus slides in a posterior direction
15.3.2.6.4 Plantar Flexion 45º
15.3.2.6.4.1 Body of the talus slides in a anterior direction
15.3.2.7 Ligaments
15.3.2.7.1 Introduction
15.3.2.7.1.1 The proximal attachments of both the medial and lateral ligaments of the ankle are near the axis of movement for Dorsiflexion and plantar flexion.
15.3.2.7.1.2 As a result, these ligaments are not pulled tight to any significant extent during normal movement at the Talocrural joint.
15.3.2.7.1.3 The ligaments about the Talocrural joint primarily function to restrict tilting and rotation of the talus within the mortise and to restrict forward or backward displacement of the leg on the tarsus.
15.3.2.7.1.4 The main exception to this is the Tibiocalcaneal portion of the deltoid ligament, which is so oriented as to help check eversion at the Subtalar joint as well as an “eversion tilt” of the talus in the mortise.
15.3.2.7.2 Medial (deltoid) Ligaments
15.3.2.7.2.1 Introduction
15.3.2.7.2.2 The deltoid ligament as a whole attaches proximally to the medial aspect of the medial Malleolus and fans out to achieve the distal attachments described above.
15.3.2.7.2.3 It is somewhat triangular, with the apex at its proximal attachment
15.3.2.7.2.4 The deltoid ligament, considered as a whole, contributes to restriction of eversion, internal rotation, and external rotation, as well as forward and backward displacement of the tarsus. However, sectioning of the deltoid ligament alone apparently results primarily in stability into eversion of the tarsus on the tibia, the other motions being checked by other ligaments, as described.
15.3.2.7.2.5 Anterior Tibiotalar
15.3.2.7.2.6 Posterior Tibiotalar
15.3.2.7.2.7 Tibiocalcaneal
15.3.2.7.2.8 Tibionavicular
15.3.2.7.2.9 The Tibionavicular ligament blends with the plantar calcaneonavicular (spring) ligament inferiorly
15.3.2.7.3 Lateral Collateral Ligaments
15.3.2.7.3.1 Introduction
15.3.2.7.3.1.1 The lateral ligaments, unlike those of the medial side, are separate bands of fibers diverging from their proximal attachment at the distal end of the fibula.
15.3.2.7.3.2 Anterior Talofibular
15.3.2.7.3.2.1 The anterior Talofibular ligament is the most frequently injured ligament in ankle sprains
15.3.2.7.3.2.2 It passes medially, forward and downward from the anterior aspect of the fibula to the lateral aspect of the neck of the talus.
15.3.2.7.3.2.3 In the neutral position, the anterior Talofibular ligament can check posterior movement of the leg on the tarsus and external rotation of the leg on the tarsus because it is directed forward and medially. With the foot in plantar flexion, the anterior Talofibular ligament becomes more vertically oriented and is in a position to check inversion of the talus in the mortise. This ligament is the most commonly injured of the ligaments of the ankle, the mechanism of injury usually being a combined plantar flexion-inversion strain.
15.3.2.7.3.3 Posterior Talofibular
15.3.2.7.3.3.1 Passes from the Malleolar fossa medially and slightly downward and backward to the lateral tubercle of the posterior aspect of the talus.
15.3.2.7.3.3.2 The posterior Talofibular ligaments is oriented so as to check internal rotation of the leg on the tarsus and forward displacement of the leg on the tarsus.
15.3.2.7.3.4 Calcaneofibular
15.3.2.7.3.4.1 Runs from the tip of the lateral Malleolus downward and backward to a small prominence on the upper lateral surface of the calcaneus.
15.3.2.7.3.4.2 It is longer and narrower than the anterior and posterior Talofibular ligaments.
15.3.2.7.3.4.3 The Calcaneofibular ligament is directed downward and backward when the foot is in the neutral position. When the foot is dorsiflexed, the ligament becomes more vertically oriented and is in a better position to check inversion of the tarsus with respect to the leg.
15.3.2.7.3.4.4 The Calcaneofibular ligament, which crosses both the Talocrural and the talocalcaneal joint, runs parallel to, and inserts close to, the axis of movement at the Subtalar joint. The Calcaneofibular ligament plays little or no role in restricting inversion at the Subtalar joint. This is true in all positions of Dorsiflexion and plantar flexion, since it maintains a parallel orientation to the Subtalar axis throughout the range.
15.3.2.8 Nerve Supply
15.3.2.8.1 Deep Peroneal (Anterior Tibial) Nerve
15.3.2.8.2 Tibial Nerve (Branches Arising in the Leg)
15.3.3 Subtalar/Talocalcaneal (ta’’lo-kal-ka-ne-al)
15.3.3.1 Summary
15.3.3.1.1 This synovial modified plane or gliding joint is uniaxial and is formed by the union of the talus and calcaneus at two separate articular capsules (Posterior & Anterior) separated by the tarsal canal which divides the two joint cavities.
15.3.3.1.2 The Subtalar joint allows the movements of inversion and eversion. This joint is supported by several external ligaments (Medial and Lateral Collateral Ligaments (Talocrural), Extensor Retinaculum, Posterior and Lateral Talocalcaneal) and internal ligaments (Interosseous Talocalcaneal (Tarsal Canal) & Cervical Talocalcaneal Ligament)
15.3.3.2 Illustration
15.3.3.2.1 Talocalcaneonavicular (Illustration)
15.3.3.2.2 Posterior Ankle Tibiofibular Joint
15.3.3.3 Introduction
15.3.3.3.1 The talus also articulates with the Navicular, and the Talonavicular joint is involved in the movements ascribed to the Subtalar joint.
15.3.3.3.2 Functionally, the Subtalar joint includes the articulation between the posterior facet of the talus and the opposing articular surface of the calcaneus, as well as the articulation between the anterior and medial facets of the two bones.
15.3.3.3.3 These articulations move in conjunction with one another. Anatomically, the anterior and medial articulations are actually part of the talocalcaneonavicular joint; they are enclosed within a joint capsule separate from that of the posterior talocalcaneal articulation.
15.3.3.3.4 Functionally, the subtalar joint includes the articulation between the posterior facet of the talus and the opposing articular surface of the calcaneus, as well as the articulation between the anterior and medial facets of the two bones. These articulations move in conjunction with one another. Anatomically, the anterior and medial articulations are actually part of the talocalcaneonavicular joint; they are enclosed within a joint capsule separate from that of the posterior talocalcaneal articulation.
15.3.3.3.5 . The joint capsules of the posterior portion of the talocalcaneal joint and the talocalcaneonavicular portion of the subtalar joint are separated by the ligament of the tarsal canal. This ligament runs from the underside of the talus, at the sulcus tali, downward and laterally to the dorsum of the calcaneus, at the sulcus calcanei. Since it is situated medially to the axis of motion of inversion-eversion at the subtalar joint, it checks eversion.[7] This ligament is often referred to as the interosseous talocalcaneal ligament (see Fig. 15-11).
15.3.3.3.6 More laterally, in the sinus tarsi, is the cervical talocalcaneal ligament. It passes from the inferolateral aspect of the talar neck downward and laterally to the dorsum of the calcaneus. It occupies the anterior part of the sinus tarsi. Since the cervical ligament lies lateral to the subtalar joint axis, it restricts inversion of the calcaneus on the talus.[8]
15.3.3.3.7 Also, within the lateral aspect of the sinus tarsi, bands from the inferior aspect of the extensor retinaculum pass downward, as well as medially, to the calcaneus. These bands are considered part df the talocalcaneal ligament complex. They help check inversion at the subtalar joint.
15.3.3.4 Definition
15.3.3.4.1 This joint is formed between the Talus and calcaneus.
15.3.3.5 Type of Joint
15.3.3.5.1 Synovial
15.3.3.5.2 Modified plane or gliding joint
15.3.3.6 Movements
15.3.3.6.1 Supination and pronation are movements permitted by the Subtalar and talocalcaneonavicular joint.
15.3.3.6.2 Uniaxial
15.3.3.6.3 Inversion (Kisner[9])
15.3.3.6.3.1 Turning inward of the calcaneus and is combined with adduction, supination, and plantarflexion of the Talonavicular joint
15.3.3.6.4 Eversion (Kisner[10])
15.3.3.6.4.1 Turning outward of the calcaneus and is combined with abduction, pronation, and Dorsiflexion of the Talonavicular joint
15.3.3.6.5 Supination (Kendall[11])
15.3.3.6.5.1 Rotation of the foot in which the sole of the foot moves in a medial direction
15.3.3.6.6 Pronation (Kendall[12])
15.3.3.6.6.1 Rotation in which the sole of the foot moves in a lateral direction
15.3.3.7 Ligaments
15.3.3.7.1 Medial and Lateral Collateral Ligaments (Talocrural)
15.3.3.7.2 Extensor Retinaculum
15.3.3.7.2.1 Also, within the lateral aspect of the sinus tarsi bands from the inferior aspect of the extensor retinaculum pass downward, as well as medially, to the calcaneus. These bands are considered part of the talocalcaneal ligament complex. They help check inversion at the Subtalar joint.
15.3.3.7.3 Interosseous Talocalcaneal (Tarsal Canal)
15.3.3.7.3.1 The ligament of the tarsal canal separates the joint capsules of the posterior portion of the talocalcaneal joint and the talocalcaneonavicular portion of the Subtalar joint. This ligament runs from the underside of the talus, at the Sulcus tali, downward and laterally to the dorsum of the calcaneus at the Sulcus calcanei. Since it is situated medially to the axis of motion of inversion-eversion at the Subtalar joint, it checks eversion. This ligament is often referred to as the interosseous talocalcaneal ligament.
15.3.3.7.4 Cervical Talocalcaneal Ligament
15.3.3.7.4.1 More laterally, in the sinus tarsi, is the cervical talocalcaneal ligament. It passes from the inferolateral aspect of the talar neck downward and laterally to the dorsum of the calcaneus. It occupies the anterior part of the sinus tarsi. Since the cervical ligament lies lateral to the Subtalar joint axis, it restricts inversion of the calcaneus on the talus.
15.3.3.7.5 Posterior and Lateral Talocalcaneal
15.3.3.8 Articulations
15.3.3.8.1 There are three articulations between the talus and calcaneus; the posterior is separated from the anterior and middle by the tarsal canal. The canal divides the Subtalar joint into two joint cavities.
15.3.3.8.2 With physiologic motions of the Subtalar joint, the convex posterior portion of the calcaneus slides opposite to the motion; the concave anterior and middle facets on the calcaneus slide in the same direction.
15.3.3.8.2.1 Inversion
15.3.3.8.2.1.1 Posterior Articulation Slides Lateral
15.3.3.8.2.2 Eversion
15.3.3.8.2.2.1 Posterior Articulation Slides Medial
15.3.3.8.3 Posterior Articulation
15.3.3.8.3.1 Has its own capsule; the facet on the bottom of the talus is concave, while the opposing facet on the calcaneus is convex.
15.3.3.8.4 Anterior Articulations
15.3.3.8.4.1 Enclosed in the same capsule as the Talonavicular articulation, forming the talocalcaneonavicular joint. Functionally, these articulations work together. The facets of the anterior and middle articulations on the talus are convex, while the opposing facets on the calcaneus are concave.
15.3.3.9 Nerve Supply
15.3.3.9.1 Medial Plantar (Tibial)
15.3.4 Talocalcaneonavicular (TCN)
15.3.4.1 Summary
15.3.4.1.1 This Synovial, compound ball & socket joint with the Navicular forming the socket and the talus forming the ball. The talus articulates with the calcaneus at anterior and medial facets. All of the above articulations are enclosed in the same fibrous capsule. The joint is supported by the calcaneonavicular (Spring) ligament, Bifurcate Ligament (Calcaneonavicular Portion), Deltoid Ligament (Tibionavicular Portion), and Dorsal Talonavicular ligament. The joint assists in inversion and eversion.
