Advanced Clinical Therapy- A
New Approach
Copyright © February 2004 Ted Nissen
TABLE OF CONTENTS
4 Research Questions and Hypothetical Discussion
5 Single Case (Anecdotal) Studies
6 Clinical Assessment and Treatment
1 Introduction
1.1 Forward
1.1.1
We all seem to have a book in
us but the sad fact of hard copy printing, is that most books don’t find a
publisher and most that are published barely pay for the costs of publishing
let alone the for the writers time. Publishing is undergoing a not so quite
revolution with the prevalence of fast (DSL) online Internet access because for
better or worse anyone with an Internet connection and Web Hosting can put
their ideas to electronic print. The following is a work in progress. That
means as I write it I will post it on the Web for your review. There may be
misspellings, missing sections, theoretical missteps, awkward phrases, grammatical
lapses and inevitable misinformation, which occur without a good editor. With
your patience, It is hoped you will find this information useful and
insightful. It represents more than 30 years of massage practice, a very
curious mind, and a sincere desire to help other massage practitioners. If you
would like to help me with this project use this link. Web Site Help For more information on the volunteer
positions needed in creating this site. Information
Ted Nissen Long Beach California February 2004
1.2 Preface
1.2.1 This is an online textbook for the Massage and related professions meant to describe a theoretical perspective and novel assessment protocols, which will assist the soft tissue therapist, apply currently known techniques to areas of irritation, which are the root cause of common soft tissue disease. Soft tissue disease causes significant health problems and much pain and suffering to many patients. Soft Tissue Therapy when applied to these small areas is expected to increase the curative effect of soft tissue treatments. Although other soft tissue therapists (Chiropractors, Physical Therapists ect) may find the conceptual constructs and assessment protocols useful massage therapists would benefit most because they simply have more time to spend with patients. The assessment techniques are time consuming and lend themselves better to the Massage Therapy Profession.
1.2.2 The massage therapist has a face to many Americans and is no longer a shady character in some sleazy massage parlour. With the depiction of the massage therapist in many popular TV shows (Friends ect) and with the advent of chair massage in offices and businesses many people now feel comfortable going to a massage therapist for their aches and stress. Given this popular support, insurance companies are beginning to pay claims with the massage therapist as sole provider (Blue Shield). State licensing of the massage therapist should improve the quality of patient care and replace archaic punitive municipal laws in the regulation of the massage therapy profession. This professional evolution can be seen in other professions such as Chiropractic and Nursing by example.
1.2.3 Massage is still thought of as a palliative treatment for stress and for temporary relief of minor aches and pains. The Spa industry is probably the major employer of massage therapists although Chiropractic, Physical Therapy Centers and Hospitals employ in lesser but significant numbers. Vocational schools do a very good job at Training students in basic technical knowledge and massage techniques used in the Spas and clinics. Traditional Vocational Education evolved as way of training students who did not plan for University training for a professional career. Vocational schools are businesses, which provide the business community with semi skilled workers to meet the demands of their customers.
1.2.4 In addition to this trend are more experienced massage therapists who are applying massage techniques to Orthopaedic and other medical problems. Sports massage evolved as an effective treatment for sports injuries and as a way to improve athletic performance. Orthopaedic Massage is taught in some Massage Schools and has a small but growing support.
1.2.5 Another trend is an interest in developing a body of research data on the effects of massage therapy on a variety of common ailments.
1.2.6 This textbook will provide a useful theoretical perspective and novel assessment protocols to Vocational school teachers/students, Experienced massage therapists, and massage researchers.
1.3 Why Do Research?
1.3.1 Massage although increasingly popular with the general public is still viewed with considerable controversy by the medical community. Negative associations with “laying on of hands” conjure up notions of charlatanism and since many prostitutes still use massage parlours as a front for their business questionable morality is added to the mix. The trend toward state licensing of massage therapists along with Massage Therapy Associations strong support for ethical standards may serve to counterweight these negative associations.
1.3.2 Even with these considerations aside the value of massage therapy, if any, is frequently felt to be of a psychological nature or the result of the placebo phenomenon. Worse, those who have advocated the use of massage for non-scientific or non-physiological mechanisms that the medically oriented professional cannot always accept. Reflex zones, trigger points, fibrositic nodules, and meridians have all been identified as areas to which massage may be directed, but have never been identified as true anatomical or physiological entities. Massage may also be recommended for conditions, which by themselves do not warrant its use such as pain, for conditions that are not proven to respond to massage therapy such as obesity, or for clinical entities that do not exist, such as cellulite removal.
1.3.3 In addition, there is little empiric or direct scientific evidence for the efficacy of massage. Massage tends to be used on the basis that it "seems to work;" it makes the patients feel better. So, while there is little question among clinicians who employ massage as therapeutic measure that it has some value, its value is not well documented. This is primarily because massage is often used for the relief of painful conditions in which there a few associated pathological signs. This makes reliable measurement of the possible effects of treatment a difficult problem in research design methodology and technology. While massage may certainly provide temporary pain relief in many conditions, it does not necessarily contribute to the long-term relief of pain, which requires resolution of the pathological state.
1.3.4 The result of the prevailing attitudes towards massage is that it is often not used in the treatment of some conditions for which it might have a significant therapeutic effect.
1.3.5 Massage may be more readily justified and rationalized in the following instances, where it may have a direct or indirect of effect upon the pathological state.
1.3.5.1 Deep stroking in the presence of certain edematous conditions may assist in the resolution of fluid accumulations.
1.3.5.2 A variety of massage techniques can be used to reflexively promote muscle relaxation for more effective mobilization of a part. This may certainly be useful when abnormal muscle tension is an important factor in the perpetuation of the pathological process
1.3.5.3 Deep frictions and kneading types of massage may assist in restoring mobility between tissue interfaces or may increase extensibility of individual structures.
1.3.5.4 Massage also tends to increase circulation to the area treated, which may be desirable in certain cases.
1.3.5.5 These effects are generally well described in traditional massage textbooks along with descriptions of related massage techniques. [1] [2] [3] [4]
1.3.5.6 Transverse friction, Ischemic Compression and other techniques to tendons and ligaments. [5] [6] [7] [8]
1.3.6 Research is needed for pathologies per above that might reasonably respond to massage treatments to determine if any curative benefit is achieved.
1.4 What is Science?
1.4.1 Systematic prolonged study, observation, Theoretical Modelling, Experimentation, predictive/descriptive conclusions corroborative verification and willingness to abandon cherished theory when the evidence doesn’t support it. Pythagoras (6th Century BC), Galileo (1564-1642 ad), and Ben Franklin are examples.
1.4.2 The Pythagorean discovery that the pitch of a note depends on the length of the string which produces it, and that concordant intervals in the scale are produced by simple numerical ratios (2 : 1 octave, 3 : 2 fifth, 4 : 3 fourth, etc.), was epoch-making: it was the first successful reduction quality to quantity, the first step towards the mathematization of human experience – and therefore the beginning of Science. The Pythagorean theorem showed us how mathematics can reveal relationships in shapes that confound our eyes. There is no obvious relationship between the lengths of the sides of a right-angled triangle; when we build a square over each side, the areas of the two smaller squares will exactly equal the area of the larger. In such wonderfully ordered laws, hitherto hidden from the human eye, could be discovered by the contemplation of number shapes, was it not legitimate to hope that soon all secrets of the universe would be revealed through them?
1.4.3 Galileo constructed a working model of the solar system with elliptical planetary orbits and a light source at the center and from the vantage point of the earth drew the phases of Venus on a piece of paper as it revolved around the light source. With a telescope he then observed Venus as it revolved around the sun and likewise drew it. The drawings of the phases of Venus were the same from the model and the actual observations demonstrating by analogy the elliptical orbits of plants around the sun.
1.4.4 For centuries, the devastating scourge of lightning had generally been considered supernatural phenomena. During a 35-year period in Germany alone during the mid 1700's, 386 churches were struck and more than a100 bell ringers killed and in Venice some 3000 people were killed when tons of gunpowder stored in a church was hit. Ben Franklin in journal he kept for its experiments noted the similarities between the sparks produced by an electrostatic device and the look, shape, and even smell of lightening. in June 1752 49 year old Ben Franklin and is 21 year old son William chased lightning strikes in the Philadelphia farm fields. Franklin had fashioned the silk kite with a sharp metal wire attached. At the end of the string which held the kite high in the air he attached a metal key which drew the charge from a lightening strike down the wet string through the key into a Leyden Jar (primitive battery). Later he was able to use the electrical charge in the battery to cook a Turkey. These discoveries prompted the installation of lightening rods which drew the destructive electrical charge of the lightening harmlessly into the earth.
1.5 Profession Vs. Vocation
1.5.1 Professionals solve societal problems whose resolution is highly valued and whose professional practice requires academic institutional support and scientific (prolonged systematic) study. These are problems that can not readily be resolved by the uninitiated with trial and error problem solving
1.5.2 A vocation
2 Theoretical Perspectives
2.1 Introduction
2.1.1 There are a plethora of massage techniques but few theoretical models, which inform the massage profession. Technique tells us how we might fix it but not why it is broken. Theory suggests a broad range of techniques many of which would be undiscovered without theory (Structural Integration spawned Heller Work Ect.). Theory asks the simple question “why is something so?” It is the analysis of a set of speculative facts in their relation to one another with the hope of answering the WHY questions. Our clients come to us because they experience some measure of discomfort (emotional and or physical) from the mild to excruciating. The question which we can then ask is “Why do we hurt?”. In addition to being descriptive, a theory should predict objective observable phenomena, which others can witness. These are anecdotal accounts of others in the profession or patients who have witnessed or can report the outcomes. It is called anecdotal because it is unscientific in that your data is based on observations of unscientific observers. This is where theory comes to life. This anecdotal evidence pro and con is the meat and substance of theory. The purpose of this section is to outline a theoretical model (Theoretical Model Why Do We Hurt?) with scientific references Literature Review, predictive outcomes and suggest a disease process, assessment, technique and treatment. Thus begins the discourse for lively scientific debate. If the Massage Therapy Profession is to join the scientific community of soft tissue professionals, we are benefited in our discussions when we can reference a theoretical model, which shares a common language with other professions.
2.2 Visualization of Theoretical Perspective
Theoretical Model-Why Do We Hurt?
2.3 Core Theory (Descriptive and Predictive)
2.3.1 Summary
2.3.1.1 A significant degree of patient discomfort and dysfunction after novel, repetitive or over activity can be caused by small areas of irritation and ischemia (Inflammatory, metabolic and or neurological Etiology) near where the ligaments and tendons attach to the bone or at biomechanical stress points along their course. It is expected that this root cause will be much more prevalent than the usual explanations or Diagnosis by soft tissue professionals (Medical Doctors, Physical Therapists, Chiropractors, Sports Doctors and others) for the pain phenomena post exercise or activity soreness (Sprain/Strain, DOM, Trigger Points, Subluxation ect). These areas of irritation are created in response to novel, repetitive or over activity. Symptoms and tissue sensitivity seem to increase with age and with the presence of other pathologies such as Osteoarthritis, Degenerative Disc Disease, Diabetes, and stress. These areas of irritation refer distally in predictable and observable patterns causing a wide array of symptoms from headaches to muscle weakness, trigger points and postural dysfunction.
2.3.1.2 Simple palpation techniques (dermatomal, sclerotomal, myotomal, and extrasegmental), range of motion assessment, postural assessment and muscle testing are but a few of the assessment techniques which can point to areas which would benefit from soft tissue treatment.
2.3.1.3 Massage Therapy can increase the circulation of blood and lymph fluid to and from these relatively discrete areas thereby relieving not only the symptoms but also the cause of the problem. Examples of typical areas of irritation are; Glenohumeral Tendon attachments, Muscle tendon attachments to the medial superior scapular angle, Cervical Facet Ligaments, Cervical Spinal Ligaments, Lower lumbar spinal and facet ligaments, Deep Hip Rotators tendon attachments, and sacroiliac tendon and ligament attachments. Simple palpation techniques, range of motion assessment, postural assessment and muscle testing are well suited to the massage environment and can define the areas of therapeutic treatment. Massage treatments such as ischemic compression, stripping massage and therapeutic stretching are effective treatments with curative effects to primary and secondary treatment areas.
2.3.2 Detailed Discussion
2.3.2.1 Root Cause of Post Activity Nociceptive Phenomena
2.3.2.1.1 A significant amount of muscle tension, pain and dysfunction that the average person experiences after novel, repetitive or over activity is caused by irritation of the afferent sensory nerve fibers which supply the tendon and ligament cells near where they attach to the bone or at biomechanical stress points along their course. Gutstein-Good[9] [10] It is expected that this root cause will be much more prevalent than the usual explanations or Diagnosis by soft tissue professionals (Medical Doctors, Physical Therapists, Chiropractors, Sports Doctors and others) for the pain phenomena post exercise or activity soreness (Sprain/Strain, DOM, Trigger Points, Subluxation ect).