15.3.4.2 Illustration
15.3.4.2.1 Plantar Ligaments & Joints
15.3.4.2.2 Talocalcaneonavicular (Illustration)
15.3.4.3 Introduction
15.3.4.3.1 The TCN joint includes the articulation between the anterior and medial facets of the talus and calcaneus (Subtalar/Talocalcaneal Joint), the articulations between the inferior aspect of the head of the talus and the subjacent spring ligament, and the articulation between the anterior aspect of the head of the talus and the posterior articular surface of the Navicular.
15.3.4.3.2 The Talonavicular portion of this joint constitutes the medial half of the transverse tarsal joint.
15.3.4.3.3 The talocalcaneonavicular joint is enclosed by a joint capsule, the posterior aspect of which transverses the tarsal canal, forming the anterior wall of the canal. The capsule is reinforced by the spring ligament inferiorly, the calcaneonavicular portion to the bifurcate ligament laterally, and the Tibionavicular portion of the deltoid ligament medially.
15.3.4.3.4 The talocalcaneonavicular joint includes the articulation between the anterior and medial facets of the talus and calcaneus (described previously as part of the subtalar joint), the articulations between the inferior aspect of the head of the talus and the subjacent spring ligament, and the articulation between the anterior aspect of the head of the talus and the posterior articular surface of the navicular. The combined talonavicular and talo-spring ligament portion of this joint is essentially a compound ball-and socket joint; the head of the talus is the ball, while the superior surface of t4e spring ligament and the posterior surface of the navicular form: the socket. It should be noted that the superior surface of the spring ligament is lined with articular cartilage. The talonavicular portion of this joint constitutes the medial half of the transverse tarsal joint..
15.3.4.3.5 The talocalcaneonavicular joint is enclosed by a joint capsule, the posterior aspect of which traverses the tarsal canal, forming the anterior wall of the canal.. The capsule, is reinforced by the spring ligament inferiorly, the calcaneonavicular portion of the bifurcate ligament laterally, and the tibionavicular portion of the deltoid ligament medially (see Figs. 15-10 and 15-12).
15.3.4.3.6 The spring ligament passes from the anterior and medial margins of the sustentaculum tali forward to the inferior and inferomedial aspect of the navicular.
15.3.4.3.7 . As mentioned, its superior surface articulates with the underside of the head of the talus. This ligament maintains apposition of the medial aspects of the forefoot and hindfoot and in so doing helps to maintain the normal arched configuration of the foot. Laxity of the ligament allows. a medial separation between the calcaneus and forefoot, with the forefoot assuming an abducted position with respect to the hindfoot. At the same time, the foot is allowed to "untwist," which effectively lowers the normal arch of the foot, and the talar head is allowed to move medially and inferiorly. Further discussion of the twisted configuration and arching of the foot is included in the section on biomechanics.
15.3.4.4 Definition
15.3.4.4.1 This joint is formed between the anterior capsule of the Subtalar/Talocalcaneal Joint and the Navicular.
15.3.4.5 Type of Joint
15.3.4.5.1 Synovial
15.3.4.5.2 Compound Ball & Socket
15.3.4.5.2.1 The combined Talonavicular and talo-spring ligament portion of this joint is essentially a compound ball and socket joint; the head of the talus is the ball, while the superior surface of the spring ligament and the posterior surface of the Navicular form the socket. The superior surface of the spring ligament is lined with articular cartilage.
15.3.4.6 Movements
15.3.4.6.1 Inversion
15.3.4.6.2 Eversion
15.3.4.6.3 Navicular Accessory Motions
15.3.4.6.3.1 Inversion
15.3.4.6.3.1.1 Introduction
15.3.4.6.3.1.1.1 When the foot is inverted with supination and plantarflexion the Navicular slides on the head of the talus in a plantar direction
15.3.4.6.3.1.1.2 When the foot is everted with pronation and Dorsiflexion the Navicular slides on the head of the talus in a dorsal direction.
15.3.4.6.3.2 Rotation
15.3.4.6.3.2.1 Turning inward, or supination
15.3.4.6.3.3 Dorsal sliding
15.3.4.6.3.4 Supination
15.3.4.6.3.5 Plantarflexion
15.3.4.6.3.6 Adduction
15.3.4.6.3.7 Eversion
15.3.4.6.3.8 Rotation
15.3.4.6.3.8.1 Turning outward, or pronation, of the foot
15.3.4.6.3.9 Plantar Sliding
15.3.4.6.3.10 Pronation
15.3.4.6.3.11 Dorsiflexion
15.3.4.6.3.12 Abduction
15.3.4.7 Ligaments
15.3.4.7.1 Calcaneonavicular (Spring) Ligament
15.3.4.7.1.1 The spring ligament passes from the anterior and medial margins of the sustentaculum tali forward to the inferior and inferomedial aspect of the Navicular. Its superior surface articulates with the underside of the head of the talus. This ligament maintains apposition of the medial aspects of the forefoot and Hindfoot and in so doing helps to maintain the normal arched configuration of the foot. Laxity of the ligament allows a medial separation between the calcaneus and forefoot, with the forefoot assuming an abducted position with respect to the Hindfoot.
15.3.4.7.1.2 At the same time, the foot is allowed to “untwist” which effectively lowers the normal arch of the foot, and the talar head is allowed to move medially and inferiorly.
15.3.4.7.1.3 The plantar calcaneonavicular ligament is a broad and thick band of fibers, which connects the anterior margin of the sustentaculum tali of the calcaneus to the plantar surface of the Navicular. This ligament not only serves to connect the calcaneus and Navicular, but supports the head of the talus, forming part of the articular cavity in which it is received. The dorsal surface of the ligament presents a fibrocartilaginous facet, lined by the synovial membrane, and upon this a portion of the head of the talus rests. Its plantar surface is supported by the tendon of the Tibialis posterior; its medial border is blended with the forepart of the deltoid ligament of the ankle-joint.
15.3.4.7.1.4 The plantar calcaneonavicular ligament, by supporting the head of the talus, is principally concerned in maintaining the arch of the foot. When it yields, the head of the talus is pressed downward, medialward, and forward by the weight of the body, and the foot becomes flattened, expanded, and turned lateralward, and exhibits the condition known as flat-foot. This ligament contains a considerable amount of elastic fibers, so as to give elasticity to the arch and spring to the foot; hence it is sometimes called the “spring” ligament. It is supported, on its plantar surface, by the tendon of the Tibialis posterior, which spreads out at its insertion into a number of fasciculi, to be attached to most of the tarsal and metatarsal bones. This prevents undue stretching of the ligament, and is a protection against the occurrence of flat-foot; hence muscular weakness is, in most cases, the primary cause of the deformity.
15.3.4.7.2 Bifurcate Ligament (Calcaneonavicular Portion)
15.3.4.7.3 Deltoid Ligament (Tibionavicular Portion)
15.3.4.7.4 Dorsal Talonavicular[13]
15.3.4.8 Nerve Supply
15.3.4.8.1 Medial Plantar (Tibial)
15.3.5 Calcaneocuboid
15.3.5.1 Summary
15.3.5.1.1 This synovial, sellar (saddle) joint between the calcaneus (convex in a dorsal to plantar direction and concave in a medial to lateral direction) and the cuboid (reciprocally concave and convex)
15.3.5.1.2 This joint is supported by the Calcaneocuboid (Short Plantar) Ligament, Long Plantar ligament and the Bifurcate Ligament (Calcaneocuboid Band).
15.3.5.2 Introduction
15.3.5.2.1 The lateral portion of the transverse tarsal joint is the calcaneocuboid joint.
15.3.5.2.2 The calcaneocuboid joint is a sellar joint in that the Calcaneal joint surface is concave superoinferiorly and convex mediolaterally; the adjoining cuboid surface is reciprocally shaped. This joint is enclosed in a joint capsule distinct from that of the talocalcaneonavicular joint and constitutes the lateral half of the transverse tarsal joint.
15.3.5.2.3 The joint capsule is reinforced inferiorly by the strong plantar calcaneocuboid (short plantar) ligament and the long plantar ligament.
15.3.5.2.4 Dorsally, the joint capsule is reinforced by the calcaneocuboid band of the bifurcate ligament.
15.3.5.2.5 The lateral portion of the transverse tarsal joint is the calcaneocuboid joint. The calcaneocuboid joint is a sellar joint in that the calcaneal joint surface is concave superoinferiorly and convex mediolaterally (see Figs. 15-3 and 15-4); the adjoining cuboid surface is reciprocally shaped. This joint is enclosed in a joint capsule distinct from that of the talocalcaneonavicular joint and constitutes the lateral half of the transverse tarsal joint. The joint capsule is reinforced inferiorly by the strong plantar calcaneocuboid (short plantar) ligament and the long plantar ligament. The short plantar ligament runs from the anterior tubercle of the plantar aspect of the calcaneus to the underside of the cuboid. The long plantar ligament runs from the posterior tubercles of the calcaneus forward to the bases of the fifth, fourth, third, and sometimes second metatarsals (see Fig. 15-9). Both of these ligaments support the normal arched configuration of the foot by helping to maintain a twisted relationship between the hindfoot and forefoot. Dorsally, the joint capsule is reinforced' by the calcaneocuboid band of the bifurcate ligament (see Fig. 15-10)
15.3.5.3 Definition
15.3.5.3.1 This joint is formed between the calcaneus and the cuboid bones.
15.3.5.4 Type of Joint
15.3.5.4.1 Synovial
15.3.5.4.2 Sellar (Saddle)
15.3.5.4.2.1 The articulating surface of the calcaneus is convex in a dorsal to plantar direction and concave in a medial to lateral direction; the articulating surface of the cuboid is reciprocally concave and convex.
15.3.5.5 Movements
15.3.5.5.1
15.3.5.6 Ligaments
15.3.5.6.1 Introduction
15.3.5.6.1.1 Both the long and short plantar ligaments support the normal arched configuration of the foot by helping to maintain a twisted relationship between the Hindfoot and forefoot.
15.3.5.6.2 Calcaneocuboid (Short Plantar) Ligament
15.3.5.6.2.1 The short plantar ligament runs from the anterior tubercle of the plantar aspect of the calcaneus to the underside of the cuboid.
15.3.5.6.2.2 The plantar calcaneocuboid ligament lies nearer to the bones than the preceding, from which it is separated by a little Areolar (ă-realer) tissue. It is a short but wide band of great strength, and extends from the tubercle and the depression in front of it, on the forepart of the plantar surface of the calcaneus, to the plantar surface of the cuboid behind the peroneal groove.
15.3.5.6.3 Long Plantar Ligament
15.3.5.6.3.1 The long plantar ligament runs from the posterior tubercles of the calcaneus forward to the bases of the fifth, fourth, third, and sometimes second metatarsals.
15.3.5.6.3.2 The rough surface in front of the calcaneus processes gives attachment to the long plantar ligament. On the distal end it attaches to the cuboid bone whose plantar surface presents in front with a deep groove (Peroneal Sulcus), which runs obliquely forward and medial ward (Peroneus Longus tendon inserts). Behind this groove is a prominent ridge where the long plantar ligament is attached.
15.3.5.6.3.3 The long plantar ligament is the longest of all the ligaments of the tarsus: it is attached behind to the plantar surface of the calcaneus in front of the tuberosity, and in front to the tuberosity on the plantar surface of the cuboid bone, the more superficial fibers being continued forward to the bases of the (sometimes second), third, fourth and fifth metatarsal bones. This ligament converts the groove on the plantar surface of the cuboid into a canal for the tendon of the Peroneus longus.
15.3.5.6.4 Bifurcate Ligament (Calcaneocuboid Band)
15.3.6 Metatarsophalangeal Joints (MP)
15.3.6.1 Summary
15.3.6.1.1 This synovial, Condyloid (KON-di-loyd) joint is formed between the distal ends of the metatarsals with the adjacent end of the proximal phalanges and supported by the medial and lateral collateral ligaments and the plantar ligaments. The joint movements are flexion, extension, abduction, and adduction.
15.3.6.2 Illustration
15.3.6.2.1 Bones of the right Foot, Dorsal View
15.3.6.2.2 Bones of the Right Foot Plantar View
15.3.6.2.3 Ligaments on the Plantar Surface of the Right Foot (Superficial)
15.3.6.2.4 Plantar Calcaneonavicular Ligament and the Insertions of three Tendons
15.3.6.3 Introduction
15.3.6.3.1 The metatarsophalangeal joints are condyloid formed by the articulation of the distal ends of the metatarsals with the adjacent ends of the proximal phalanges.
15.3.6.3.2 The plantar surface of this joint is considerably thickened because of the plantar ligament at the MP joint and thus flexion is restricted.
15.3.6.3.3 The dorsal surface of the MP joint is loose which permits a wider rage of extension when compared to flexion.
15.3.6.3.4 Two sesamoid bones are embedded in the plantar ligament of the big toe.
15.3.6.3.5 The plantar aponeurosis is inserted into slips on either side of the MP joint.
15.3.6.4 Definition
15.3.6.4.1 This joint is formed between the distal end of the metatarsal with the adjacent end of the proximal phalanges
15.3.6.5 Type of Joint
15.3.6.5.1 Synovial
15.3.6.5.2 Ellipsoidal or Condyloid (KON-di-loyd)
15.3.6.6 Movements
15.3.6.6.1 Introduction
15.3.6.6.1.1 Flexion and extension are movements about a coronal axis.
15.3.6.6.1.2 Adduction and abduction are movements about a Sagittal axis. The line of reference for adduction and abduction of the toes is the axial line projected distally in line with the second metatarsal and extending through the second digit.
15.3.6.6.1.3 Because abduction of the toes is restricted by the wearing of shoes, this movement is markedly limited in most adults.
15.3.6.6.2 Flexion 30º
15.3.6.6.2.1 Movement in a caudal direction
15.3.6.6.3 Extension 40º
15.3.6.6.3.1 Movement in a cranial direction
15.3.6.6.4 Adduction
15.3.6.6.4.1 Movement toward the axial line
15.3.6.6.5 Abduction
15.3.6.6.5.1 Movement away from the axial line
15.3.6.7 Ligaments
15.3.6.7.1 Medial and Lateral Collateral Ligaments
15.3.6.7.2 Plantar Ligament
15.3.6.8 Nerve Supply
15.3.6.8.1 Medial Plantar (Tibial)
15.3.6.9 Lateral Plantar Nerve & Superficial Branch
15.3.7 Interphalangeal Joints of Toes (IP)
15.3.7.1 Summary
15.3.7.1.1 This synovial, hinge joint is formed between the adjacent surfaces of the phalanges and its movements are flexion and extension.
15.3.7.2 Illustration
15.3.7.2.1 Bones of the right Foot, Dorsal View
15.3.7.2.2 Bones of the Right Foot Plantar View
15.3.7.2.3 Ligaments on the Plantar Surface of the Right Foot (Superficial)
15.3.7.3 Introduction
15.3.7.3.1 The Interphalangeal joints are ginglymus or hinge joints formed by the articulations of adjacent surfaces of phalanges
15.3.7.4 Definition
15.3.7.4.1 This joint is formed between the adjacent surfaces of the phalanges
15.3.7.5 Type of Joint
15.3.7.5.1 Synovial
15.3.7.5.2 Ginglymus (JIN-gli-mus) or Hinge Joints
15.3.7.6 Movements
15.3.7.6.1 Introduction
15.3.7.6.1.1 Flexion and extension are movements about a coronal axis
15.3.7.6.2 Flexion
15.3.7.6.2.1 Movement in a caudal direction
15.3.7.6.3 Extension
15.3.7.6.3.1 Movement in a cranial direction
15.3.7.7 Nerve Supply
15.3.7.7.1 Medial Plantar (Tibial)
15.3.7.8 Lateral Plantar Nerve & Superficial Branch
15.3.8 Intercuneiform and Cuneocuboid Articulations
15.3.8.1 Illustration Definition
15.3.8.1.1 http://www.bartleby.com/107/96.html
15.3.8.2 Summary
15.3.8.2.1 These synovial gliding joints are formed between the cuneiform bones and between the cuneiform and cuboid bones. The joints permit minimal gliding movements and are supported by dorsal, plantar and Interosseous Ligaments.
15.3.8.3 Illustrations
15.3.8.3.1 Bones of the right Foot, Dorsal View
15.3.8.3.2 Bones of the Right Foot Plantar View
15.3.8.3.3 Right Foot Synovial Joint Cavities
15.3.8.3.4 Intertarsal and Tarsometatarsal Joints (Horizontal Section of the Right Foot)
15.3.8.4 Definition
15.3.8.4.1 This joint is formed between the adjacent surfaces of the cuneiform bones
15.3.8.5 Type of Joint
15.3.8.5.1 Synovial
15.3.8.5.2 Gliding
15.3.8.6 Movements
15.3.8.6.1 Minimal Gliding
15.3.8.7 Ligaments
15.3.8.7.1 Dorsal Ligaments
15.3.8.7.1.1 Consist of three transverse bands: one connects the first with the second cuneiform, another the second with the third cuneiform, and another the third cuneiform with the cuboid.
15.3.8.7.2 Plantar Ligaments
15.3.8.7.2.1 Similar arrangement to the dorsal, and are strengthened by slips from the tendon of the Tibialis posterior.
15.3.8.7.3 Interosseous Ligaments
15.3.8.7.3.1 Consist of strong transverse fibers, which pass between the rough non-articular portions of the adjacent surfaces of the bones.
15.3.9 Tarsometatarsal Articulations
15.3.9.1 Illustration Definition
15.3.9.1.1 http://www.bartleby.com/107/97.html
15.3.9.2 Summary
15.3.9.2.1 These synovial gliding joints are formed between the cuneiform, cuboid and bases of the five metatarsal bones. These joints permit minimal gliding movement and are supported by dorsal, plantar and Interosseous Ligaments.
15.3.9.3 Definition
15.3.9.3.1 This joint is formed between the adjacent surfaces of the first, second, and third cuneiforms, and the cuboid, which articulate with the bases of the metatarsal bones.
15.3.9.3.2 The first metatarsal bone articulates with the first cuneiform; the second is deeply wedged in between the first and third cuneiforms articulating by its base with the second cuneiform; the third articulates with the third cuneiform; the fourth, with the cuboid and third cuneiform; and the fifth, with the cuboid.
15.3.9.4 Type of Joint
15.3.9.4.1 Synovial
15.3.9.4.2 Gliding
15.3.9.5 Movements
15.3.9.5.1 Minimal Gliding
15.3.9.6 Ligaments
15.3.9.6.1 Dorsal Ligaments
15.3.9.6.1.1 The dorsal ligaments are strong, flat bands. The first metatarsal is joined to the first cuneiform by a broad, thin band; the second has three, one from each cuneiform bone; the third has one from the third cuneiform; the fourth has one from the third cuneiform and one from the cuboid; and the fifth, one from the cuboid.
15.3.9.6.2 Plantar Ligaments
15.3.9.6.2.1 The plantar ligaments consist of longitudinal and oblique bands, disposed with less regularity than the dorsal ligaments. Those for the first and second metatarsals are the strongest; the second and third metatarsals are joined by oblique bands to the first cuneiform; the fourth and fifth metatarsals are connected by a few fibers to the cuboid
15.3.9.6.3 Interosseous Ligaments
15.3.9.6.3.1 The interosseous ligaments are three in number. The first is the strongest, and passes from the lateral surface of the first cuneiform to the adjacent angle of the second metatarsal. The second connects the third cuneiform with the adjacent angle of the second metatarsal. The third connects the lateral angle of the third cuneiform with the adjacent side of the base of the third metatarsal.
15.3.10 Intermetatarsal Articulations
15.3.10.1 Illustration Definition
15.3.10.1.1 http://www.bartleby.com/107/98.html
15.3.10.2 Summary
15.3.10.2.1 These synovial gliding joints are formed between the adjacent surfaces of the heads and bases of the five metatarsal bones. The joints permit minimal gliding movement and are supported by dorsal, plantar, Interosseous Ligaments and Transverse Metatarsal Ligaments.
15.3.10.3 Definition
15.3.10.3.1 This joint is formed between the adjacent surfaces of the heads and bases of the five metatarsal bones.
15.3.10.4 Type of Joint
15.3.10.4.1 Synovial
15.3.10.4.2 Gliding
15.3.10.5 Movements
15.3.10.5.1 Minimal Gliding
15.3.10.6 Ligaments
15.3.10.6.1 Introduction
15.3.10.6.1.1 The base of the first metatarsal is not connected with that of the second by any ligaments; in this respect the great toe resembles the thumb.
15.3.10.6.1.2 The bases of the other four metatarsals are connected by the dorsal, plantar, and interosseous ligaments.
15.3.10.6.2 Dorsal Ligaments
15.3.10.6.2.1 Pass transversely between the dorsal surfaces of the bases of the adjacent metatarsal bones.
15.3.10.6.3 Plantar Ligaments
15.3.10.6.3.1 Similar arrangement to the dorsal
15.3.10.6.4 Interosseous Ligaments
15.3.10.6.4.1 Consist of strong transverse fibers, which connect the rough non-articular portions of the adjacent surfaces.
15.3.10.6.5 Transverse Metatarsal Ligament
15.3.10.6.5.1 The transverse metatarsal ligament is a narrow band which runs across and connects together the heads of all the metatarsal bones; it is blended anteriorly with the plantar (glenoid) ligaments of the metatarsophalangeal articulations. Its plantar surface is concave where the Flexor tendons run below it; above it the tendons of the Interossei pass to their insertions. It differs from the transverse metacarpal ligament in that it connects the metatarsal to the others.
15.3.11 Synovial Membranes of Foot (Review)
15.3.11.1 Summary
15.3.11.1.1 There are nine synovial membranes in the foot enclosing both single and multiple articulations in the foot. 1.) Subtalar/Talocalcaneal 2.) Talocalcaneal 3.) Talocalcaneonavicular 4.) Calcaneocuboid 5.) Cuneonavicular 6.) Intercuneiform, Cuneocuboid, and cuneiform (2nd & 3rd)/metatarsal (2nd, 3rd, & 4th) 7.) 1st cuneiform with great toe 8.) Cuboid & Metatarsal (4th & 5th) 9.) Navicular & Cuboid (Rare)
15.3.11.2 Synovial Membranes
15.3.11.2.1 Subtalar/Talocalcaneal (ta’’lo-kal-ka-ne-al)
15.3.11.2.2 Talocalcaneal
15.3.11.2.3 Talocalcaneonavicular
15.3.11.2.4 Calcaneocuboid
15.3.11.2.5 Cuneonavicular
15.3.11.2.6 Intercuneiform, Cuneocuboid and the articulations of the second and third cuneiforms with the bases of the second and third metatarsal bones, and the adjacent surfaces of the bases of the second, third, and fourth metatarsal bones
15.3.11.2.7 First cuneiform with the metatarsal bone of the great toe
15.3.11.2.8 Cuboid with the fourth and fifth metatarsal bones
15.3.11.2.9 Contiguous surfaces of the Navicular and cuboid bones (Rare)
15.4 Biomechanics (Kessler)
15.4.1 Introduction
15.4.1.1 Summary
15.4.1.1.1 Problems in the biomechanics of the foot ankle complex are likely to cause abnormal stresses to the joints of the foot and ankle, as well as to the other weight-bearing joints such as the knee, hip, or lower spine. The foot/ankle as a movable pivot helps in the maintenance of balance and economy of energy consumption, which are adversely affected by inadequate mobility, and improper structural alignment of the foot ankle complex.
15.4.1.2 The joints of the foot and ankle constitute the first movable pivots in the weight-bearing extremity once the foot becomes fixed to the ground.
15.4.1.3 Considered together, these joints must permit mobility in all planes in order to allow for minimal displacement of a person’s center of gravity with respect to the base of support when walking over flat or uneven surfaces. In this sense maintenance of balance and economy of energy consumption are, in part, dependent on proper functioning of the ankle-foot complex.