2.3.2.2 Hume’s Fork- Tendon and Ligament Metabolic Stress
2.3.2.2.1 The tendon and ligament cells near where they attach to the bone receive greater stress than the other cells of the tendon or ligament because of their proximity to the bone, which is being pulled by opposing muscles. In the tradition of analytic empiricism promulgated by the 18th century Scottish philosopher, David Hume (Hume’s Fork) the following simple experiment will reveal these stresses. If you cut a strip of paper ¼ to 1/3 of an inch thick and affix one end to a stable surface while pulling on the other end the following result should occur. Assuming the paper strip is equally strong in all its parts, the strip of paper will break more frequently on either end of the paper strip. That is near where your pinched fingers are pulling (the paper breaks more commonly at this site) or where you have affixed the other end. In the case of ligament cells, both ends of their attachments are vulnerable to the stresses of movement and receive greater metabolic demand. In the case of tendon cells only the cells near the bone seem prone to irritation probably because the tendon cells which interdigitate with the muscle cells have a better blood supply than the cells near the bone. Biomechanical stress points are usually areas of a tendon which receive greater stress because they are being pressed on by other structures such as bone and or soft tissue (this may occlude blood supply) or flexed repetitively (this may transfer mechanical stress to the apex of the flexing action). An example is at the Talocrural joint where the posterior tendons of plantar flexor muscles are repeatedly flexed and in the case of the tarsal canal muscles (flexor hallucis longus, tibialis posterior, flexor digitorum longus) pressed against the dome of the calcaneus. In the case of the Achilles tendon this biomechanical stress point is 3 to 5 cm proximal to the insertion onto the calcaneus as this is the most common site of Achilles tendonitis. Repetitive activities such as such as running and or walking repeatedly flex and straighten the tendon so that the cells in tendon and ligament cells (fibroblasts) in this area of the tendon receive greater stress in a similar manner to the cells near where the tendon and ligament attach to the bone. To demonstrate this principal with the above-defined strip of paper if you repeatedly flex and straighten the strip and then affix one end to a stable surface while pulling on the other end the following result should occur. The paper strip will break at the apex of the flexing action. This apex of the paper strip is the biomechanical stress point
2.3.2.3 Fixed Vascular Supply
2.3.2.3.1 The blood and lymph supply to these tendon and ligament cells is probably fixed based on the usual activity of the person. When a patient becomes more active (Over activity), initiates a new movement (Novel Activity), or repeats a movement more times than usual (Repetitive Activity) the tendon and ligament cells need more oxygen, glucose, and protein to survive.
2.3.2.4 Increased Metabolic Demand can result in Cell stress and or Death
2.3.2.4.1 Since the body cannot meet the cells metabolic demand they either die or the demand on the cells must be reduced. That is the person must become less active. How would anyone know to become less active unless they received a distress call from the overworked tendon and ligament cells? Cells can get stressed out to you know.
2.3.2.5 Distress Call from Overworked Tendon and Ligament Cells (Reflex ARC) (Sympathetic Afferent Over stimulation)
2.3.2.5.1 The body has an ingenious way of doing this by decreasing the blood flow to the cells. The Sympathetic Nerves become over stimulated. Perhaps as yet unknown chemical messengers from the overworked tendon and ligament cells cause this over stimulation (Afferent Fibers from blood vessels supplying muscle and tendon cells near bone attachments) The efferent fibers of the sympathetic nervous system constrict the muscles around the arterial walls (vasoconstriction) and the blood flow to the cells is reduced (ischemia). Revis [11] This is what is known as a Reflex Arc. Incoming sensory stimulation (Afferent Fibers) from the viscera triggers a response from the spinal cord, which in turn sends its response to the viscera (Efferent Fibers). This is very similar to overloading electrical circuits, which trigger a fuse to shut down the power.
2.3.2.6 Increased Concentration of Metabolites Irritate Afferent Sensory Nerve Fibres (Ischemia)
2.3.2.6.1 This reduces the flow of the metabolic waste out of the area and increases the concentration of these wastes resulting in irritation of the afferent sensory nerve fibers resulting in Nociceptive (Uncomfortable, Noxious) Example Kellgren[12] The patient is thereby informed to reduce the activity level.
2.3.2.7 Cell Death
2.3.2.7.1 If the person does not reduce their activity level, the cells in these areas may die in sufficient numbers and produce a higher concentration of enzymatic chemicals.
2.3.2.8 Inflammatory Chemicals (Enzymatic Trigger)
2.3.2.8.1 These enzymes initiate the production of inflammatory chemicals from the cell walls of the local vessels (blood and Lymph?).
2.3.2.9 Vessels Become Porous
2.3.2.9.1 These inflammatory chemicals (Kinin System, Prostaglandins and Leukotrienes ect) decrease the size of the cells, which comprise the walls of these vessels. These or other chemicals may also initiate the relaxation of muscles surrounding the vessels resulting in vasodilation. Revis [13]
2.3.2.10 Decreased Concentration of Metabolic Waste (Edema)
2.3.2.10.1 Fluid from the blood and lymph system flows out of the vessels in greater volume because the opening in the vessel walls has increased (vasodilation) and the vessels have become more porous. This fluid flows to the areas with less interstitial fluid (osmosis) around the tendon and ligament cells and helps decrease the concentration of metabolic waste.
2.3.2.11 Temporary Reduction in Nociceptive Sensory Phenomena
2.3.2.11.1 This may temporally reduce the excitation of the afferent nerve fibers. This reduced excitation will be short lived.
2.3.2.12 Inflammatory Chemicals Irritate Afferent Sensory Nerves
2.3.2.12.1 Afferent Sensory Nerve fibers are excited by the increased concentration of inflammatory chemicals. This nerve irritation may result in Nociceptive (Uncomfortable, Noxious) Sensory Phenomena Example. The patient is thereby informed to reduce the activity level.
2.3.2.13 Lymphatic System (Macrophages) carries away Dead Tendon and Ligament Cells
2.3.2.13.1 Because vessel walls become more porous, large lymphatic cells (macrophages) are able to travel in and out of the area of injury to retrieve and carry away dead ligament and tendon cells.
2.3.2.14 Inflammatory chemicals Encourage New Vessel Growth
2.3.2.14.1 Inflammatory chemicals may have the additional benefit of encouraging the growth blood vessels, which will increase the blood supply and allow for greater future activity (Exercise Adaptation).
2.3.2.15 Activity Level Remains the Same
2.3.2.15.1 If the person continues their activity level, the problems will be exacerbated.
2.3.2.16 Increased Cell Death
2.3.2.16.1 , Cells in these areas will continue to die.
2.3.2.17 Increased Concentration of Inflammatory Chemicals
2.3.2.17.1 Cell Death will result in higher concentration of enzymatic chemicals and resultant increase in inflammatory chemicals.
2.3.2.18 Referred Sensory Phenomena
2.3.2.18.1 Afferent Sensory Nerve fibers are excited by the increased concentration of inflammatory chemicals. This nerve irritation may result in Nociceptive (Uncomfortable, Noxious) Sensory Phenomena Example The patient is thereby informed to reduce the activity level.
2.3.2.19 Increased Skin Conductance
2.3.2.19.1 The area of ischemia or inflammation because it excites the area nerve supply should be detectable by surface instruments that measure skin conductance. The surface of the skin will become moister over these areas and thus conduct an electrical impulse more readily. This along with the palpation assessment methods outlined below can provide researchers with prima facie evidence of underlying pathology. Travell J [14]
2.3.2.20 Referral Patterns, Nociceptive Phenomena, and Clinical Observations
2.3.2.20.1 The irritated nerves refer distally in predictable and observable patterns (dermatomally, sclerotomally, myotomally, and extrasegmentally, and or Trigger Point Referral Zones) Kellgren [15] causing a wide array of Nociceptive (Uncomfortable, Noxious) Sensory Phenomena eg (Pain, headaches, sweating, blanching, and nausea, (sometimes referred Cutaneous Paresthesia and numbness instead of deep pain). Inman VT, Saunders JB [16] Clinical Phenomena may be observed (Muscle weakness, trigger points, postural dysfunction) Most objective clinical measures may not reveal the underlining disease process
2.3.2.21 Differential Assessment
2.3.2.21.1 Cell death is accelerated and sympathetic nervous system hypersensitivity is exacerbated when the clinical picture is complicated by other disease processes such as degenerative disc disease, Postural Faults, Osteoarthritis, stress, fibromyalgia, Lyme disease, diabetes, and other organic dysfunction to name some by example. Practitioners would need to rule out other organic disease, which can mimic soft tissue dysfunction symptoms before a tentative conclusion is reached regarding a course of soft tissue treatment. Stress can also accelerate cell death by reducing blood circulation to tendon and ligament cells.
2.3.2.22 Massage Therapy
2.3.2.22.1 Soft Tissue Therapies such as Massage Therapy is effective to the extent that it increases circulation to these relatively small areas of metabolic dysfunction with ancillary treatment to the distal referral zones where secondary and tertiary dysfunction such as muscular weakness and trigger points can further complicate the clinical picture. Massage may be more effective when superficial structures can be accessed with ischemic compression or other massage techniques.
2.3.2.23 Assessment Techniques
2.3.2.23.1 Simple Assessment Techniques can direct therapy to discrete areas of irritation which increases the effectiveness of massage treatment Palpation techniques include; nerve referral areas (dermatomal, sclerotomal, myotomal, and extrasegmental), range of motion assessment, postural assessment and muscle testing. These assessment techniques can point to but not necessarily confirm the areas, which would benefit from soft tissue treatment.
2.3.2.24 Laboratory Tests
2.3.2.24.1 Sed rates (erythrocyte sedimentation rate [ESR])may be elevated when inflammation is pronounced but largely most objective clinical measures may not reveal the underlining disease process. MRI imaging is will probably not reveal any underlying pathology.
2.3.2.25 Typical Areas of Irritation
2.3.2.25.1 Glenohumeral Tendon attachments
2.3.2.25.1.1 Refers pain into the temporal area of the skull-Headache Symptoms
2.3.2.25.2 Cervical Facet Ligaments
2.3.2.25.2.1 Refer pain extrasegmentally into the upper back
2.3.2.25.3 Cervical Spinal Ligaments
2.3.2.25.3.1 Refers pain dermatomally depending on the spinal level into the neck shoulders and arms
2.3.2.25.4 Lower lumbar spinal and facet ligaments
2.3.2.25.4.1 Refer pain extrasegmentally and according to spinal level dermatomally, can cause postural faults and muscle weakness in hamstrings
2.3.2.25.5 Deep Hip Rotators tendon attachments
2.3.2.25.5.1 Refers into the lower back and down the L5 and S1 Dermatome into the hamstrings and fascia lata
2.3.2.26 Collagen Fiber Pathology
2.3.2.26.1 Extracellular matrix materials produced by the fibroblast (Tendon and Ligament Cell) include dense regularly arranged collagenous (kola=glue) protein fibers that form a zig zag pattern (allows flexibility=think Chinese finger trap) and are arranged longitudinally along lines that they are habitually pulled. When healthy these fibers provide extensibility (they give a little-flexibility) and resistance to force. There is interfiber mobility between the collagen protein strands and extrafiber mobility between the bundled collagen fibers and other tissues. When the force applied to these collagen fibers is not too excessive or novel and nutrition to the fibroblast cell is adequate, damaged collagen fibers are ingested by the fibroblast cell, which produces collagen precursors, that, in response to imposed stresses, polymerize into collagen fibers. These collagen fibers mature with the same zig zag pattern, intra and extra fiber mobility, extensibility, and resistance to force as their neighbors and align longitudinally with any novel direction of pull. This hypertrophic response to gradually increasing force and novelty to the tendon and ligament tissue does not produce cell stress, death, pain or inflammation.
2.3.2.26.2 If the force applied to the tendon and ligament fibers is too great or the direction of pull too dramatic (novelty) and the nutrition to the fibroblast cell inadequate several pathological conditions may result.
2.3.2.26.2.1 Ligament/Tendon Sprain/Strain
2.3.2.26.2.1.1 This is macrodamage to the tendon and ligament tissue where massive numbers of collagen fibers are ripped apart. This may involve a partial or complete rupture of the tendon and ligament tissue such as Achilles tendon rupture or anterior talofibular ligament sprain. Precipitating factors may include a history of tendon and or ligament pathology.
2.3.2.26.2.2 Cell Stress
2.3.2.26.2.2.1 As previously mentioned, fibroblast cell stress may result in vasoconstriction to the area. This could further compromise the nutritional status of the cell. The fibroblasts ability to produce healthy collagen fibers may be compromised. Collagen fibers may not mature properly. The zigzag pattern of the collagen protein may be absent affecting the fibers extensibility this may result in susceptibility to micro damage resulting increased concentration of protein particulate matter which the fibroblast cell may not be able to ingest. This may begin an inflammatory process with ensuing symptomatic consequences. Interfiber bonds (adhesions) between the collagen fibers and extra fiber bonds between the collagen fibers and other tissues may also develop. Loss of extensibility, reduced resistance to force, increased susceptibility to micro damage and increased inflammation is the likely result.