15.4.1.4 Adequate mobility and proper structural alignment of these joints are also necessary for normal attenuation of forces transmitted from the ground to the weight-bearing extremity.
15.4.1.5 Deviations in alignment and changes in mobility are likely to cause abnormal stresses to the joints of the foot and ankle, as well as to the other weight-bearing joints. It follows that detection of biomechanical alterations in the ankle-foot region is often necessary for adequate interpretation of painful conditions affecting the foot and ankle, as well as conditions affecting the knee, hip, or lower spine.
15.4.1.6 Figure 15-13
15.4.1.6.1
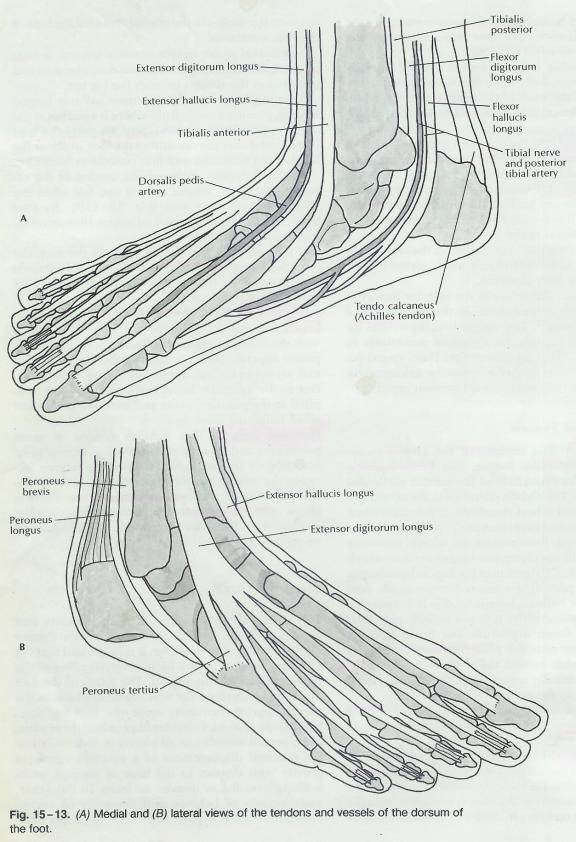
15.4.2 Structural Alignment
15.4.2.1 Summary
15.4.2.1.1 In the normal standing position, the patella faces straight forward, the knee joint axis lies in the frontal plane and the tibial tubercle is in line with the midline or lateral half of the patella and a line passing through the tips of the of the malleoli should be 20° to 25° with the frontal plane. The lateral Malleolus is positioned inferiorly with respect to the medial Malleolus such that the intermalleolar line makes an angle of about 10° with the transverse plane. With the patellae facing straight forward, the feet should be pointed outward about 5° to 10°. A Valgus positioning of the calcaneus on the talus is associated with pronation at the Subtalar joint, whereas a varus hind-foot involves supination. When considering the structure of the foot as a whole, it is helpful to compare it to a twisted plate; the calcaneus, at one end, is positioned vertically when contacting the ground, whereas the metatarsal heads are positioned horizontally when making contact with a flat surface. The medial arch is dependent almost entirely on the twisted configuration of the foot, which is maintained statically by the short and long plantar ligaments and dynamically by the anterior and posterior tibialis muscles. Referring back to the cardboard model, notice that when the cardboard is allowed to untwist by inclining the vertical end in one direction and keeping the other end flat on the table the arch flattens. In the foot, inclination of the vertical component of the structure, the calcaneus, will result in similar untwisting or twisting; this results in a respective decrease or increase in the arching of the foot, if the metatarsal heads remain in contact with the ground. The person who stands with the heel in a valgus position will have a relatively "flat" or untwisted foot, whereas a person whose heel is in a varus position when standing will appear to have a "high" arch because of increased twisting between hindfoot and forefoot.
15.4.2.2 In the normal standing position, the patella faces straight forward, the knee joint axis lies in the frontal plane and the tibial tubercle is in line with the midline or lateral half of the patella. In this position, a line passing between the tips of the malleoli should make an angle of about 20° to 25° with the frontal plane. This represents the normal amount of tibial torsion; the distal end of the tibia is rotated outward with respect to the proximal end.
15.4.2.3 The lateral Malleolus is positioned inferiorly with respect to the medial Malleolus such that the intermalleolar line makes an angle of about 10° with the transverse plane. The joint axis of the ankle mortise joint corresponds approximately to the intermalleolar line.
15.4.2.4 With the patellae facing straight forward, the feet should be pointed outward about 5° to 10°.
15.4.2.5 If, when the feet are in normal standing alignment, the patellae face inward, increased femoral anterversion, increased external tibial torsion, or both, may be present. Clinically, the fault can be differentiated by assessing rotational range of motion of the hips and estimating the degree of tibial torsion by noting the rotational alignment of the malleoli with respect to the patellae and tibial tubercles.
15.4.2.6 In the presence of increased hip anterversion, the total range of hip motion will be normal but skewed such that internal rotation is excessive and external rotation is restricted proportionally. Similar considerations holds for a situation in which the patellae face outward when the feet are normally aligned; femoral retroversion, internal tibial torsion, or both, are likely to exist.
15.4.2.7 With respect to the frontal plane, normal knee alignment may vary from slight genu valgum to some degree of genu Varum. Since in most persons the medial femoral condyle extends farther distally than the later condyle, slight genu valgum tends to be more prevalent.
15.4.2.8 At the hndfoot, the calcaneus should be positioned in vertical alignment with the tibia. A valgus or varus heel can usually be observed as a bowing of the Achilles tendon. A Valgus positioning of the calcaneus on the talus is associated with pronation at the Subtalar joint, whereas a varus hind-foot involves supination.
15.4.2.9 When considering the structure of the foot as a whole, it is helpful to compare it to a twisted plate (Figure 15-14); the calcaneus, at one end, is positioned vertically when contacting the ground, whereas the metatarsal heads are positioned horizontally when making contact with a flat surface.
15.4.2.10 Figure 15-14
15.4.2.10.1
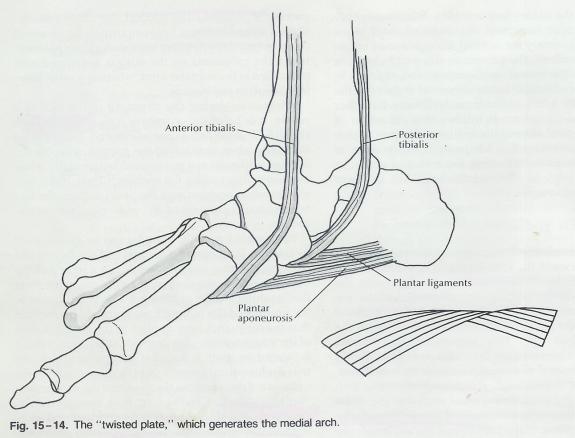
15.4.2.11 Thus, in the normal standing position on a flat, level surface, the metatarsal heads are twisted 90° with respect to the calcaneus.
15.4.2.12 To demonstrate this, a model can be constructed by taking a light rectangular piece of cardboard and twisting it so that one end lies flat on a table and the opposite end is perpendicular to the tabletop. Note the “arching” of the cardboard. This is analogous t the arching of the human foot. It should be realized that the term arch her applies to the configuration of the structure, which is dependent on the fact that it is twisted on itself. It does not refer to an arch in the true architectural sense, in which the arched configuration is dependent on the shapes of the component “building blocks.”
15.4.2.13 In the foot, both situations exist. On the medial side, there is little architectural arching and, therefore, little inherent stability of the medial arch. The medial arch is dependent almost entirely on the twisted configuration of the foot, which is maintained statically by the short and long plantar ligaments and dynamically by the anterior and posterior tibialis muscles. In contrast, the lateral side of the foot represents a true architectural arch. (Fig. 15-15) Here the cuboid, being wedged between the calcaneus and metatarsals, serves as the structural keystone. Only a small component of the lateral arch is a result of the twisted configuration of the foot.
15.4.2.14 Figure 15-15
15.4.2.14.1
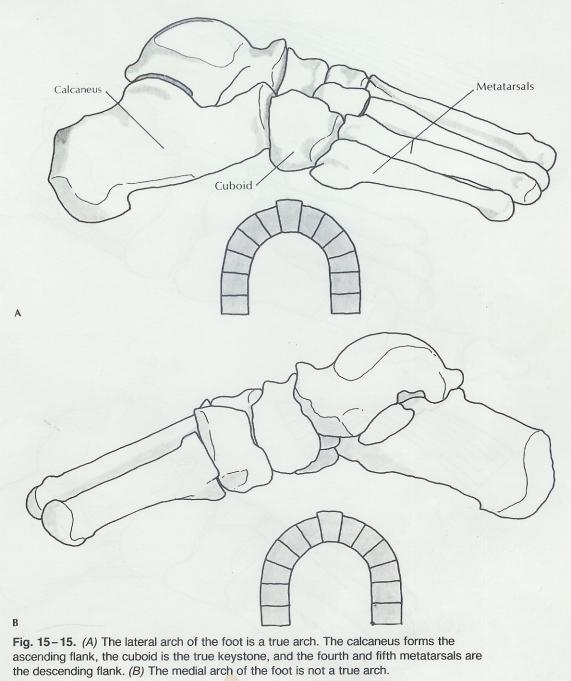
15.4.2.15 Referring back to the cardboard model, notice that when the cardboard is allowed to untwist by inclining the vertical end in one direction and keeping the other end flat on the table the arch flattens. Inclining the vertical end in the opposite direction increases the twist and increases the arch. In the foot, inclination of the vertical component of the structure, the calcaneus, will result in similar untwisting or twisting; this results in a respective decrease or increase in the arching of the foot, if the metatarsal heads remain in contact with the ground. (Fig. 15-16)
15.4.2.16 Figure 15-16
15.4.2.16.1
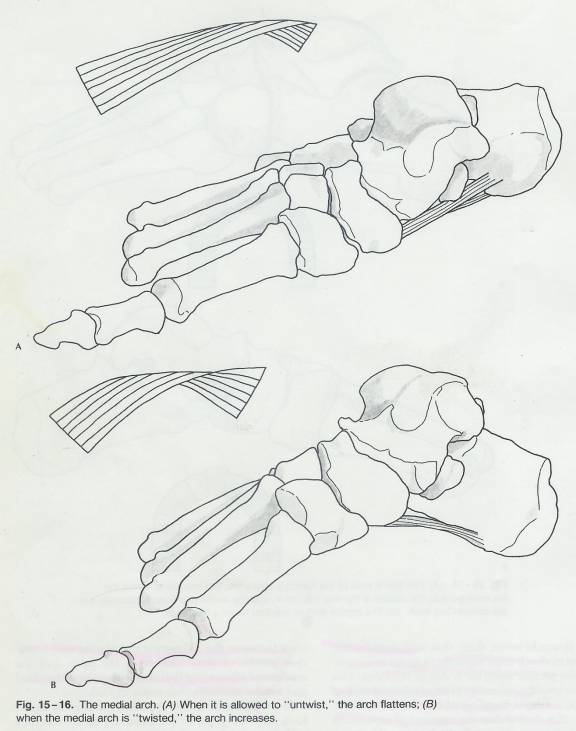
15.4.2.17 The person who stands with the heel in a valgus position will have a relatively “flat” or untwisted foot, whereas a person whose heel is in a varus position when standing will appear to have a “high” arch because of increased twisting between hindfoot and forefoot. The former situation is often termed a pronated foot or flatfoot, while the latter is termed a supinated foot or pes cavus. In the situation of the heel remaining in a vertical position but the metatarsal heads inclined on, say, an uneven surface, the effect will also be to twist or untwist the foot and, therefore, to raise or to lower the arch. For example, if the inclination is such that the first metatarsal head is on a higher level than the fifth, the forefoot supinates on the hndfoot, untwisting the foot and lowering the arch.
15.4.2.18 Note that supination of the forefoot with the hindfoot fixed is the same as pronation of the hindfoot with the forefoot fixed; they both involve untwisting of the tarsal skeleton from motion at the Subtalar, transverse tarsal, and tarsal-metatarsal joints.
15.4.2.19 Reference is often made to a transverse arch of the foot, distinguishing it from the longitudinal arch. The cardboard model should help to make it clear that some transverse arching results from the twisted configuration of the foot. This is simply a transverse component of the arch discussed previously. This transverse component will increase and decrease along with twisting and untwisting of the foot. There is also a structural component to the transverse arching of the foot, resulting from the contours and relationships of the tarsals and metatarsals. It must be realized, however, that at the level of the metatarsal heads in the standing subject, not transverse arch exists, since each of the heads makes contact with the floor.
15.4.2.20 Figure 15-21
15.4.2.20.1
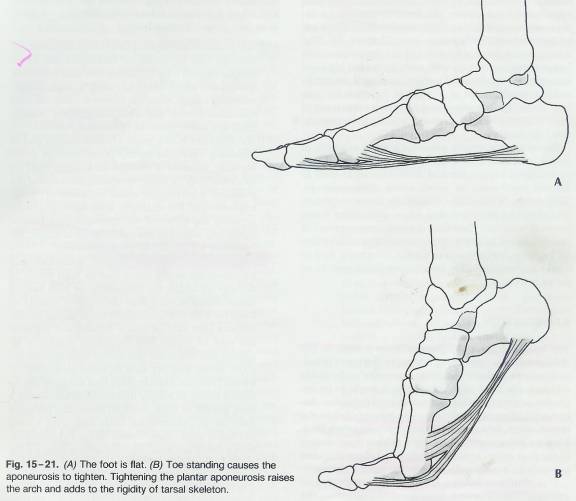
15.4.2.21 Figure 15-22
15.4.2.21.1
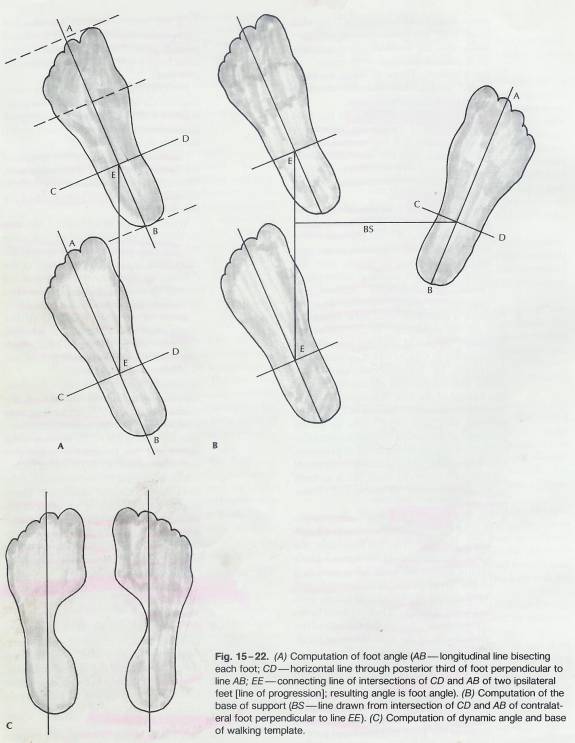
15.4.2.22 Figure 15-23&24
15.4.2.22.1
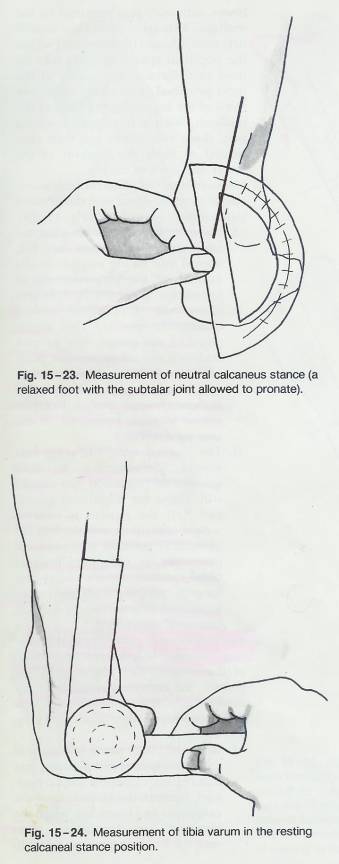
15.4.2.23 Figure 15-25
15.4.2.23.1
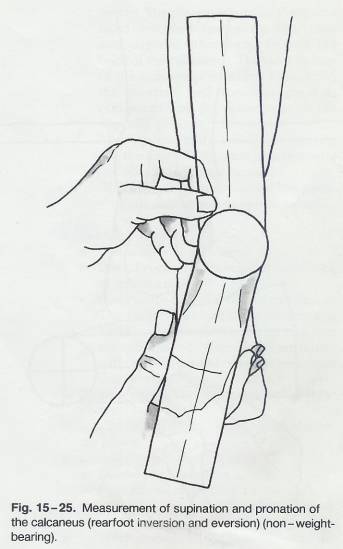
15.4.2.24 Figure 15-26
15.4.2.24.1
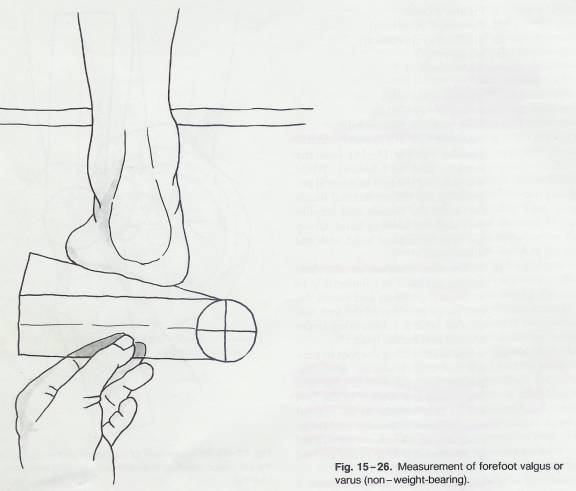
15.4.3 Arthrokinematics of the Ankle-Foot Complex
15.4.3.1 Ankle Mortise Joint
15.4.3.1.1 Summary
15.4.3.1.1.1 The anterior talus is 6mm wider than the posterior talus yet dorsiflexion does not separate the tibia and fibula more than 2 mm if at all. Both the anterior and posterior aspects of the talus are in a close, fit with tibial and fibular malleoli. How does such a wide anterior bone fit into a smaller posterior articular space? It is because the axis of talar motion is more medial than lateral, the lateral talar articulation is longer than the medial articulation, which means it moves a greater distance than the medial talus. The lateral talus rotates in a helical movement and there is movement of combined rolling and sliding which also changes the axis of movement positionally. Thus the final close packed position of full dorsiflexion results in only minimal tibular/fibular displacement.
15.4.3.1.2 The superior articular surface of the talus is wider anteriorly than posteriorly, the difference in widths being as much as 6 mm. The articular surfaces of the tibial and fibular malleoli maintain a close fit against the medial and lateral articular surfaces of the talus in all positions of plantar flexion and Dorsiflexion. As the foot moves from full plantar flexion into full Dorsiflexion the talus rolls backward in the mortise. It would seem, then, that with ankle Dorsiflexion the malleoli must separate in order to accommodate the greater anterior width of the talus. This separation could occur as a result of a lateral shift of the fibula, a lateral bending of the fibula, or both. However, it is found that the amount of separation that occurs between the malleoli during ankle dorsiflexion varies from none to only 2 mm, which is much less than would be expected considering the amount of wedging of the superior articular surface of the talus.
15.4.3.1.3 There appears to be a significant discrepancy between the difference in anterior and posterior widths of the trochlea of the talus and the amount of separation that occurs between the tibial and fibular malleoli with ankle dorsiflexion.
15.4.3.1.4 In understanding this apparent paradox, a closer look must be given to the structure of the trochlea and the type of movement the talus undergoes during ankle dorsiflexion. If both sides of the trochlea are examined it is evident that the lateral articular surface, which articulates with the fibular Malleolus, is longer in its anteroposterior dimension than the medial articular surface. The reason for this is that the lateral Malleolus moves over a greater excursion, with respect to the talus, during plantar flexion-dorsiflexion, than does the medial Malleolus. This is partly because the axis of motion is farther from the superior trochlear articular surface laterally than medially. The corollary to this (and this is true of essentially all joints with sellar surfaces) is that the relatively trackbound movement that the talus undergoes on plantar flexion-dorsiflexion at the ankle is not a pure swing, but rather an impure swing; it involves an element of spin, or rotation, that results in a helical movement.
15.4.3.1.5 Another way of conceptualizing this movement is to consider the talus as a section of a cone whose apex is situated medially rotating within the mortise about its own long axis, rather than a truly cylindrical body undergoing a simple rolling movement within the mortise. (Figure 15-17)
15.4.3.2 Figure 15-17
15.4.3.2.1
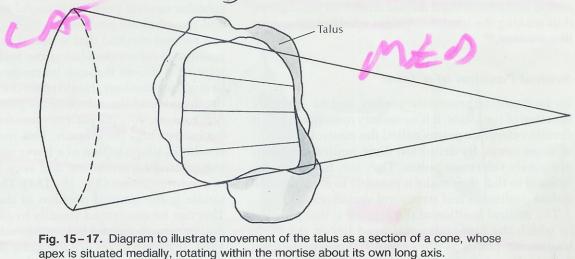
15.4.3.2.2 As a result of this, the intermalleolar lines projected onto the superior trochlear articular surface at various positions of plantar flexion and dorsiflexion are not parallel lines. Therefore, the degree of wedging of the trochlea does not reflect the relative intermalleolar distances in dorsiflexion and plantar flexion of the ankle. The true intermalleolar distances are represented by the length of these nonparallel lines projected onto the superior trochlear surface. The projected line with the foot in plantar flexion is only slightly shorter, if at all, than that for dorsiflexion and the necessary separation of the malleoli during dorsiflexion is minimal.
15.4.3.2.3 Up to this point, the ankle mortise joint axis has been considered as a fixed axis of motion. This has been done for the sake of simplicity and convenience using the approximate center of movement as the joint axis. No joint moves about a stationary joint axis. As indicated by instant center analysis of knee joint motion, this is true of the ankle mortise joint as well. Their surface velocities determined from the instant centers of movement show that when moving from full plantar flexion to full dorsiflexion there is initially a momentary distraction of the Tibiotalar joint surfaces, followed by a movement of combined rolling and sliding throughout most of the range, and terminating with an approximation of joint surfaces at the position of extreme dorsiflexion. These findings are consistent with the fact that the close packed position of the ankle mortise joint is dorsiflexion; the tightening of the joint capsule that occurs with movement of any joint into its close-packed position produces an approximation of the joint surfaces.
15.4.3.3 Subtalar Joint (Talocalcaneal)
15.4.3.3.1 Summary
15.4.3.3.1.1 From the outset, movement at this joint is somewhat difficult to conceptualize because the posterior articulation between the talus and calcaneus is concave superiorly on convex inferiorly, while the Anteromedial articulation is convex on concave. The posterior Calcaneal facet moving against the opposing concave talar surface can be compared with the radial head moving within the radial notch of the ulna. In at least some persons, this type of movement at the Subtalar joint is accompanied by a slight forward displacement of the talus during pronation and a backward displacement on supination, thus making the total movement a helical, or screw like motion.