2.3.2.26.2.3 Cell Death
2.3.2.26.2.3.1 Fibroblast cell death may mean loss of the capacity of the tissue to hypertrophy, increased micro damage to the collagen fibers, loss of extensibility and resistance to force and most certainly an increase of local inflammation with attendant painful symptoms.
2.3.2.27 Myofascial Trigger Points
2.3.2.27.1 An increased incidence of Myofascial Trigger Points may result from connective tissue pathology and dysfunction. An example of this is found when the tendinous attachment of the infraspinatus develops pathology near its attachment to the posterior aspect of the humerus. Infraspinatus TP 1-3 become hyperirritable and refer in the characteristic pain pattern for that muscle.
3 Literature Review
3.1 Muscles and Tendons
3.1.1 Kellgren [17] injected 0.1-0.3 ml of 6% hypertonic saline solution into muscle tissue and found that pain was referred distally from the original injection site.
3.1.2 Kellgren[18] also found that pressure to sensitive areas of the muscle tissue in patients with "fibrositis" (Myofacial Trigger Points) reproduced the patients reported pain symptoms. After Kellgren identified the pain patterns created by these injections he identified in reverse these problem areas based solely on patient complaints. The spot tenderness was often remote from the patients reported pain and the area around that point was not painful to the patient. When that spot was injected with procaine, the patients reported pain was relieved.
3.1.3 Travell[19], Good[20] and Kelly[21] reported similar findings. In 1967, Hockaday and Whitty[22] confirmed Kellgren's principle findings.
3.1.4 These tender spots sometimes referred cutaneous paresthesias and numbness instead of deep pain[23].
3.1.5 Myofascial referred pain did not always follow dermatomal[24], myotomal[25] or sclerotomal[26] patterns of innervation[27][28].
3.1.6 Travell & Simons[29] outline several causative factors of myofascial trigger points including; Direct: Acute overload, Repetitive stress, Chilling, and Gross Trauma. Indirect: Organ/Joint Disease, Other trigger points and emotional distress.
3.1.7 Trigger Points are a region of muscle tissue, which is ischemic and or is metabolically elevated from surrounding tissues. Poor circulation would mean that there would be poor heat distribution and thus the greater the temperature of the Trigger Point. For example when a needle thermocouple is first injected into a TP the temperature is higher than that of the surrounding tissue but after 15-20 seconds lowers to that of the surrounding tissue[30]
3.1.8 Popelianskii, et al.[31] measured the rate at which radioactive[32] NaI was eliminated from tissue in the clinically affected area. They reported a distinct prolongation of the resorption rate of the isotope, which they interpreted as due to impaired local circulation.
3.1.9 These trigger points can exist in a latent form for decades, become periodically active restricting range of motion causing varying degrees of disability from mild to severe. One session using a variety of treatment modalities, which restore circulation to the ischemic area in the muscle, can eliminate the TP permanently[33].
3.2 Fascial and Ligamentous Trigger Points
3.2.1 Kellgren [34] injected the fascial epimysium of the gluteus medius muscle with 0.1 ml of 6% saline solution which referred pain several centimeters distally. The tendon of the tibiallis anterior, similarly injected, referred pain to the medial aspect of the ankle and instep.
3.2.2 Travell[35] reported that ankle and foot pain subsequent to an acute ankle sprain was caused by four TPs in the joint capsule.
3.2.3 Physiologic saline[36] [37] was injected into Trigger Points caused by sprains of the knee, ankle, wrist and metacarpophalangeal joint of the thumb. The referred pain caused by these trigger points was at first elicited and then permanently relieved by the saline injection.
3.2.4 Leriche[38] injected 5 or 6 ligamentous TP sites with a local anesthetic following a sprain or fracture with complete pain relief.
3.2.5 Gorrell[39] outlined a technique for the identification and injection of ligamentous ankle TPs after reviewing the anatomy of the ankle ligaments.
3.2.6 Kraus[40] presented a literature review of injection treatment of ligamentous TPs indicating the ease of point location, the immediacy of pain relief and the subsequent 10-day post injection soreness.
3.2.7 Hacket[41] outlined pain patterns of iliolumbar, sacroiliac, sacrospinal, and sacrotuberous ligaments.
3.2.8 Dittrich[42] studied the latissimus dorsi aponeurosis and found Trigger Points in the aponeurosis at the junction of the lumbodorsal fascia which referred pain to the shoulder region.
3.2.9 Weiser[43] relieved medial knee pain symptoms by injecting 2% lidocaine (Xylocaine) with triamcinolone into the tender spot at the insertion of the semimembranosus muscle in 98 patients.
3.2.10 De Valera and Raftery[44] injected a local anesthetic into three pelvic ligaments, the sacroiliac, sacrospinous and sacrotuberous, abolishing referred painful symptoms.
3.3 Periosteal Trigger Points
3.3.1 Kellgren[45] injected hypertonic saline into the periosteum producing painful referred symptoms.
3.3.2 Saunders [46] reported on 160 experiments designed to describe the nature of pain referred from deep tissue structures such as the periosteum. Noxious stimulation included; scratching it with a needle, injecting it with 6% salt solution, or by applying a measured pressure. All of these stimulations produced severe referred painful symptoms which ranged in intensity and distance of projection based on strength of stimulus. When these periosteal or ligamentous attachments were repeatedly stimulated a consistent pattern of referred pain emerged. Autonomic reactions, such as sweating, blanching, and nausea were subjectively reported by research subjects.
3.3.3 Gross[47] reinforced the observation that the deep periosteal structures refer pain,
3.3.4 Lawrence[48] injected a local anesthetic into periosteal TPs, which relieved painful symptoms.
3.4 Vasoconstriction due to over stimulation of sympathetic nerve fibers.
3.4.1 Gutstein-Good wrote at least 12 papers between 1938[49] and 1957[50] repeatedly asserting that TPs were a result of vasoconstriction due to an over stimulation of the sympathetic fibers supplying the vessels.
3.4.2 Travell & Simons[51] “Increased Metabolism/Reduced Circulation -Sympathetic mediated vasoconstriction is the most likely central feedback mechanism to maintain restricted circulation. The fact that stimulation of muscle nociceptors strongly activates y-motor efferents to the muscle spindles may contribute indirectly.
3.4.3 Travell & Simons[52] explain how acute overload or repetitive stress may damage the muscle cells sarcoplasmic reticulum resulting in release of its stored calcium and sustained contracture. The body could respond with severe local vasoconstriction. “There is now a region of increased metabolism with decreased circulation and the muscle fibers passing through that region are strongly shortened independent of propagated action potentials. “ This model may not however explain the underlying process of the formation of trigger points in non-muscular tissue such as ligaments and periosteal tissue.
3.4.4 Revis[53] describes the vasoconstriction found in reflex sympathetic dystrophy which may be instructive of a similar process found in myofascial trigger points. “In healthy patients, a sympathetic response to injury occurs, with vasoconstriction designed to prevent blood loss and swelling. This initial response soon subsides and gives way to vasodilatation and increased capillary permeability, allowing tissue repair. In patients with RSD, this sympathetic response continues unabated. The reasons for the perpetuation of the response is not known but may be related to central dysregulation of nociceptive impulses. This dysregulation may be mediated by wide dynamic range neurons in the spinal cord. Prolonged ischemia from the vasoconstriction produces more pain, establishing a reflex arc that promotes further sympathetic discharge and vasospasm.”
3.5 Prevalence of Inflammation/Subluxation as a cause of pain
3.5.1 A Chronic Pain[54] web site sums up a subscriber’s opinion (Mike) (last name withheld) of inflammation and Chronic pain “During medical and other therapy training programs, we are taught that repetitive strain injury causes inflammation of the overused tissues.”….” Most of the time, however, the primary pathology resulting from repetitive strain injury is not inflammation, but rather it is myofascial pain generated primarily from trigger points in the injured muscles.”
3.5.2 Barrett[55] “Many chiropractors have claimed that spinal misalignments cause or contribute to disease by choking off "nerve energy" to body tissues.”…” The conditions often have nothing to do with a patient's symptoms and are not changed by chiropractic treatment.”
3.5.3 The National Association for Chiropractic Medicine (NACM) states in their Web Site[56] “The first and foremost requirement for membership in the NACM is that a Doctor of Chiropractic Medicine renounce the chiropractic hypothesis and/or philosophy; that is, the tenets upon which their scope of practice is based.”….” The original chiropractic hypothesis, stated simply, is that "Subluxation is the cause of disease."”…” Because the hypothesis has found no validity in universally accepted, peer-reviewed, published scientific journals, belief in the hypothesis, then, is essentially theosophy. Science has not found any organ system pathology which "adjustment" or "manipulation" of spinal joint structures has effect; that is, no disease or "dis-ease" process is affected.”
3.6 Prevalence, Severity and Cost
3.6.1 Sola et al.[57] Among 200 unselected, asymptomatic young adults. Focal tenderness representing latent TPs in 54% of the female, and 45% of the male subjects. Referred pain was demonstrated in 5% of these subjects.
3.6.2 Travell & Simons[58] state that pain from TPs can match the severity of a heart attack. “The severity of symptoms ranges from painless restriction, to agonizing incapacitating pain”
3.7 Implications of Research
3.7.1
4 Research Questions and Hypothetical Discussion
4.1 Research Questions
4.1.1 Do chemical irritants cause referred pain?
4.1.2 Do chemical irritants refer in patterns similar to the referral patterns of ligament and tendon irritation?
4.1.3 Does the sympathetic nervous system cause vasoconstriction subsequent to novel, repetitive, or over activity?
4.1.4 Do the waste products of cell metabolism cause referred pain?
4.1.5 Do inflammatory chemicals irritate afferent nerve fibers?
4.1.6 Do patients symptoms reduce significantly more when treatment is applied to clinically active areas than when massage treatment is applied gernerally?
4.2 Proposed Medical Research Hypothesis, Design and Methodology
4.2.1 Chemical Irritants injected into the end attachments of ligaments and tendons cause referred phenomena in predictable and observable patterns with attendant dysfunction, which is abolished by anesthetic injection.
4.2.1.1 Research Design and Methodology
4.2.1.1.1 Hypertonic saline solution (0.1-0.3 ml of 6%) injected into ligament and tendon attachments near where they attach to the bone. Muscle testing, Trigger Point examination, Postural examination and Grid Data recording sheets are used to determine the path and nature of referral phenomena. These paths are compared with predictable and observable patterns (dermatomally, sclerotomally, myotomally, and extrasegmentally) and with expected symptoms. (headaches, muscle weakness, trigger points, postural dysfunction, sweating, blanching, and nausea, (sometimes referred Cutaneous Paresthesia and numbness instead of deep pain)). 2% lidocaine (Xylocaine) with triamcinolone or other comparable anesthetic is injected into the treatment area and the above examintion and recording protocols are used and analysis of results provided.
4.2.2 Chemical Irritants injected into the end attachments of ligaments and tendons cause referred phenomena in predictable and observable patterns with attendant dysfunction, which is abolished by massage therapy.
4.2.2.1 Research Design and Methodology
4.2.2.1.1 Hypertonic saline solution (0.1-0.3 ml of 6%) injected into ligament and tendon attachments near where they attach to the bone. Muscle testing, Trigger Point examination, Postural examination and Grid Data recording sheets are used to determine the path and nature of referral phenomena. These paths are compared with predictable and observable patterns (dermatomally, sclerotomally, myotomally, and extrasegmentally) and with expected symptoms. (headaches, muscle weakness, trigger points, postural dysfunction, sweating, blanching, and nausea, (sometimes referred Cutaneous Paresthesia and numbness instead of deep pain)). Massage therapy (Ischemic compression or similar technique) is applied to the treatment area. The above examination and recording protocols are used and analysis of results provided.
4.2.3 The sympathetic nervous system causes vasoconstriction of the vessels surrounding the clinically affected area subsequent to novel, overly repetitive, or over activity
4.2.3.1 Research Design and Methodology
4.2.3.1.1 Subjects perform exercises (novel, repetitive and or overly intense activity), which stress ligaments and or tendons of a predefined clinical area. The rate at which radioactive NaI is eliminated from tissue in the clinically affected area is measured. Prolongation of the resorption rate of the isotope, which is due to impaired local circulation will be noted.
4.2.4 Prolonged exercise (novel, overly repetitive, or over activity) results in the production of inflammatory chemicals and vasodilation of the clinically affected areas. These irritated tissues refer in predictable and observable patterns.
4.2.4.1 Research Design and Methodology
4.2.4.1.1 Sedentary Subjects are given prolonged exercise and skin conductance studies are performed on clinically affected areas. Notation is made regarding conductance rates and is compared to surrounding areas. Pain and or sensation referral patterns are also recorded.