15.4.3.3.2 As discussed previously, this is a compound joint with two distinct articulations. From the outset, movement at this joint is somewhat difficult to conceptualize because the posterior articulation between the talus and calcaneus is concave superiorly on convex inferiorly, while the Anteromedial articulation is convex on concave. Understanding talocalcaneal movement is perhaps facilitated by considering it analogous to movement at the proximal and distal Radioulnar joints. The Radioulnar joints, like the talocalcaneal joints, move in conjunction with one another and have only one degree of freedom of motion. The posterior Calcaneal facet moving against the opposing concave talar surface can be compared with the radial head moving within the radial notch of the ulna. As this movement occurs the Anteromedial facet of the talus must move in relation to the concave Anteromedial surface of the calcaneus, just as the head of the ulna must move within the ulnar notch of the radius at the distal joint of the forearm. In at least some persons, this type of movement at the Subtalar join t is accompanied by a slight forward displacement of the talus during pronation and a backward displacement on supination, thus making the total movement a helical, or screw like motion.
15.4.3.4 Neutral Position of a Joint
15.4.3.4.1 Summary
15.4.3.4.1.1 The neutral position of the first ray is that position in which the first metatarsal head lies in the same transverse plane as the central three metatarsal heads when they are at their most dorsiflexed position. Root and co-workers describe a neutral position of the Subtalar joint that is that position of the joint in which the foot is neither pronated nor supinated. From this position, full supination of the normal Subtalar inverts the calcaneus twice as many degrees as full pronation everts it. When the Subtalar joint is held in its neutral position there is no longer the ability for the midtarsal joint to pronate. According to James, the talar head in a pronated foot can be palpated as a medial bulge; in a supinated foot the talar head bulges laterally. The neutral position is usually present when the longitudinal axis of the lower limb and the vertical axis o f the calcaneus are parallel. A second method that is useful in the open-chain position involves visualizing and feeling the Subtalar joint as it moves through its range of motion. To begin, the examiner should place the ulnar surface of the thumb into the Sulcus of the patient's foot from pronation to supination and back again. This can be confirmed visually by observing the lateral curves above and below the Malleolus.
15.4.3.4.2 To facilitate arthrometric studies and to correlate function of the joints, it is necessary to assign to joints certain reference points called the neutral positions of those joints. By definition these neutral positions are purely reference points. They are, however, significant in that they make it possible to measure and define positional and structural variances.
15.4.3.4.3 The neutral position of the first ray is that position in which the first metatarsal head lies in the same transverse plane as the central three metatarsal heads when they are at their most dorsiflexed position. From this neutral position, the first metatarsal can move an equal distance above and below the transverse plane of the lesser metatarsal heads when the first ray is moved through its full range.
15.4.3.4.4 Root and co-workers describe a neutral position of the Subtalar joint that is that position of the joint in which the foot is neither pronated nor supinated. Another way to state this is the position from which the Subtalar joint could be maximally pronated and supinated. From this position, full supination of the normal Subtalar inverts the calcaneus twice as many degrees as full pronation everts it. Subtalar neutral is two thirds from inversion and one third from eversion of the calcaneus.
15.4.3.4.5 Clinically this is important since the Subtalar neutral position provides a foundation for meaningful and valid measurements and observation s to take place with respect to the foot and entire leg. It is not only a basis for meaningful communication but is also the foundation for the application of precise therapy, such as the fabrication of an effective biomechanical orthotic device. There is also a direct clinical correlation between the Subtalar joint and the midtarsal joint. When the Subtalar joint is held in its neutral position there is no longer the ability for the midtarsal joint to pronate. The Midtarsal is unable to dorsiflex, evert, or abduct even the Subtalar is in its neutral position. This position is termed the Normal locking position of the midtarsal joint.
15.4.3.4.6 According to James, the talar head in a pronated foot can be palpated as a medial bulge; in a supinated foot the talar head bulges laterally. In the neutral position the talar head can be palpated equally on the medial and lateral aspects of the ankle. The neutral position is usually present when the longitudinal axis of the lower limb and the vertical axis o f the calcaneus are parallel. This method for establishing the Subtalar neutral position is useful in both the open and closed-chain positions.
15.4.3.4.7 A second method that is useful in the open-chain position involves visualizing and feeling the Subtalar joint as it moves through its range of motion. To begin, the examiner should place the ulnar surface of the thumb into the Sulcus of the patient’s foot from pronation to supination and back again. This movement is very similar in shape to that of a horse saddle, being very abrupt toward pronation and very flat and shallow toward supination (Fig. 15-18a). The bottom of this saddle is the neutral position of the Subtalar joint. This can be confirmed visually by observing the lateral curves above and below the Malleolus (Fig. 15-18b). If these curves are the same depth, this is the accurate neutral position. If the curve below the Malleolus is deeper or shallower, then the foot is still in a pronated or supinated position and should be repositioned.
15.4.3.5 Figure 15-18
15.4.3.5.1
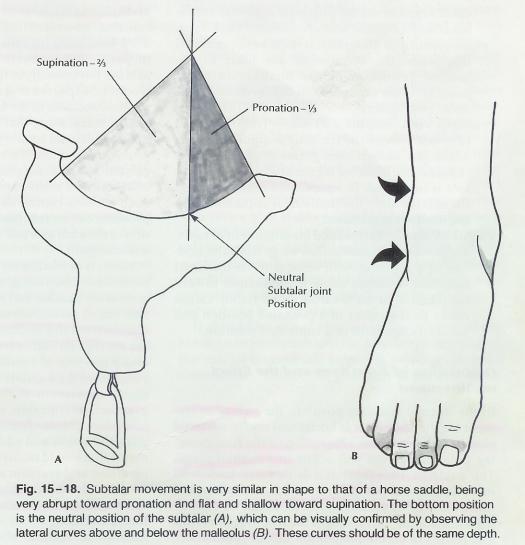
15.4.3.6 Transverse Tarsal Joints: Talonavicular and Calcaneocuboid Joints
15.4.3.6.1 Summary
15.4.3.6.1.1 Although the talonavicular joint is a ball and socket joint with potential multidirectional movement because the navicular is closely bound to the cuboid bone laterally, the movement allowed at the calcaneocuboid joint largely governs its freedom of movement. The axis of motion of most concern is the axis of pronation and supination. Such an orientation allows a movement of inversion-adduction-plantar flexion (supination) and eversion-abduction-dorsiflexion (pronation) of the forefoot. In the standing position, movement and positioning of the transverse tarsal joint occurs in conjunction with subtalar joint movement; when the subtalar joint pronates, the transverse tarsal joint supinates and vice versa.
15.4.3.6.2 Although perhaps some movement occurs between the cuboid and navicular, movement of these two bones is considered here as a unit with respect to the calcaneus and the talus. The configuration of the talonavicular articulation is essentially that of a ball and socket joint. Because of this configuration, it potentially has three degrees of freedom of movement, allowing it to move in all planes. However because the navicular is closely bound to the cuboid bone laterally, its freedom of movement is largely governed by the movement allowed at the calcaneocuboid joint. The calcaneocuboid joint, having a sellar configuration, has two degrees of freedom, each of which occurs about a distinct access of motion.
15.4.3.6.3 The axis of motion of most concern is the axis of pronation and supination. This axis is similar in location and orientation to the subtalar joint axis, the major difference being that it is not inclined as much vertically. It passes through the talar head, backward, downward, and laterally. Such an orientation allows a movement of inversion-adduction-plantar flexion (supination) and eversion-abduction-dorsiflexion (pronation) of the forefoot. In the standing position, movement and positioning of the transverse tarsal joint occurs in conjunction with subtalar joint movement; when the subtalar joint pronates, the transverse tarsal joint supinates and vice versa. Pronation of the forefoot close packs and locks the transverse tarsal joint complex, whereas supination results in loose packing and a greater degree of freedom of movement
15.4.3.7 Osteokinematics of the Ankle-Foot Complex
15.4.3.7.1 Terminology
15.4.3.7.1.1 At this point, some terms related to movements and positioning of various components of the ankle and foot must be clarified.
15.4.3.7.1.2 Inversion-Eversion
15.4.3.7.1.2.1 Movement about a horizontal axis lying in the Sagittal plane. Functionally pure inversion and eversion rarely occur at any of the joints of ankle or foot. More often they occur as a component of supination or pronation.
15.4.3.7.1.3 Abduction-Adduction
15.4.3.7.1.3.1 Movement of the forefoot about a vertical axis or the movement of the forefoot that results from internal or external rotation of the hindfoot with respect to the leg.
15.4.3.7.1.4 Internal-External Rotation
15.4.3.7.1.4.1 Movement between the leg and hindfoot occurring about a vertical axis. Pure rotations do not occur functionally but rather occur as components of pronation and supination.
15.4.3.7.1.5 Plantar flexion-Dorsiflexion
15.4.3.7.1.5.1 Movement about a horizontal axis lying in the plane corresponding to the intermalleolar line. Functionally, these usually occur in conjunction with other movements.
15.4.3.7.1.6 Pronation-Supination
15.4.3.7.1.6.1 Functional movements occurring around the obliquely situated subtalar or transverse tarsal joint axis. At both of these joints, pronation involves abduction, eversion and some dorsiflexion; supination involves adduction, inversion, and plantar flexion of the distal segment on the proximal segment. This is because these joint axes are inclined backward, downward, and laterally. It must be appreciated that when the metatarsals are fixed to the ground, pronation of the hindfoot (subtalar joint) involves supination of the forefoot (transverse tarsal joint).
15.4.3.7.1.7 Pronated Foot-Supinated Foot
15.4.3.7.1.7.1 Traditionally, a pronated foot (in the standing position) is one in which the arched configuration of the foot is reduced; the hindfoot is pronated while the forefoot is supinated. In a supinated foot (standing) the arch is high, the hindfoot is supinated, and the forefoot is pronated.
15.4.3.7.1.8 Valgus-Varus
15.4.3.7.1.8.1 Terms used for alignment of parts. Valgus denotes inclination away from the midline of a segment with respect to its proximal neighbor, whereas varus is inclination toward the midline. At the hindfoot and forefoot, valgus refers to alignment in a pronated position and varus to alignment in a supinated position.
15.4.3.8 Orientation of Joint Axes and the Effect on Movement
15.4.3.8.1 Summary
15.4.3.8.1.1 In the normal standing position, the axis of movement for the knee joint is horizontal and in a frontal plane. The ankle mortise joint axis is directed backward mediolaterally about 25° from the frontal plane and downward from medial to lateral about 10° to 15° from horizontal. Movement of the free foot about this axis results in combined plantar flexion, adduction, and inversion or combined dorsiflexion, abduction, and eversion. Note that the above statements relate the movements at the respective joints to the orientations of the joint axes when the foot and leg are swing feely. The obvious question in this regard would be; How is it possible to move both the tibia and femur in the Sagittal plane such as when performing a knee bend with the knee pointed forward, when movement is occurring at the ankle and knee about two nonparallel axes? Since the knee joint axis lies horizontally in the frontal plane, no problem would be expected there, since it is ideally oriented to allow rotation of the bones in the Sagittal plane. It would seem, then, that by performing such a knee bend an internal rotatory movement must be applied to the ankle, since the ankle joint axis I externally rotated with respect to the frontal plane. This apparent problem can be resolved by considering the orientation of the joint axis and associated movements at the subtalar joint. The average deviation from the midline of the foot is 23°, whereas the average deviation from the horizontal is 42°. Because the axis of motion for the subtalar joint deviates from the Sagittal plane and from the horizontal plane, movement at this joint involves combined eversion, dorsiflexion, and abduction or combined inversion, plantar flexion, and adduction. Subtalar movement is essentially uniaxial, so that any movement occurring at the joint may occur only in conjunction with its component movements, that is, abduction can only occur in conjunction with eversion and dorsiflexion the three together constituting pronation at the subtalar. Supination causes the calcaneus to assume a varus position, which, since the metatarsals remain flat on the ground, increases the twist in the foot and raises the arch.
15.4.3.8.2 In the normal standing position, the axis of movement for the knee joint is horizontal and in a frontal plane. With flexion and extension of the free-swinging tibia, movement will occur in a Sagittal plane. The ankle mortise joint axis is directed backward mediolaterally about 25° from the frontal plane and downward from medial to lateral about 10° to 15° from horizontal. Movement of the free foot about this axis results in combined plantar flexion, adduction, and inversion or combined dorsiflexion, abduction, and eversion. Note that the above statements relate the movements at the respective joints to the orientations of the joint axes when the foot and leg are swing feely. In this position, movements at one joint may occur independently of the other.