4.3 Proposed Patient Research, Hypothesis, Design and Methodology
4.3.1 Project # 1
4.3.1.1 Hypothesis
4.3.1.1.1 Localization and treatment (Ischemic Compression) of specific sites of vasoconstriction and or vasodilation (Inflammation) will correlate highly with reduced subjective reports of pain.
4.3.1.2 Research Design and Methodology
4.3.1.2.1 Randomised post exertion pain patient selection, clinical assessment completed to determine discrete areas of vasoconstriction (Ischemia) and or inflammation (Vasodilation), Pre treatment pain rating obtained from patients and statistically compared with post treatment pain rating for treatment effects.
4.3.2 Project # 2
4.3.2.1 Hypothesis
4.3.2.1.1 Localization and treatment (Ischemic Compression) of specific sites of vasoconstriction and or vasodilation (Inflammation) is more effective than circulatory massage to the general area.
4.3.2.2 Research Design and Methodology
4.3.2.2.1 Two groups of randomised post exertion pain patient are selected, clinical assessment completed to determine discrete areas of vasoconstriction (Ischemia) and or inflammation (Vasodilation), Pre treatment pain rating obtained from patients in both groups and statistically compared with post treatment pain rating for treatment effects. The statistical outcomes of both groups are then compared and the results noted.
5 Single Case (Anecdotal) Studies
5.1 Introduction
5.1.1
5.2 Rating Scales
5.2.1 Sensation Intensity
5.2.1.1 No Sensation 0
5.2.1.2 Mild Sensation 1-3
5.2.1.3 Discomforting 3-5
5.2.1.4 Distressing 5-7
5.2.1.5 Horrible 7-9
5.2.1.6 Excruciating 9-10
5.3 Single Case Single Visit (Anecdotal) Studies
5.3.1 Plantar Foot
5.3.1.1 Cell Stress/Death of Superficial & Intrinsic Foot Structures at Calcaneal & Metatarsal Attachments
5.3.1.1.1 Study Title
5.3.1.1.1.1 “Single Case Single Visit Outcome (Anecdotal) Study-Plantar Foot-Superficial & Intrinsic Foot Structure Attachments -The Treatment Effects of Compression and Stretching.”
5.3.1.1.2 Summary of Protocol (Detailed Protocol)
5.3.1.1.2.1 Patient Selection
5.3.1.1.2.1.1 Pre-screening
5.3.1.1.2.1.1.1 EXCLUDE
5.3.1.1.2.1.1.1.1 Lumbar Pathology, Lumbar Pain, Early AM Heal Pain, Achilles Tendonitis and Sedentary (40-60 yr old) recently active women
5.3.1.1.2.1.1.2 CAN INCLUDE
5.3.1.1.2.1.1.2.1 Frequent Weight Bearing Activities, Wear Shoes w/ Elevated Heals, and Plantar Foot Tenderness(Right Foot) (Palpation Plantar Foot)
5.3.1.1.2.1.1.3 MUST INCLUDE
5.3.1.1.2.1.1.3.1 Achilles Tendon Tenderness (Right Foot) (Palpation Achilles Tendon)
5.3.1.1.2.2 Treatment Technique and Sensation Intensity Rating
5.3.1.1.2.2.1 Pre-Treatment Rating (0-10) (Sensation Intensity Rating Scale) using 3 lbs pincer (pinching) pressure along Achilles Tendon (Right & Left Foot) (Palpation Achilles Tendon)
5.3.1.1.2.2.2 Compression and Stretching Treatment at (Right Foot) Calcaneal Tuberosity (Medial & Lateral Process), bases of the 2nd-5th metatarsals, and between the Proximal Heads of the Metatarsal bones (Technique Plantar Foot) (Alternate Technique)
5.3.1.1.2.2.3 Post-Treatment Rating (0-10) (Sensation Intensity Rating Scale) using 3 lbs pincer (pinching) pressure along Achilles Tendon (Right Foot) (Palpation Achilles Tendon)
5.3.1.1.3 Illustrations
5.3.1.1.3.1 Why Do We Hurt?
5.3.1.1.3.2 Dermatomes ALL
5.3.1.1.3.3 Dermatomes L1-S3 Front
5.3.1.1.3.4 Dermatomes L1-S4 Back
5.3.1.1.3.5 Extrasegmental Referral
5.3.1.1.3.6 Cell Stress/Death of Intrinsic Foot Structures-Direction of Pressure
5.3.1.1.3.7 Muscle Bone Attachments-Foot Plantar Right
5.3.1.1.3.8 Bones Foot Plantar Surface
5.3.1.1.3.9 Plantar Aponeurosis (Fascia) Illustrated
5.3.1.1.3.10 Plantar Aponeurosis (Fascia) Picture
5.3.1.1.3.11 Technique Plantar Foot
5.3.1.1.3.12 Palpation Achilles Tendon
5.3.1.1.3.13 Palpation Plantar Foot
5.3.1.1.3.14 Palpation L4 Dermatome
5.3.1.1.3.15 Foot Plantar Intrinsic Superficial & Deep View
5.3.1.1.3.16 Tendon, Ligament, Muscle Tissue and Cells
5.3.1.1.3.17 Exit of Spinal Nerves
5.3.1.1.3.18 Cutaneous Nerve Distribution Plantar Foot & Posterior Lower Leg
5.3.1.1.3.19 Right Foot Dorsal/Plantar
5.3.1.1.3.20 Left Talus
5.3.1.1.3.21 Calcaneus
5.3.1.1.3.22 Navicular and Cuboid Bones
5.3.1.1.3.23 1st, 2nd, and 3rd Cuneiform Bones
5.3.1.1.3.24 Metatarsals
5.3.1.1.3.25 Right Foot Lateral & Medial Ligaments
5.3.1.1.3.26 Plantar Ligaments & Joints
5.3.1.1.3.27 Right Foot Synovial Joint Cavities
5.3.1.1.3.28 Lumbar and Sacral Plexus
5.3.1.1.3.29 Nerve Distribution (Lumbar and Sacral Plexus)
5.3.1.1.3.30 Arteries Of Pelvis & Right Lower Extremity Anterior/Posterior
5.3.1.1.3.31 Veins Of Pelvis & Right Lower Extremity Anterior/Posterior
5.3.1.1.3.32 Synovial (Mucous) Sheaths of the Tendons & Retinaculum (Ligaments) Around the Ankle (Lateral & Medial)
5.3.1.1.3.33 Synovial Joint Types
5.3.1.1.3.34 Generalized Synovial Joint Capsule Frontal Section
5.3.1.1.3.35 Bony Anatomy of the Foot and Ankle (Medial & Lateral Aspect)
5.3.1.1.3.36 Tarsal Tunnel Soft Tissue, Achilles Tendon & Calcaneal Bursa
5.3.1.1.3.37 Planes of Reference
5.3.1.1.3.38 Classes of Levers
5.3.1.1.3.39 Phases of Gait
5.3.1.1.4 Observation
5.3.1.1.4.1 I noticed that my clients who did a lot of weight bearing exercise had a lot of tenderness in their achilles tendon, which would diminish with treatment to the plantar aponeurosis and ligament attachments. Further, I noticed the same population tended to develop increased pathology in the plantar foot structures (plantar aponeurosis, long and short plantar ligament ect) I wondered if early treatment could help prevent later pathological developments. After considerable reading of the literature I wondered if at the early stages at least either trigger points or perhaps some metabolic dysfunction was the cause and if so increasing circulation thru massage should help. So I decided to do an anecdotal study. One treatment of pressure (thumb, finger, knuckle=Significant amount of pressure=3-4 lbs or more) to four locations with foot movement as indicated to each client. Treatment
5.3.1.1.5 Rationale for Single Case Studies
5.3.1.1.5.1 The massage therapy profession does not have a boatload, bundle or even a small packet of money for research relative to the pharmaceutical industry for example. Single case single visit out come studies are cheap and easy to do, don’t take a lot of time (15-20 Minutes) and although unscientific by definition (Anecdotal) provide an abundance of useful data which may direct more controlled scientific study. This is like the fashion model photographers’ Polaroid (To check lighting & photogenics before more expensive film is used) or the legal equivalent to prima facie inquiry when the rules of law are loosened to allow legally prohibitive facts in as evidence to assess criminality. Single case outcome studies don’t prove or disprove anything but protocols and statistical methods can be tested and may later serve as useful tools in subsequent more controlled scientific research. This project will further increase the body of knowledge necessary to establish a scientific basis for massage therapy treatments and act as a counterweight to the notion that massage treatment is palliative without curative value.
5.3.1.1.6 Rational for the Theoretical Perspective and Study of Tendon and Ligament Trigger Points
5.3.1.1.6.1 Travell[59] offers a theoretical perspective as to why muscle tissue and its associated deep fascia (FASH-ē-a; fascia=bandage) (Dense (Collagenous) Connective Tissue-Irregularly Arranged around muscles) develops a hyperirritable focal point (Trigger Point) within a taut band of skeletal muscle fibers. This theory, explains why Myofascial Trigger Points may develop in muscle tissue, but it does not explain how trigger points could develop in its associated fascia. Nor does her trigger point manual discuss the location or pain referral patterns of deep Fascial (surrounding muscles) trigger points. Although existence of tendon and ligament trigger points are acknowledged by Travell their location and pain referral patterns are only discussed in relation to the research of others and their location and pain referral patterns are never discussed in detail. The purpose of the following theoretical perspective and subsequent study is to explain the nature of tendon and ligament trigger points and examine the efficacy of clinical massage therapy as a viable curative treatment.
5.3.1.1.7 Theoretical Thinking (See Theoretical Model Why Do We Hurt?)
5.3.1.1.7.1 The facial, Ligamentous, and tendon structures of the foot undergo enormous weight bearing forces especially for individuals who are on their feet a lot, engage in sports activities such as walking, running or hiking, or wear elevated heals. The forces of weight bearing also place pressure on the vessels that supply blood to the tissues. The transport of essential cell nutrition (O2, glucose and protein) to the tendon and connective tissue cells may be diminished and or interrupted. Cell stress and or death may ensue along with concomitant nerve irritation and referred sensory phenomena. With cell stress, enzymatic messengers may initiate a reflex arc (afferent and efferent sympathetic nerve fibres) causing vasoconstriction, increased metabolite concentration, and further nerve irritation. With cell death enzymatic messengers may initiate the production of inflammatory nerve irritants which refer sensory phenomena segmentally (Dermatomes ALL, Dermatomes L1-S3 Front, Dermatomes L1-S4 Back) and extra-segmentally (Extrasegmental Referral). The tendon and connective tissue cells near the bone or at biomechanical stress points may be most affected due greater mechanical stresses and diminished blood supply. (Hume’s Fork, Cell Stress/Death of Intrinsic Foot Structures-Direction of Pressure, Muscle Bone Attachments-Foot Plantar Right, Bones Foot Plantar Surface, Plantar Aponeurosis (Fascia) Illustrated, Plantar Aponeurosis (Fascia) Picture) These Pre-Acute, Acute, and or Chronic conditions if left untreated may have a cascading effect which contribute to clinical conditions e.g.; postural faults Trigger Points and or Plantar Fasciitis. It is unlikely that the usual laboratory measures eg sed rates (erythrocyte sedimentation rate [ESR]), radiography, MRI, and or neurological testing will reveal these sub clinical phenomena. It is expected that a high percentage of active patient populations without lumbar or other pathology will present with these conditions and thus provide a fertile field of study. Ischemic compression and stretching have proven effective in the treatment of trigger points and may help re-establish circulation, help remove metabolic and or inflammatory irritants and improve the transport of essential cell nutrition (O2, glucose and protein) to the tendon and connective tissue cells aforementioned. (Research Summary) This may have a curative effect and help prevent potential clinical pathology (Plantar Fasciitis, postural faults, and or trigger points), athletic injuries, impaired activities of daily living (ADL), and or impaired athletic performance.
5.3.1.1.8 Hypothesis
5.3.1.1.8.1 Hypothesis Defined
5.3.1.1.8.1.1 If a theory is the analysis of a set of speculative facts in their relation to one another with the hope of answering the WHY questions a hypothesis is concise statement in order to draw out and test the theories logical or empirical consequences. In this plantar foot study if the theory states that connective tissue cell stress/death produces neurological irritation and increasing circulation reduces that irritation and provides lasting curative relief then the referred Achilles tendon tenderness should decrease with treatments that increase circulation to these connective tissue structures. Further once circulation is re-established a lasting curative effect in the form of reduced Achilles tendon tenderness should persist without treatment.
5.3.1.1.8.2 Plantar Foot Study Hypothesis-Single Visit
5.3.1.1.8.2.1 Compression and stretching of the connective tissue structures of the plantar foot will significantly reduce Achilles tendon tenderness as subjectively reported by clients.