15.4.3.8.3 Therapists must be more concerned, however, with what happens when the foot becomes fixed to the ground and movement occurs simultaneously at the joints of the lower extremities. This is the situation during weight-bearing activities, or normal functional activities, involving the leg. The obvious question in this regard would be; How is it possible to move both the tibia and femur in the Sagittal plane such as when performing a knee bend with the knee pointed forward, when movement is occurring at the ankle and knee about two nonparallel axes? The heavy-weight lifter largely avoids the problem by pointing the knees outward, thus using external rotation and abduction at the hip.
15.4.3.8.4 This brings the knee and ankle axes closer to parallel alignment. The fact remains, however, that it is possible to perform a deep knee bend with the knee directed forward, and through a considerable range. Since the knee joint axis lies horizontally in the frontal plane, no problem would be expected there, since it is ideally oriented to allow rotation of the bones in the Sagittal plane. It would seem, then, that by performing such a knee bend an internal rotatory movement must be applied to the ankle, since the ankle joint axis I externally rotated with respect to the frontal plane. Surely ankle mortise joints cannot be expected to withstand such stresses during daily activities. This apparent problem can be resolved by considering the orientation of the joint axis and associated movements at the subtalar joint.
15.4.3.8.5 The axis of motion for the subtalar joint is directed backward, downward, and laterally. The degree of inclination and mediolateral deviation of the axis varies greatly among persons. The average deviation from the midline of the foot is 23°, whereas the average deviation from the horizontal is 42°. Because the axis of motion for the subtalar joint deviates from the Sagittal plane and from the horizontal plane, movement at this joint involves combined eversion, dorsiflexion, and abduction or combined inversion, plantar flexion, and adduction. Note that pure abduction and adduction of the foot are movements that would occur about a vertical axis and that inversion and eversion occur about a purely horizontal axis. Since the subtalar axis is positioned about midway between horizontal and vertical, it follows that movement about this axis would include elements of adduction-abduction as well as eversion-inversion.
15.4.3.8.6 Now again consider a situation of simultaneous knee and ankle flexion in the Sagittal plane with the foot fixed (deep knee bend). It was indicated that with such a movement an internal rotatory moment of the tibia on the talus would be applied to the ankle. Because the subtalar axis allows an element of movement about a vertical axis (rotation in the horizontal plane), this internal rotatory moment can be transmitted to the subtalar joint. Internal rotation of the tibia on the foot is, of course, equivalent to external rotation of the foot on the leg, which is referred to as abduction of the foot. Subtalar movement is essentially uniaxial, so that any movement occurring at the joint may occur only in conjunction with its component movements, that is, abduction can only occur in conjunction with eversion and dorsiflexion the three together constituting pronation at the subtalar. Thus with the foot fixed, simultaneous dorsiflexion of the ankle and flexion of the knee, keeping the leg in the Sagittal plane, requires pronation at the subtalar joint.
15.4.3.8.7 As a corollary to this, with such a movement, if pronation at the subtalar joint is restricted, and abnormal internal tibial rotatory stress will occur at the ankle mortise joint, an internal femoral rotatory stress will be placed on the knee, or both. The need for subtalar movement can be reduced by moving the leg out of the Sagittal plane (by pointing the knee outward), bringing the knee and ankle axes into closer alignment.
15.4.3.8.8 Similar considerations apply to the situation of a person rotating the leg over a fixed foot. Any rotation imparted to the tibia is transmitted to the subtalar joint (Fig. 15-19).
15.4.3.9 Figure 15-19
15.4.3.9.1
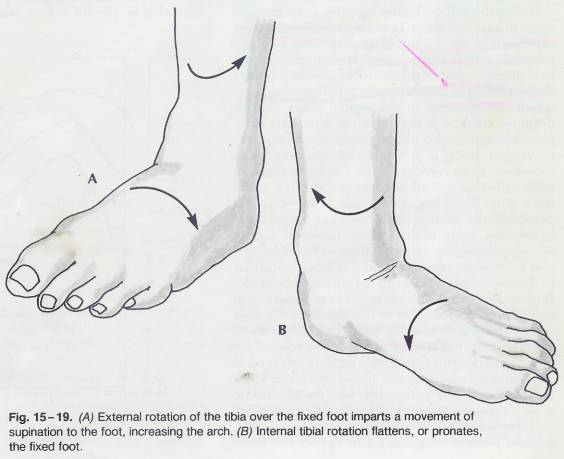
15.4.3.9.2 For example, if on rotates the leg externally over a foot that is fixed to the ground, the subtalar joint undergoes a movement of supination. This is analogous to movement about a mitered hinge; movement of one component about a vertical axis is transmitted to the second component as movement about a horizontal axis. Supination causes the calcaneus to assume a varus position, which, since the metatarsals remain flat on the ground, increases the twist in the foot and raises the arch. The opposite occurs with internal tibial rotation; pronation of the hindfoot causes a relative supination of the forefoot; the foot untwists and the arch flattens. This can easily be observed if one attempts to rotate the leg with the foot fixed to the ground. With respect to the structural alignment, then , a person with excessive internal tibial torsion will tend to have a pronated hindfoot (calcaneus in valgus position) and a forefoot that is supinated with respect to the hindfoot. The resultant untwisting of the foot causes a flatfoot on standing. The person with excessive external tibial torsion will tend to have a varus heel and a high arch.
15.4.3.9.3 The degree of twisting and untwisting of the foot also varies with stance width. When standing with the feet far apart, the heel tends to deviate into a valgus position with respect to the floor and the metatarsal heads remain flat; the metatarsals assume a position of supination with respect to the heel, thus untwisting the foot. The opposite occurs when standing with the legs crossed.
15.4.3.9.4 It should be noted that when standing with the hindfoot in pronation and the forefoot in supination the medial metatarsals assume a position closer to dorsiflexion. Since the joint axis of the first metatarsal is obliquely oriented (from Anterolateral to Posteromedial), dorsiflexion of the first metatarsal involves a component of abduction away from the midline of the foot.
15.4.3.9.5 Therefore, in a pronated foot, the first metatarsal is usually positioned in varus. On the other hand, a person with metatarsus primus varus, a condition in which the first metatarsal deviates into varus position, the foot will tend to assume a pronated position. This is because in order for the first metatarsal to be in a varus angle, it must also be in some dorsiflexion. This causes supination of the forefoot, which necessitates pronation of the hindfoot in order for the person to stand with the metatarsal head and calcaneus in contact with the ground.
15.4.3.10 Ankle and Foot During Gait
15.4.3.10.1 Summary
15.4.3.10.1.1 Clinicians must be concerned with the function of the joints of the ankle and foot during normal daily activities. The prime consideration here, of course, is walking. Again, because these are weight-bearing joints and because the foot becomes fixed to the ground during the stance phase, an understanding of the biomechanical interrelationships between these joints and the other joints of the lower extremity is necessary. During the gait cycle, the leg progresses through space in a Sagittal plane. Minimization of vertical displacement of the center of gravity is largely accomplished by angular movement of the lower extremity components in the Sagittal plane, that is, flexion-extension at the hip, knee, and ankle complex. The hip has no trouble accommodating such movement since it is multiaxial, allowing some movement in all vertical planes. The knee, although essentially uniaxial, allows flexion and extension in the Sagittal plane because its axis of movement is perpendicular to this plane and horizontally oriented. Movement of the tibia in a parasagittal plane over a fixed foot requires simultaneous movement at the subtalar and ankle mortise joints. Those muscles that affect movement at the ankle mortise joint also cross the subtalar joint, moving it as well. During the first interval, each of the segments of the lower extremity rotates internally with respect to its more proximal neighboring segment; the pelvis rotates internally in space, the femur rotates internally on the pelvis, and the tibia rotates internally on the femur. Much of this internal rotation is absorbed at the subtalar joint as pronation. Internal rotation of the leg with respect to the foot, occurring at the subtalar joint, makes the axis o the ankle mortise joint more perpendicular to the plane of progression. This is because the obliquity of the ankle axis, in the coronal plane, imposes a component of adduction of the foot during plantar flexion. At heel-strike, a moment-arm equal to the distance between the point of heel contact and the ankle joint develops. This results in some flexion at the knee, which is consistent with the fact that the tibia is rotating internally with respect to the femur. Through the early period of foot-flat, during which most of dorsiflexion occurs, the segments of the lower extremity continue to rotate internally. This occurs as supination at the subtalar joint. Consistent with this, the Peroneus longus muscle contracts, maintaining a pronated twist of the metatarsals and bring the foot as a whole toward its twisted configuration.Internal rotation of the talus with respect to the calcaneus occurs as pronation, while external rotation results in supination at the subtalar joint. Also, once the foot becomes flat on the ground, the metatarsal heads become fixed and the twisting and untwisting of the foot becomes dependent on the position of the hind foot. A relatively common condition that illustrates the biomechanical interdependency of the weight-bearing joints is femoral anteversion.
15.4.3.10.1.2
15.4.3.10.2 Clinicians must be concerned with the function of the joints of the ankle and foot during normal daily activities. The prime consideration here, of course, is walking. Again, because these are weight-bearing joints and because the foot becomes fixed to the ground during the stance phase, an understanding of the biomechanical interrelationships between these joints and the other joints of the lower extremity is necessary.
15.4.3.10.3 During the gait cycle, the leg progresses through space in a Sagittal plane. In order to minimize energy expenditure, the center of gravity must undergo minimal vertical displacement. Minimization of vertical displacement of the center of gravity is largely accomplished by angular movement of the lower extremity components in the Sagittal plane, that is, flexion-extension at the hip, knee, and ankle complex. The hip has no trouble accommodating such movement since it is multiaxial, allowing some movement in all vertical planes. The knee, although essentially uniaxial, allows flexion and extension in the Sagittal plane because its axis of movement is perpendicular to this plane and horizontally oriented. The ankle mortise join, however, cannot allow a pure Sagittal movement between the leg and foot because its axis of motion is not perpendicular t the Sagittal plane; it is rotated outward about 25°.During the normal gait cycle, however, movement between the foot and leg in the Sagittal plane does occur. This is only possible through participation of another joint, the subtalar joint. Movement of the tibia in a parasagittal plane over a fixed foot requires simultaneous movement at the subtalar and ankle mortise joints. This is consistent with the fact that no muscles attach to the talus. Those muscles that affect movement at the ankle mortise joint also cross the subtalar joint, moving it as well.
15.4.3.10.4 In considering the various movements occurring at each of the segments of the lower extremity during gait, it is convenient to speak of three intervals of stance phase; these are 1.) The interval from heel-strike to foot-flat 2.) Midstance (foot-flat), and 3.) The interval from the beginning of heel-rise to toe-off.