5.3.1.1.8.3 Plantar Foot Study Hypothesis-Multiple Visit
5.3.1.1.8.3.1 Subsequent treatment (Compression and stretching of plantar foot connective tissues) visits will continue to reduce Achilles tendon tenderness as subjectively reported by clients. This reduced Achilles tendon tenderness will persist even after treatment is discontinued.
5.3.1.1.9 Protocol Detailed (Summary)
5.3.1.1.9.1 Patient Selection
5.3.1.1.9.1.1 Pre-screening
5.3.1.1.9.1.1.1 EXCLUDE the following clients from the study
5.3.1.1.9.1.1.1.1 Persons with known lumbar pathology and or lumbar pain.
5.3.1.1.9.1.1.1.2 These conditions can refer sensory phenomena including pain into the foot along the L4-5 and S1-2 dermatomes (Dermatomes ALL) and will not respond to treatment of the superficial & intrinsic structures. It would then be impossible to judge the effects of treatment as referred pain from the lumbar region would persist.
5.3.1.1.9.1.1.1.3 Persons with Early AM Heal Pain
5.3.1.1.9.1.1.1.4 This is a symptom marker for Plantar Fasciitis, which is a clinical condition that underlies pathology that is more serious. Although this condition may respond to the compression and stretching treatments the focus of the current study is on the treatment effects on sub clinical conditions.
5.3.1.1.9.1.1.1.5 Persons with Achilles Tendonitis
5.3.1.1.9.1.1.1.6 Persons who have a current or past Diagnosis of Achilles Tendonitis will not respond to this treatment. You can suspect Achilles Tendonitis in persons who are overweight and flatfooted or who are long distance runners. These persons should also be excluded from this study.
5.3.1.1.9.1.1.1.7 Sedentary (40-60 yr old) women recently engaged in novel, repetitive or over activity involving walking, standing and or running.
5.3.1.1.9.1.1.1.8 According to Travell[60] sedentary, middle-aged women (40-60 years old) who have recently engaged in novel, repetitive or over activity (walking, standing, and or running) are prone to develop trigger points. Activities such as walking, standing and or running may cause injury to the muscle cells of the Soleus and Tibialis posterior, which can refer pain and tenderness into the Achilles tendon. Since Active patients can still develop trigger points in these lower leg muscles subsequent studies may help determine their numbers. Trigger Point Study
5.3.1.1.9.1.1.2 CAN INCLUDE the following clients in the study
5.3.1.1.9.1.1.2.1 Persons who engage in Frequent Weight Bearing Activities
5.3.1.1.9.1.1.2.2 These clients are more likely to place greater stress on the tissues in question and manifest sub clinical symptoms. Sedentary clients who have symptoms especially those clients who are overweight may have other conditions such as diabetes, deep vein thrombosis ect which will not respond to treatment.
5.3.1.1.9.1.1.2.3 Persons who Wear Shoes w/ Elevated Heals
5.3.1.1.9.1.1.2.4 Greater stresses are placed on the plantar foot structures when clients wear high-healed shoes.
5.3.1.1.9.1.1.2.5 Persons who have Plantar Foot Tenderness (Right Foot) (Palpation Plantar Foot)
5.3.1.1.9.1.1.2.6 This area may be palpated to establish connective tissue irritation near the Proximal Heads of the Metatarsal bones, which refers extrasegmentally and dermatomally into the plantar surface of the foot.
5.3.1.1.9.1.1.3 MUST INCLUDE the following clients in the study
5.3.1.1.9.1.1.3.1 Persons who have Achilles Tendon Tenderness (Right Foot) (Palpation Achilles Tendon)
5.3.1.1.9.1.1.3.2 This area is palpated to determine pre and post treatment ratings. Generally, connective tissue attachments near Calcaneal Tuberosity (Medial Process) refer into the Achilles Tendon, extrasegmentally and dermatomally.
5.3.1.1.9.2 Treatment Technique and Sensation Intensity Rating
5.3.1.1.9.2.1 Pre-Treatment Rating
5.3.1.1.9.2.1.1 3 lbs pincer (pinching) pressure along Achilles Tendon. (Right & Left Foot) (Palpation Achilles Tendon)
5.3.1.1.9.2.1.1.1 The amount of pressure can be roughly gauged by pinching a bathroom scale with your thumb and forefinger until you reach 3 lbs pressure. Then pinch the Achilles tendon (Right & Left Foot) of the client and ask them to rate the sensation using the Sensation Intensity Rating Scale. (0-10) Be sure to label the left and right foot ratings. For example L=4 R=5.
5.3.1.1.9.2.1.1.2 Sensation rating of above 1 will be selected for the study and those persons with ratings below 1 will be excluded from the study.
5.3.1.1.9.2.2 Compression and Stretching Treatment (Technique Plantar Foot)
5.3.1.1.9.2.2.1 Standard Technique (Right Foot ONLY)
5.3.1.1.9.2.2.1.1 Pressure is directed against the Calcaneal Tuberosity and just anterior (Medial & Lateral Process), calcaneal plantar surface, bases of the 2nd-5th metatarsals (Right Foot), with foot Dorsiflexion, and between the Proximal Heads of the Metatarsal bones, with toe extension. Treatment continues until Achilles Tendon tenderness subsides. (Technique Plantar Foot)
5.3.1.1.9.2.2.2 Alternate Technique Hand Position
5.3.1.1.9.2.2.2.1 The technique demonstrated in the picture (Technique Plantar Foot) can be altered to suit individual therapist preferences. For example separated fingers can be used against the bony processes with foot dorsiflexion while the client is in the supine position. If the client is prone using the same or more comfortable finger position the foot is dorsiflexed while the leg is flexed at the knee.
5.3.1.1.9.2.3 Post-Treatment Rating
5.3.1.1.9.2.3.1 3 lbs pincer (pinching) pressure along Achilles Tendon. (Right Foot) (Palpation Achilles Tendon)
5.3.1.1.9.2.3.1.1 The amount of pressure can be roughly gauged by pinching a bathroom scale with your thumb and forefinger until you reach 3 lbs pressure. Then pinch the Achilles tendon (Right Foot) of the client and ask them to rate the sensation using the Sensation Intensity Rating Scale. (0-10)
5.3.1.2 Plantar Foot Study Conducted June/July 2002
5.3.1.2.1 Study Title
5.3.1.2.1.1 “Single Case Single Visit Outcome (Anecdotal) Study-Plantar Foot-Superficial & Intrinsic Foot Structure Attachments -The Treatment Effects of Compression and Stretching. June/July 2002”
5.3.1.2.2 Summary of Protocol (Detailed Protocol)
5.3.1.2.2.1 Summary of Protocol
5.3.1.2.3 Rationale
5.3.1.2.3.1 Rationale
5.3.1.2.4 Theoretical Thinking
5.3.1.2.4.1 Theoretical Thinking
5.3.1.2.5 Protocol Detailed (Summary)
5.3.1.2.5.1 Protocol Detailed
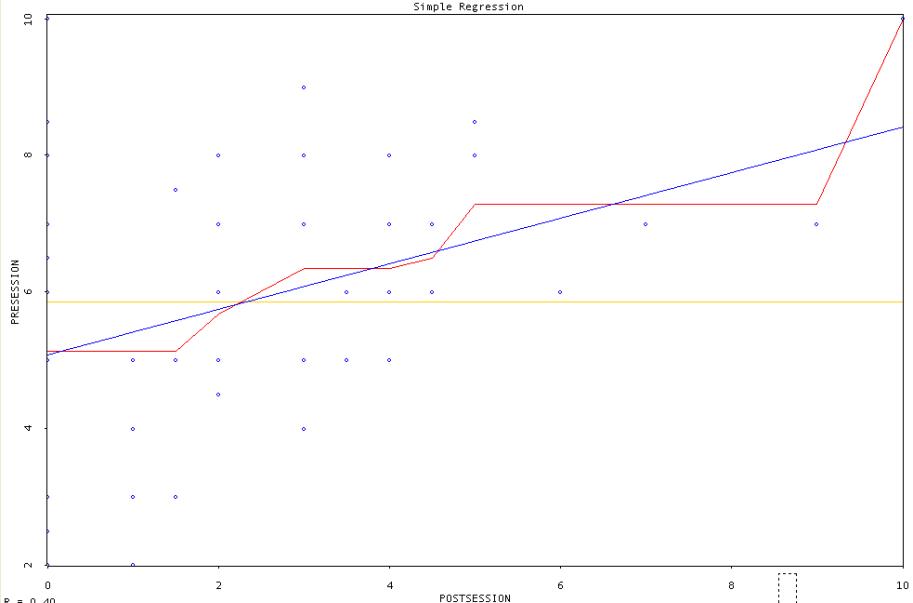
5.3.1.2.6 Analysis of Study
5.3.1.2.6.1 The t Score of 12.01912473, which assesses whether the means of two groups are statistically different from one another is more than the expected critical value at alpha .001= 3.46455. The average reduction in tenderness of the tendon was 62%. This strongly suggests that the treatment alone and or some other factor such as placebo or gate effect is responsible for the decrease in the Achilles’ tendon palpation tenderness. In either case the difference between pre and posttest means was significant and the null hypothesis can be rejected. The correlation coefficient (r (Pearson product-moment correlation coefficient)) between pre and posttest scores was 0.395997391. This allows us to correctly predict scores along a regression line 16% (Coefficient of Determination (COD)) of the time, which is significantly better than guessing (9%). If this were a better-designed study (randomized groups, control groups ect) over a large population of clients, this would be a significant result. Since this is not the case, the treatment effectiveness cannot be confirmed. Perhaps the statistical measure for such a small study is faulty. If you would like to volunteer your statistical expertise, click this link. Web Site Help Since this study was done by a single practitioner it will be interesting to see what results a multiple practitioner single case study will produce. In this study, (June/July 2002) since clients were expecting some type of treatment for their Achilles’ tendon tenderness that expectation (placebo effect) alone may be responsible for some or all of the treatment effect. If research progresses this factor should be considered in the Research Design and Methodology (RDM). In addition, since the treatment may be mildly or moderately discomforting to the client the strength of that signal may initiate a neurological gate (gate effect), which blocks any sensitivity from the Achilles’ tendon. The Gate effect alone may be responsible for some or all of the treatment effect. The Gate effect should be factored out as a treatment effect in future Research Design and Methodology. Still with such a strong treatment effect we are probably looking at some measure of treatment efficacy. Longitudinal studies where one patient is followed over time should reveal whether patients Achilles’ tendon tenderness subsides after several treatments and then remains less sensitive even without treatment. My own anecdotal patient notes demonstrate this finding.
5.3.1.2.7 Excel Worksheet for Plantar Study
5.3.1.2.7.1 Plantar Study
5.3.1.2.8 Discussion of Statistics
5.3.1.2.8.1 Statistics Discussion
5.3.1.2.9 Visualization of Research Data
5.3.1.2.9.1 Box Diamond & Dot Plot
5.3.1.2.9.2 Pre Session Rating Frequency Distribution
5.3.1.2.9.3 Post Session Rating Frequency Distribution
5.3.1.2.9.4 Theoretical Sampling Distribution Of The Mean Pre Session
5.3.1.2.9.5 Theoretical Sampling Distribution Of The Mean Post session
5.3.1.2.9.6 Sampling Distribution Of Differences Between Means
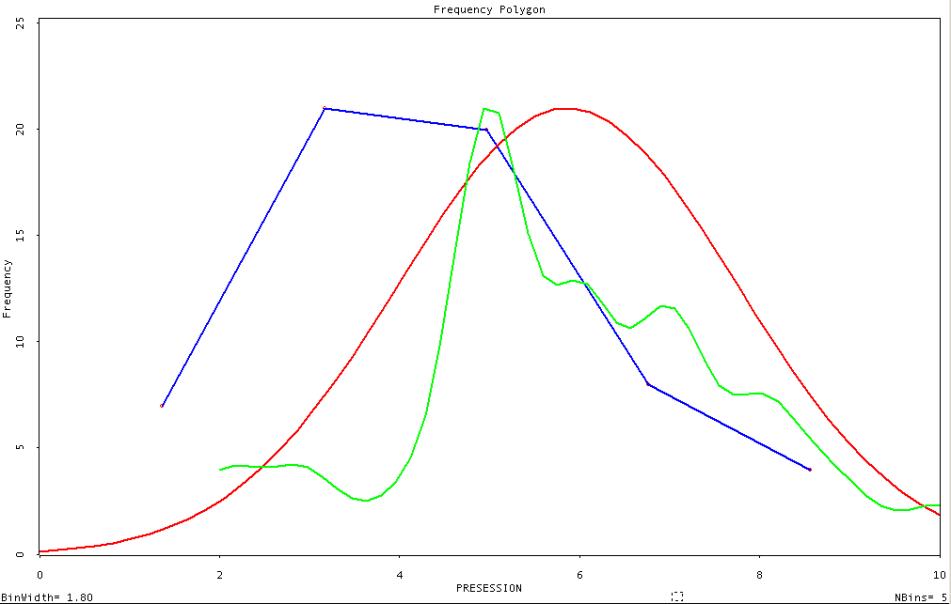
5.3.1.2.9.7 Frequency Polygon Pre-Session
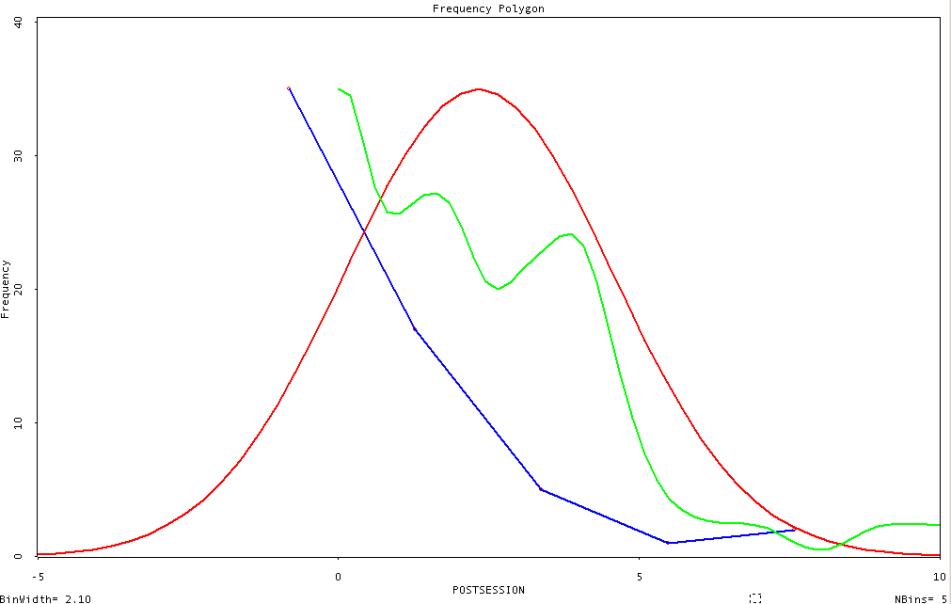
5.3.1.2.9.8 Frequency Polygon Post-Session
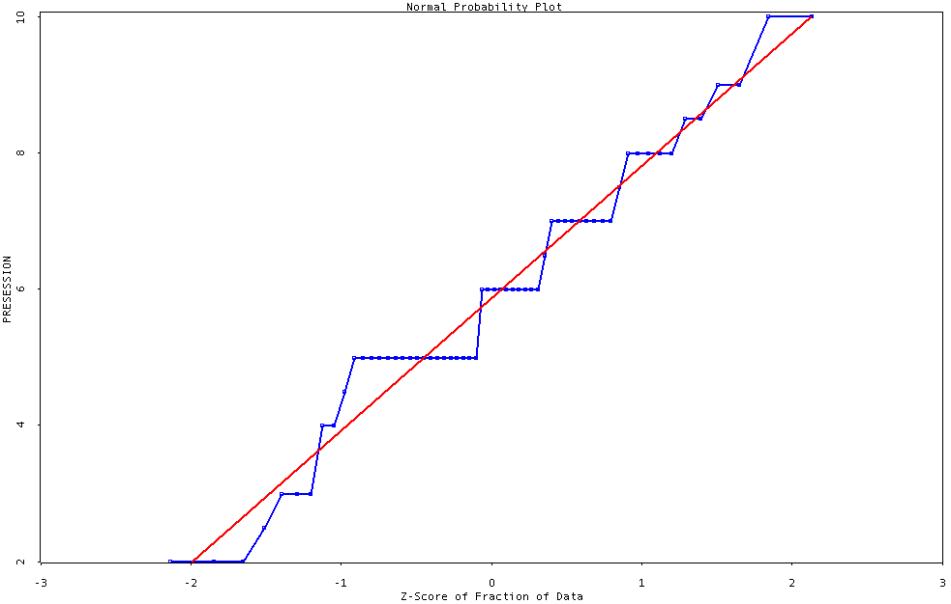
5.3.1.2.9.9 Normal Probability Plot
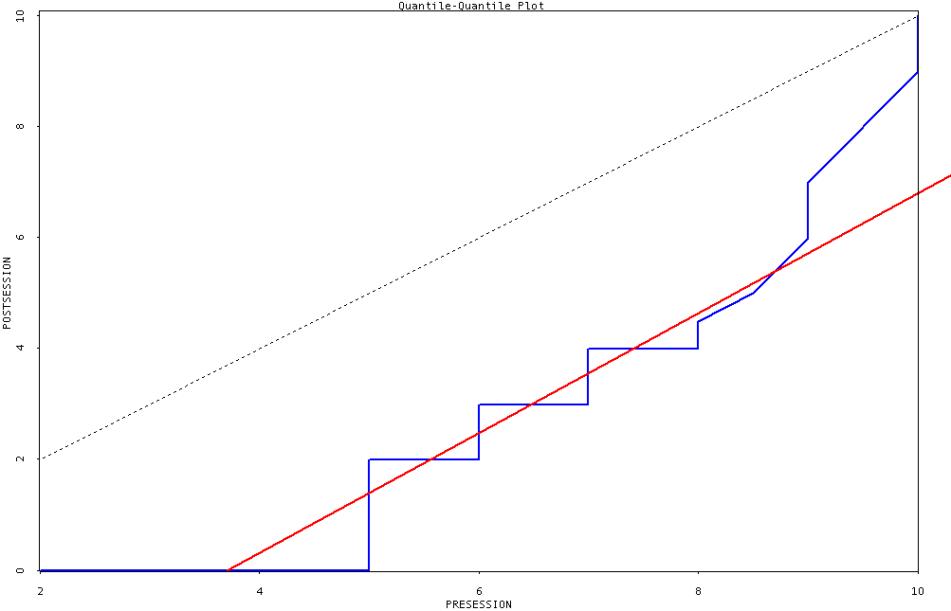
5.3.1.2.9.10 Quantile-Quantile Plot
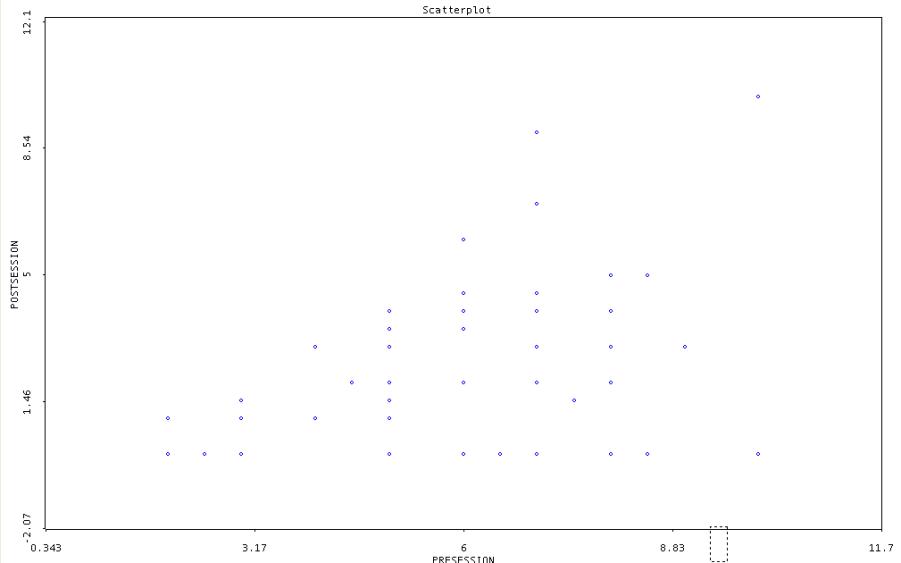
5.3.1.2.9.11 Scatter Plot
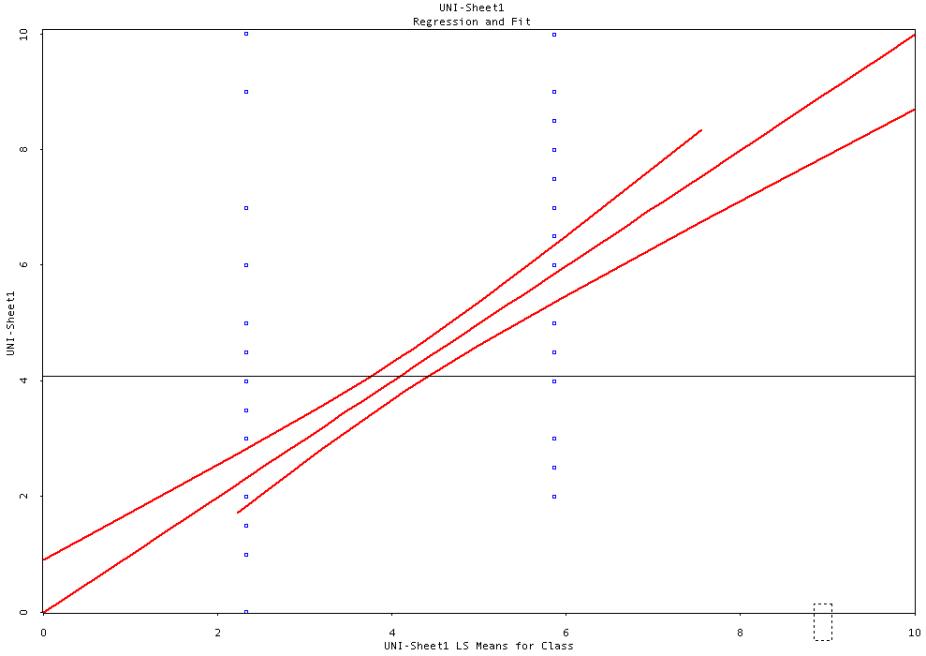
5.3.1.2.9.12 Simple Regression
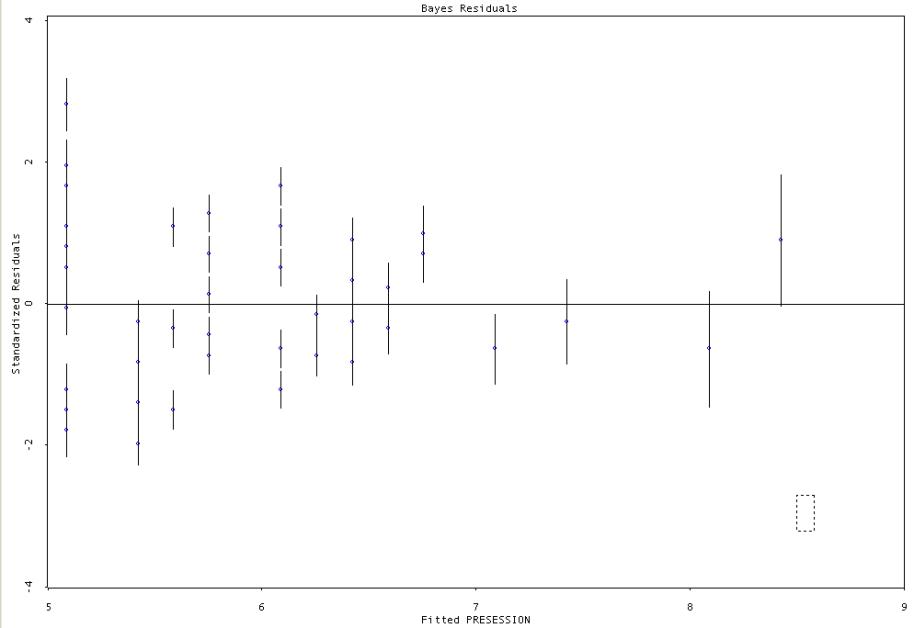
5.3.1.2.9.13 Bayes Residuals
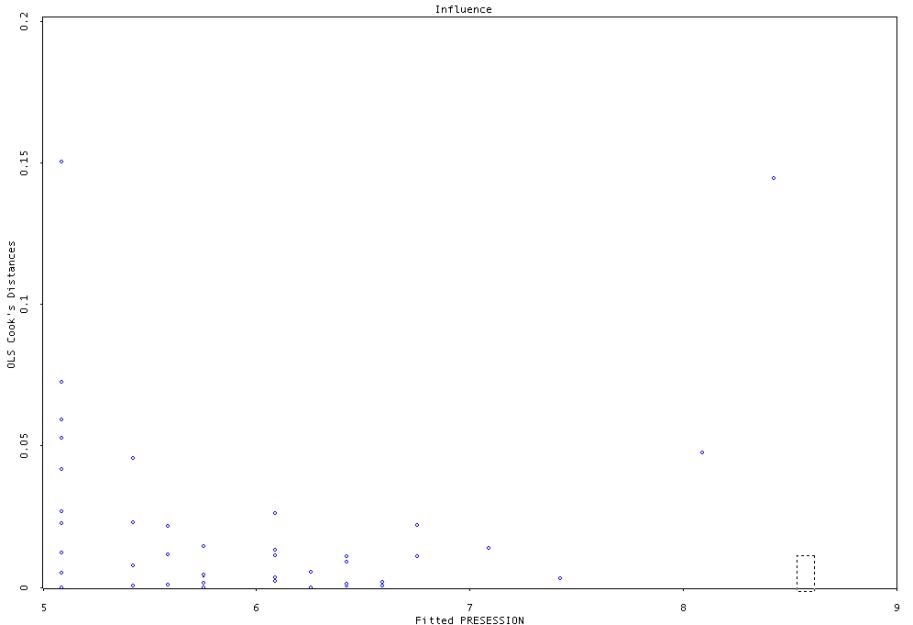
5.3.1.2.9.14 Influence Plot
5.3.1.2.9.15
ANOVA
(partial) regression plot
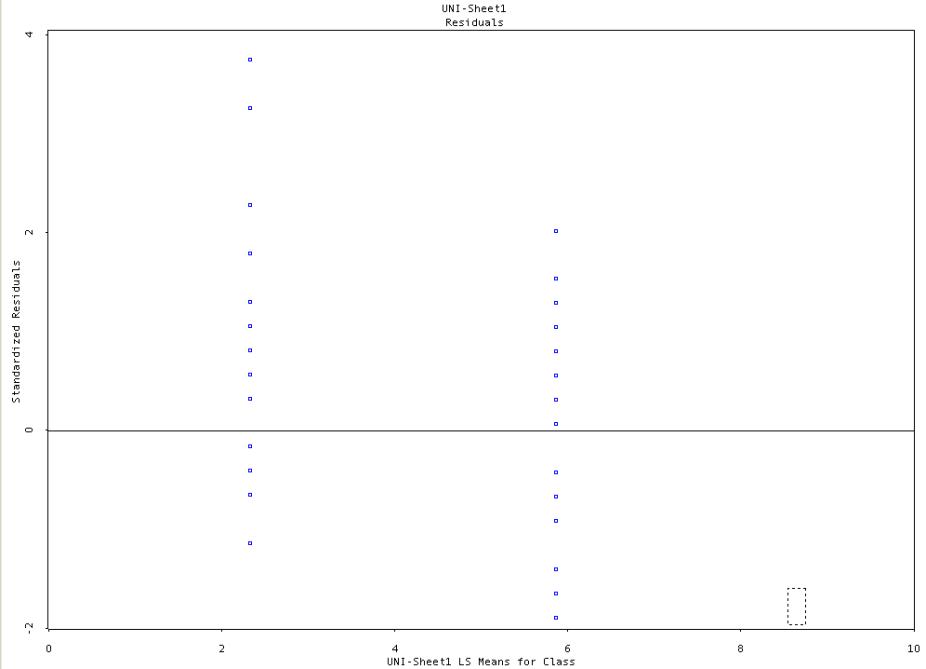
5.3.1.2.9.16 Residuals Plot-Univariate Analysis
5.3.2 Soleus and Tibialis Posterior Trigger Points
5.3.2.1 Study Title
5.3.2.1.1 “Single Case Single Visit Outcome (Anecdotal) Study-Soleus and Tibialis Posterior Trigger Points -The Treatment Effects of Ischemic Compression and Stretching.”