15.4.3.10.5 During the first interval, each of the segments of the lower extremity rotates internally with respect to its more proximal neighboring segment; the pelvis rotates internally in space, the femur rotates internally on the pelvis, and the tibia rotates internally on the femur. (Fig. 15-20a)
15.4.3.11 Figure 15-20
15.4.3.11.1
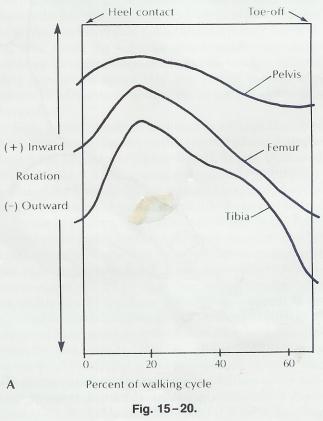
15.4.3.11.2
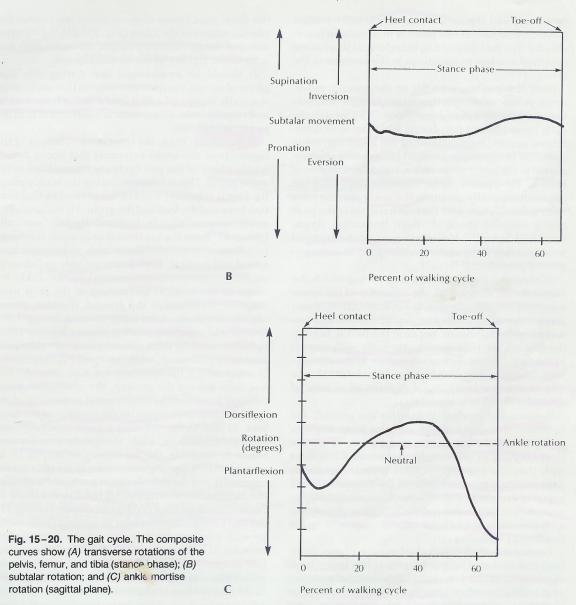
15.4.3.11.3
15.4.3.11.4 It follows that the entire lower limb rotates during this phase and that distal segments rotate more, in space, than the more proximally situated segments. At the point of heel strike, the foot becomes partially fixed to the ground, so that only minimal internal torsion between the heel and the ground takes place. Much of this internal rotation is absorbed at the subtalar joint as pronation (Fig. 15-20b). Internal rotation of the leg with respect to the foot, occurring at the subtalar joint, makes the axis of the ankle mortise joint more perpendicular to the plane of progression.
15.4.3.11.5 This allows the ankle mortise joint to provide for movement in the Sagittal plane, which, of course, is the plantar flexion occurring at the ankle during this interval (Fig. 15-20c). Note that the foot tends to deviate slightly medially in this stage of stance phase. This is because the obliquity of the ankle axis, in the coronal plane, imposes a component of adduction of the foot during plantar flexion.
15.4.3.11.6 At heel-strike, a moment-arm equal to the distance between the point of heel contact and the ankle joint develops. The reactive force of the ground acting on the foot at heel-strike across this moment-arm will tend to swing the tibia forward in the Sagittal plane. This results in some flexion at the knee, which is consistent with the fact that the tibia is rotating internally with respect to the femur. Knee flexion, form an extended position, involves a component of internal tibial rotation
15.4.3.11.7 Note that at heel-strike, the hindfoot moves into pronation while the tibialis anterior muscle contracts to bring the forefoot into supination. This causes the foot to untwist, the transverse tarsal joint to unlock, and the joints to assume a loose packed position. The foot at this point is in a position favorable for free mobility and is, therefore, at its greatest potential to adapt to variations in the contour of the ground.
15.4.3.11.8 Once the foot becomes flat on the ground, movement at the ankle mortise joint changes abruptly from plantar flexion to dorsiflexion. Through the early period of foot-flat, during which most of dorsiflexion occurs, the segments of the lower extremity continue to rotate internally. This rotation is transmitted to the joints of the ankle, since the foot is now fixed to the ground. Some internal rotation of the tibia automatically occurs at the ankle mortise joint during dorsiflexion with the foot fixed, since the joint axis is inclined about 15° from horizontal, downward and laterally. However, most of the internal rotation takes place at the subtalar joint as a component of pronation.
15.4.3.11.9 Throughout most of the period during which the foot is flat on the ground, the segments of the lower extremity rotate externally; the more distal segments rotate externally to a greater degree than their proximal neighbors. Again, because the foot is fixed to the ground, the tibia rotates externally with respect to the foot. This occurs as supination at the subtalar joint. The change during foot-flat, from internal rotation to external rotation, takes place after most of ankle dorsiflexion is complete.
15.4.3.11.10 Because the forefoot is fixed to the ground, the inversion occurring at the subtalar joint imposes pronation at the transverse tarsal joint, causing a close-packing or locking of the tarsus. Consistent with this, the Peroneus longus muscle contracts, maintaining a pronated twist of the metatarsals and bring the foot as a whole toward its twisted configuration. The foot at this point is being converted into an intrinsically stable lever capable of providing for the trust of pushing off.
15.4.3.11.11 During the final interval of stance phase, from heel-rise to toe-off, the segments of the lower limb continue to rotate externally. This external rotation of the tibia is again transmitted to the subtalar joint as supination of the hindfoot. With contraction of the calf muscle, the ankle begins plantar flexion, creating a thrust for push-off. This again creates a moment arm acting on the knee, this time moving the tibia into extension with respect to the femur. Note that this is consistent with the external rotation of the tibia occurring during this phase, since knee extension involves a component of external tibial rotation.
15.4.3.11.12 The extension of the metatarsophalangeal joints, occurring with heel-rise, causes a tightening of the plantar aponeurosis through a windlass effect, since the distal attachment of the aponeurosis crosses the plantar aspect of the joints. This tightening of the aponeurosis further raises the arch and adds to the rigidity of the tarsal skeleton.
15.4.3.11.13 It should be emphasized that during this final phase of stance, the joint movements that occur automatically convert the foot into a stable lever system and require little, if any, muscle contraction in order to accomplish this.
15.4.3.11.14 In summary, then, the transverse rotations of the segments of the lower extremity that occur during stance phase of the gait cycle are transmitted to the ankle joints. This is because during the stance phase the foot is relatively fixed to the ground so that rotation between the foot and the ground is minimal. The ankle mortise axis Is inclined slightly vertically (about 15° from the horizontal axis) while the subtalar joint axis is situated about midway between horizontal and vertical. Both joints are able to “absorb” rotatory movements transmitted to the ankle because of the vertical inclination of the joint axes. With the foot fixed to the ground, the tibia rotates slightly internally at the ankle mortise during dorsiflexion and externally during plantar flexion. Internal rotation of the talus with respect to the calcaneus occurs as pronation, while external rotation results in supination at the subtalar joint. Also, once the foot becomes flat on the ground, the metatarsal heads become fixed and the twisting and untwisting of the foot becomes dependent on the position of the hind foot. At heel-strike, the tibia rotates internally, pronating the hindfoot, while the tibialis anterior contracts to supinate the forefoot; this results in an untwisted foot. During midstance, as the tibia rotates externally and the subtalar joint gradually supinates, the foot becomes twisted. This twisting is further increased by tightening of the plantar aponeurosis. The twisted configuration results in maximal joint stability with minimal participation fo the intrinsic foot muscles. It is the twisted foot, then, that is best suited for weight-bearing and propulsion. During midstance there is little activity of the intrinsic muscles in the normal foot because the twisted configuration confers a passive, or intrinsic, stability on the foot. However, in the flatfooted person, considerably more muscle action is required since the foot is relatively untwisted. The flatfooted person must rely more on extrinsic stabilization by the muscles. An untwisted configuration is desirable in situations in which the foot must be mobile, such as in adapting to surface contours of the ground. Consistent with this is the fact that at heel-strike, the foot assumes an untwisted state in preparation for conformation to the contacting surface.
15.4.3.11.15 A relatively common condition that illustrates the biomechanical interdependency of the weight-bearing joints is femoral anteversion. A person with femoral anteversion must stand with the leg internally rotated in order to position the hip joint in normal (neutral) alignment. Conversely, if the leg is positioned in normal alignment with the patella facing straight forward, the hip joint assumes a position of relative external rotation. External rotation at the hip decreases the congruity of the joint surfaces.
15.4.3.11.16 During stance phase, as the femur externally rotates on the pelvis, the hip of the person with femoral anteversion will tend to go into too much external rotation. As the slack is taken up in the part of the joint capsule that pulls tight on external rotation, the joint receptors sense the excessive movement. To avoid excessive joint incongruity and to prevent abnormal stress to the joint capsule, the person with femoral anteversion must internally rotate during stance phase. This internal rotation is transmitted primarily to the subtalar joint, which is best oriented to accommodate transverse rotations. internal rotation at the subtalar joint causes pronation of the hindfoot; the foot untwists and the arch flattens. Thus, femoral anterversion predisposes to pronation of the foot. Also, because of the internal rotatory movement transmitted through the knee, femoral anteversion may also be a causative factor in certain knee disorders. For example, internal rotation imposed on a semiflexed knee causes the knee to assume an increased valgus position. This may predispose to patellar tracking dysfunction. Since there is a tendency for the person with femoral anteversion to walk with increased hip joint incongruity, the force of weight bearing is transmitted to a smaller area of contact at the articular surface of the hip. The result may be accelerated wear of the hip joint surfaces, perhaps leading to degenerative hip disease.
15.4.3.11.17 Femoral anteversion provides a good example of how a structural abnormality in one region may lead to localized biomechanical disturbances as well as altered mechanics at joints some distance away. This, again, is especially true of the lower extremity and should emphasize that when evaluating many patients with foot disorders it may be appropriate, if not necessary, to examine the structure and function of the knee, hip, and lower back. Conversely, foot or ankle dysfunction may precipitate disturbance in more proximal joint.
15.5 START
15.6 Examination
15.6.1
15.7
Ankle
Joint
Kendall 22
Back Table of Contents References
15.7.1.1 Type of Joint
15.7.1.1.1
15.7.1.2 Movements Permitted
15.7.1.2.1
15.7.1.3 Range of Movement
15.7.1.3.1
15.7.1.3.2
15.7.1.4 Description
15.7.1.4.1
15.7.1.5 Flexion and Extension
15.7.1.5.1 Flexion
15.7.1.5.2
15.7.1.5.3 Extension
15.7.1.5.4
15.7.1.6 Confusion
15.7.1.6.1
15.7.1.7 Measurement
15.7.1.7.1
15.8
Subtalar
Joint and Transverse Tarsal Joints Kendall 22
Back Table of Contents References
15.8.1.1 Type of Joint
15.8.1.1.1
15.8.1.2 Movements Permitted
15.8.1.2.1
15.8.1.3 Range of Movement
15.8.1.3.1
15.8.1.3.2
15.8.1.4 Description
15.8.1.4.1
15.8.1.5 Talonavicular Joint
15.8.1.5.1 Supination and Pronation
15.8.1.5.1.1
15.8.1.5.1.2 Supination
15.8.1.5.1.2.1
15.8.1.5.1.3 Pronation
15.8.1.5.1.3.1
15.8.1.6 Transverse Tarsal Joints
15.8.1.6.1 Adduction and Abduction
15.8.1.6.1.1
15.8.1.6.1.2 Adduction
15.8.1.6.1.2.1
15.8.1.6.1.3 Abduction
15.8.1.6.1.3.1
15.8.1.6.1.4 Inversion
15.8.1.6.1.4.1
15.8.1.6.1.5 Eversion
15.8.1.6.1.5.1
15.9
Metatarsophalangeal
Joints
Kendall 22
Back Table of Contents References
15.9.1.1 Type of Joint
15.9.1.1.1
15.9.1.2 Movements Permitted
15.9.1.2.1
15.9.1.3 Range of Movement
15.9.1.3.1
15.9.1.4 Description
15.9.1.4.1
15.9.1.5 Flexion and Extension
15.9.1.5.1
15.9.1.5.2 Flexion
15.9.1.5.3
15.9.1.5.4 Extension
15.9.1.5.5
15.9.1.6 Adduction and Abduction
15.9.1.6.1
15.9.1.6.2 Adduction
15.9.1.6.3
15.9.1.6.4 Abduction
15.9.1.6.5
15.10
Interphalangeal
Joints of Toes Kendall 22
Back Table of Contents References
15.10.1.1 Type of Joint
15.10.1.1.1
15.10.1.2 Movements Permitted
15.10.1.2.1
15.10.1.3 Range of Movement
15.10.1.3.1
15.10.1.3.2
15.10.1.4 Description
15.10.1.4.1
15.10.1.5 Flexion and Extension
15.10.1.5.1
15.10.1.5.2 Flexion
15.10.1.5.3
15.10.1.5.4 Extension
15.10.1.5.5
16 Temporomandibular Joint
17 Vertebral Column
17.1
Movements
of Vertebral Column Kendall 23
Back Table of Contents References