5.3.2.2 Information on Trigger Points
5.3.2.2.1 Defined
5.3.2.2.2 Clinical Criteria
5.3.2.2.3 Theoretical Model-What Causes Trigger Points
5.3.2.2.4 Literature Review
5.3.2.2.5 Flat Palpation
5.3.2.2.6 Pincer Palpation
5.3.2.2.7 Snapping Palpation
5.3.2.2.8 Ischemic Compression
5.3.2.3 Summary of Protocol Trigger Point (Detailed)
5.3.2.3.1 Patient Selection
5.3.2.3.1.1 Pre-screening
5.3.2.3.1.1.1 EXCLUDE
5.3.2.3.1.1.1.1 Lumbar Pathology, Lumbar Pain, Early AM Heal Pain, Achilles Tendonitis, and Sedentary (40-60 yr old) recently active women
5.3.2.3.1.1.2 CAN INCLUDE
5.3.2.3.1.1.2.1 Frequent Weight Bearing Activities, Wear Shoes w/ Elevated Heals, and Plantar Foot Tenderness (Palpation Plantar Foot) (Right Foot)
5.3.2.3.1.1.3 MUST INCLUDE
5.3.2.3.1.1.3.1 Achilles Tendon Tenderness (Right Foot) (Palpation Achilles Tendon)
5.3.2.3.1.1.3.2 Persons who have Exquisite, focal tenderness in Trigger Points (TP1) (Right Foot) of either the Soleus (Soleus) (Soleus Trigger Points) and or the Tibialis Posterior (Tibialis Posterior) (Tibialis Posterior Trigger Points)
5.3.2.3.1.2 Treatment Technique and Sensation Intensity Rating
5.3.2.3.1.2.1 Pre-Treatment Rating (0-10) (Sensation Intensity Rating Scale) using 3 lbs pincer (pinching) pressure along Achilles Tendon (Right Foot) (Palpation Achilles Tendon)
5.3.2.3.1.2.2 Flat & Pincer palpation Assessment, Ischemic Compression and Stretching Treatment Soleus and Tibialis Posterior (TP1) (Right Foot)
5.3.2.3.1.2.3 Post-Treatment Rating (0-10) (Sensation Intensity Rating Scale) using 3 lbs pincer (pinching) pressure along Achilles Tendon (Right Foot) (Palpation Achilles Tendon)
5.3.2.4 Illustrations
5.3.2.4.1 Neuron-Motor
5.3.2.4.2 Neuron-Sensory
5.3.2.4.3 Exit of Spinal Nerves
5.3.2.4.4 The Structure of Skeletal Muscle
5.3.2.4.5 Connective Tissue Layers
5.3.2.4.6 Motor Units
5.3.2.4.7 Histology of Skeletal Muscle Tissue
5.3.2.4.8 Neuromuscular Junction
5.3.2.4.9 Myofilaments Detailed Structure
5.3.2.4.10 Role of Ionic Calcium in Contraction
5.3.2.4.11 Event Sequence Actin Filament Sliding
5.3.2.4.12 Sequence of events in Excitation-Contraction Coupling
5.3.2.4.13 Skeletal Muscle Energy Metabolism Aerobic Anaerobic
5.3.2.4.14 Foot and Toes Superficial Anterior and Right Lateral View
5.3.2.4.15 Foot and Toes Superficial Posterior View
5.3.2.4.16 Lower Leg Posterior Muscle Bone Attachments
5.3.2.4.17 Right Dorsal Foot Muscle Bone Attachments
5.3.2.4.18 Muscle Bone Attachments-Foot Plantar Right
5.3.2.4.19 Soleus
5.3.2.4.20 Tibialis Posterior
5.3.2.4.21 Soleus Trigger Points
5.3.2.4.22 Tibialis Posterior Trigger Points
5.3.2.5 Rationale for Trigger Point Study
5.3.2.5.1 The Soleus and Tibialis Posterior muscles both refer into the Achilles Tendon and thus may be responsible for some of this tendons tenderness in active clients. According to Travell both sexes and all ages can develop TPs but it is sedentary, middle-aged women who engage in novel, repetitive or over activity that are especially vulnerable. It is expected then that the active patients of the plantar foot studies would have fewer though significant Soleus and Tibialis posterior trigger points. Knowing the % of active patients which were included in the previous plantar foot studies with this condition may be useful. This knowledge may help establish a combination of plantar foot and muscle trigger point therapies to treat both sub-clinical and clinical pathologies such as plantar Fasciitis. Knowing the % of active patients with Soleus and Tibialis Posterior trigger points may also explain the weak treatment response of some patients in the previous plantar foot studies.
5.3.2.6
Theoretical Thinking
5.3.2.6.1 Trigger Point Theory
5.3.2.7 Protocol Trigger Point Detailed (Summary)
5.3.2.7.1.1 Patient Selection
5.3.2.7.1.1.1 Pre-screening
5.3.2.7.1.1.1.1 EXCLUDE the following clients from the study
5.3.2.7.1.1.1.1.1 Persons with known lumbar pathology and or lumbar pain.
5.3.2.7.1.1.1.1.2 These conditions can refer sensory phenomena including pain into the foot along the L4-5 and S1-2 dermatomes (Dermatomes ALL) and will not respond to treatment of the superficial & intrinsic structures. It would then be impossible to judge the effects of treatment as referred pain from the lumbar region would persist.
5.3.2.7.1.1.1.1.3 Persons with Early AM Heal Pain
5.3.2.7.1.1.1.1.4 This is a symptom marker for Plantar Fasciitis, which is a clinical condition that underlies pathology that is more serious. Although this condition may respond to the compression and stretching treatments the focus of the current study is on the treatment effects on sub clinical conditions.
5.3.2.7.1.1.1.1.5 Persons with Achilles Tendonitis
5.3.2.7.1.1.1.1.6 Persons who have a current or past Diagnosis of Achilles Tendonitis will not respond to this treatment. You can suspect Achilles Tendonitis in persons who are overweight and flatfooted or who are long distance runners. These persons should also be excluded from this study.
5.3.2.7.1.1.1.1.7 Sedentary (40-60 yr old) women recently engaged in novel, repetitive or over activity involving walking, standing and or running.
5.3.2.7.1.1.1.1.8 According to Travell [61] sedentary, middle-aged women (40-60 years old) who have recently engaged in novel, repetitive or over activity (walking, standing, and or running) are prone to develop trigger points. Activities such as walking, standing and or running may cause injury to the muscle cells of the Soleus and Tibialis posterior, which can refer pain and tenderness into the Achilles tendon. Since the previous plantar foot studies could include active patients who may also have trigger points by excluding sedentary recently active women we can determine how many of our active patients in the previous study may have Soleus and Tibialis trigger points which could account for weak response to treatment and or suggest combined treatments for increased effectiveness.
5.3.2.7.1.1.1.2 CAN INCLUDE the following clients in the study
5.3.2.7.1.1.1.2.1 Persons who engage in Frequent Weight Bearing Activities
5.3.2.7.1.1.1.2.2 These clients are more likely to place greater stress on the tissues in question and manifest sub clinical symptoms. Sedentary clients who have symptoms especially those clients who are overweight may have other conditions such as diabetes, deep vein thrombosis ect which will not respond to treatment.
5.3.2.7.1.1.1.2.3 Persons who Wear Shoes w/ Elevated Heals
5.3.2.7.1.1.1.2.4 Greater stresses are placed on the plantar foot structures when clients wear high-healed shoes.
5.3.2.7.1.1.1.2.5 Persons who have Plantar Foot Tenderness (Palpation Plantar Foot ) (Right Foot)
5.3.2.7.1.1.1.2.6 This area may be palpated to establish connective tissue irritation near the Proximal Heads of the Metatarsal bones, which refers extrasegmentally and dermatomally into the plantar surface of the foot.
5.3.2.7.1.1.1.3 MUST INCLUDE the following clients in the study
5.3.2.7.1.1.1.3.1 Persons who have Achilles Tendon Tenderness (Right Foot) (Palpation Achilles Tendon)
5.3.2.7.1.1.1.3.2 This area is palpated to determine pre and post treatment ratings.
5.3.2.7.1.1.1.3.3 Persons who have Exquisite, focal tenderness in Trigger Points of either the (TP1) (Right Foot) Soleus (Soleus) (Soleus Trigger Points) and or the Tibialis Posterior (Tibialis Posterior) (Tibialis Posterior Trigger Points)
5.3.2.7.1.1.1.3.4 Since both of these muscles refer into the Achilles tendon, it is necessary to locate these trigger points to provide treatment.
5.3.2.7.1.2 Assessment, Treatment Technique and Sensation Intensity Rating
5.3.2.7.1.2.1 Pre-Treatment Rating
5.3.2.7.1.2.1.1 3 lbs pincer (pinching) pressure along Achilles Tendon. (Right Foot) (Palpation Achilles Tendon)
5.3.2.7.1.2.1.1.1 The amount of pressure can be roughly gauged by pinching a bathroom scale with your thumb and forefinger until you reach 3 lbs pressure. Then pinch the Achilles tendon (Right Foot) of the client and ask them to rate the sensation using the Sensation Intensity Rating Scale. (0-10)
5.3.2.7.1.2.1.1.2 Sensation rating of above 1 will be selected for the study and those persons with ratings below 1 will be excluded from the study.
5.3.2.7.1.2.2 Flat & Pincer palpation Assessment, Ischemic Compression and Stretching Treatment Soleus and Tibialis Posterior (TP1) (Right Foot)
5.3.2.7.1.2.2.1 Establish existence of Exquisite, focal tenderness (Trigger Points in the Soleus and Tibialis Posterior
5.3.2.7.1.2.2.1.1 Soleus
5.3.2.7.1.2.2.1.2 Locate TP1 (Soleus Trigger Points) in the Soleus (Soleus) using flat palpation or pincer palpation
5.3.2.7.1.2.2.1.3 Tibialis Posterior
5.3.2.7.1.2.2.1.4 Locate TP1 (Tibialis Posterior Trigger Points) in the Tibialis Posterior (Tibialis Posterior)
5.3.2.7.1.2.2.1.5 To locate the Tibialis Posterior Trigger Points it is necessary to push the gastrocnemius aside from a lateral or medial direction and apply flat palpation thru the Soleus muscle to the trigger points of the Tibialis posterior
5.3.2.7.1.2.2.2 Ischemic Compression and Stretching Treatment (TP1) (Right Foot)
5.3.2.7.1.2.2.2.1 Ischemic Compression is applied to TP1 of both the Soleus and Tibialis Posterior with foot Dorsiflexion. Treatment continues until Achilles Tendon tenderness subsides.
5.3.2.7.1.2.3 Post-Treatment Rating
5.3.2.7.1.2.3.1 3 lbs pincer (pinching) pressure along Achilles Tendon. (Right Foot) (Palpation Achilles Tendon)
5.3.2.7.1.2.3.1.1 The amount of pressure can be roughly gauged by pinching a bathroom scale with your thumb and forefinger until you reach 3 lbs pressure. Then pinch the Achilles tendon (Right Foot) of the client and ask them to rate the sensation using the Sensation Intensity Rating Scale. (0-10)
5.4 Single Case Multiple Visit (Anecdotal) Studies
5.4.1 Plantar Foot
5.4.1.1 Cell Stress/Death of Superficial & Intrinsic Foot Structures at Calcaneal & Metatarsal Attachments
5.4.1.1.1 Study Title
5.4.1.1.1.1 “Single Case Multiple Visit Outcome (Anecdotal) Study-Plantar Foot-Superficial & Intrinsic Foot Structure Attachments -The Treatment Effects of Compression and Stretching.”
5.4.1.1.2 Summary of Protocol (Detailed Protocol)
5.4.1.1.3 Protocol Detailed (Summary)
5.4.1.1.4 Subsequent Visit Protocol
5.4.1.1.4.1 There are 5 additional visits added to the multiple visit outcome study.
5.4.1.1.4.2 Four of these visits contain the same components as the single visit study e.g. Pre-Rating, Treatment, and Post-Rating.
5.4.1.1.4.3 The time spacing between the first and subsequent visits (2-5) should be between 2 and 3 days with no more than 3 days between treatments.
5.4.1.1.4.4 The last visit (Visit # 6) contains only a final rating of both the (Right & Left Foot) with NO PRE-RATING or TREATMENT component. Be sure to label the left and right foot ratings. For example L=4 R=5.
5.4.1.1.4.5 The time spacing between the fifth and sixth visit should be exactly 7 days.
5.4.1.1.5 Rational for Subsequent Visits
5.4.1.1.5.1 The single case single visit study does not tell us the following.
5.4.1.1.5.1.1 Gate Effect- since the treatment may be mildly or moderately discomforting to the client the strength of that signal may initiate a neurological gate (gate effect) which blocks any sensitivity from the Achilles’ tendon. My own anecdotal patient notes seem to indicate the Gate Effect lasts between 2-3 days.
5.4.1.1.5.1.2 Placebo Effect- Since clients were expecting some type of treatment for their Achilles’ tendon tenderness that expectation (placebo effect) alone may be responsible for some or all of the treatment effect. My own anecdotal patient notes seem to indicate the Placebo Effect lasts between 2-3 days.
5.4.1.1.5.1.3 Curative Effect-Depending on the severity of the pre-acute. Acute or chronic irritation it may take several treatments to re-establish circulation to the affected connective tissue cells. These treatment effects can only be measured with a multiple visit study. In addition, the 7 days between the 5th and 6th visit allows for the diminution of the Gate and Placebo effect so that the more lasting curative effect can be measured.
5.4.2 Soleus and Tibialis Posterior Trigger Points
5.4.2.1.1 Study Title
5.4.2.1.1.1 “Single Case Multiple Visit Outcome (Anecdotal) Study- Soleus and Tibialis Posterior Trigger Points -The Treatment Effects of Ischemic Compression and Stretching.”
5.4.2.1.2 Summary of Protocol (Detailed Protocol)
5.4.2.1.3 Protocol Detailed (Summary)
5.4.2.1.4 Subsequent Visit Protocol Trigger Point Multiple Visit Study
5.4.2.1.4.1 There are 5 additional visits added to the Multiple visit outcome study.
5.4.2.1.4.2 Four of these visits contain the same components as the single visit study e.g. Pre-Rating, Treatment, and Post-Rating.
5.4.2.1.4.3 The time spacing between the first and subsequent visits (2-5) should be between 2 and 3 days with no more than 3 days between treatments.
5.4.2.1.4.4 The last visit (Visit # 6) contains only a final rating with NO PRE-RATING or TREATMENT component.
5.4.2.1.4.5 The time spacing between the fifth and sixth visit should be exactly 7 days.
5.4.2.1.5 Rational for Subsequent Visits Trigger Point Multiple Visit Study
5.4.2.1.5.1 The single case single visit study does not tell us the following.
5.4.2.1.5.1.1 Gate Effect- since the treatment may be mildly or moderately discomforting to the client the strength of that signal may initiate a neurological gate (gate effect) which blocks any sensitivity from the Achilles’ tendon. My own anecdotal patient notes seem to indicate the Gate Effect lasts between 2-3 days.
5.4.2.1.5.1.2 Placebo Effect- Since clients were expecting some type of treatment for their Achilles’ tendon tenderness that expectation (placebo effect) alone may be responsible for some or all of the treatment effect. My own anecdotal patient notes seem to indicate the Placebo Effect lasts between 2-3 days.
5.4.2.1.5.1.3 Curative Effect-Depending on the severity of the pre-acute. Acute or chronic irritation it may take several treatments to re-establish circulation to the affected connective tissue cells. These treatment effects can only be measured with a multiple visit study. In addition, the 7 days between the 5th and 6th visit allows for the diminution of the Gate and Placebo effect so that the more lasting curative effect can be measured.
6 Clinical Assessment and Treatment Modalities
6.1 Introduction
6.1.1
6.2 General Functional Anatomy and Physiology
6.2.1 Introduction
6.2.1.1
6.2.2 Histology (hiss’-TOL-ō-jē; histio=tissue; logos=study of)-
6.2.2.1 Connective Tissue
6.2.2.1.1 Introduction
6.2.2.1.1.1
6.2.2.1.2 Definitions
6.2.2.1.2.1 Fibroblast (FĪ-brō-blast)
6.2.2.1.2.1.1
6.2.2.1.2.2 Collagen (KOL-a-jen)
6.2.2.1.2.2.1
6.2.2.1.3 Connective Tissue Proper
6.2.2.1.3.1 Dense (Collagenous) Connective Tissue
6.2.2.1.3.1.1 Irregularly Arranged
6.2.2.1.3.1.1.1
6.2.2.1.3.1.2 Regularly Arranged
6.2.2.1.3.1.2.1
6.2.2.2 Muscle Tissue
6.2.2.2.1 Introduction
6.3 Plantar Foot and Posterior Heal
6.3.1 Functional Anatomy, Physiology, and Pathology
6.3.1.1 Introduction
6.3.1.1.1
6.3.1.2 Connective Tissue Structures
6.3.1.2.1 Plantar Aponeurosis (a-paw-neurosis)
6.3.1.2.1.1
6.3.1.2.2 Lateral Cord of the Plantar Aponeurosis
6.3.1.2.2.1
6.3.1.2.3 Plantar Fascia (fā-si-ă)
6.3.1.2.3.1
6.3.1.2.4 Plantar Ligaments
6.3.1.2.4.1 Long Plantar Ligament
6.3.1.2.4.1.1
6.3.1.2.4.2 Plantar Calcaneocuboid Ligament (Short Plantar Ligament)
6.3.1.2.4.2.1
6.3.1.2.4.3 Plantar Calcaneonavicular (Spring) Ligament
6.3.1.2.4.3.1
6.3.1.2.4.4 Retinaculum of foot/Fascia Around the Ankle
6.3.1.2.4.4.1
6.3.1.2.4.4.2 Laciniate Ligament
6.3.1.2.4.4.2.1
6.3.1.2.4.4.3 Peroneal Retinacula
6.3.1.2.4.4.3.1
6.3.1.2.4.5 Synovial (Mucous) Sheaths of the Tendons Around the Ankle
6.3.1.2.4.5.1
6.3.1.3 Foot and Toe Muscles
6.3.1.3.1 Introduction
6.3.1.3.1.1
6.3.1.3.2 Lateral (Peroneal) Compartment
6.3.1.3.2.1
6.3.1.3.2.2 Peroneus Brevis
6.3.1.3.2.2.1
6.3.1.3.2.3 Peroneus Longus
6.3.1.3.2.3.1
6.3.1.3.3 Posterior Compartment
6.3.1.3.3.1
6.3.1.3.3.2 Posterior Superficial Compartment
6.3.1.3.3.2.1 Gastrocnemius
6.3.1.3.3.2.1.1
6.3.1.3.3.2.2 Plantaris
6.3.1.3.3.2.2.1
6.3.1.3.3.2.3 Soleus
6.3.1.3.3.2.3.1
6.3.1.3.3.3 Posterior Deep Compartment
6.3.1.3.3.3.1 Flexor Digitorum Longus
6.3.1.3.3.3.1.1
6.3.1.3.3.3.2 Flexor Hallucis Longus
6.3.1.3.3.3.2.1
6.3.1.3.3.3.3 Tibialis Posterior
6.3.1.3.3.3.3.1
6.3.1.4 Intrinsic Foot Muscles
6.3.1.4.1
6.3.1.4.2 Dorsal Muscles
6.3.1.4.2.1 Extensor Digitorum Brevis
6.3.1.4.2.1.1
6.3.1.4.2.2 Extensor Hallucis Brevis
6.3.1.4.2.2.1
6.3.1.4.3 Plantar Muscles
6.3.1.4.3.1 Plantar First Superficial Layer
6.3.1.4.3.1.1 Abductor Digiti Minimi (Foot)
6.3.1.4.3.1.1.1
6.3.1.4.3.1.2 Abductor Hallucis
6.3.1.4.3.1.2.1
6.3.1.4.3.1.3 Flexor Digitorum Brevis
6.3.1.4.3.1.3.1
6.3.1.4.3.2 Plantar Second Layer
6.3.1.4.3.2.1 Lumbricals
6.3.1.4.3.2.1.1
6.3.1.4.3.2.2 Quadratus Plantae
6.3.1.4.3.2.2.1
6.3.1.4.3.3 Plantar Third Layer
6.3.1.4.3.3.1 Adductor Hallucis
6.3.1.4.3.3.1.1
6.3.1.4.3.3.2 Flexor Digiti Minimi Brevis
6.3.1.4.3.3.2.1
6.3.1.4.3.3.3 Flexor Hallucis Brevis
6.3.1.4.3.3.3.1
6.3.1.4.3.4 Plantar Fourth Deep Layer
6.3.1.4.3.4.1 Dorsal Interossei
6.3.1.4.3.4.1.1
6.3.1.4.3.4.2 Plantar Interossei
6.3.1.4.3.4.2.1
6.3.1.5 Neurology
6.3.1.5.1 Dermatomes
6.3.1.5.1.1
6.3.1.5.2 Major Nerve Supply
6.3.1.5.2.1
6.3.1.5.2.2 Cutaneous Nerves
6.3.1.5.2.2.1 Saphenous
6.3.1.5.2.2.1.1
6.3.1.5.2.2.2 Medial plantar (tibial)
6.3.1.5.2.2.2.1
6.3.1.5.2.2.3 Lateral plantar
6.3.1.5.2.2.3.1
6.3.1.5.2.2.4 Medial Sural Cutaneous Nerve
6.3.1.5.2.2.4.1
6.3.1.5.2.2.5 Medial Calcaneal (Tibial)
6.3.1.5.2.2.5.1
6.3.1.5.2.3 Motor Nerves
6.3.1.5.2.3.1
6.3.1.5.2.3.2 Articular Branches
6.3.1.5.2.3.2.1 Medial Plantar Nerve
6.3.1.5.2.3.2.1.1
6.3.1.5.2.3.2.2 Lateral Plantar Nerve
6.3.1.5.2.3.2.2.1
6.3.1.6 Osteology-Tarsals, Metatarsals, and Phalanges
6.3.1.6.1 Tarsus (Tarsals) (7)
6.3.1.6.1.1
6.3.1.6.1.2 Posterior Tarsus
6.3.1.6.1.2.1
6.3.1.6.1.2.2 Talus
6.3.1.6.1.2.2.1
6.3.1.6.1.2.2.2 Body
6.3.1.6.1.2.2.2.1
6.3.1.6.1.2.2.3 Neck
6.3.1.6.1.2.2.3.1
6.3.1.6.1.2.3 Calcaneus (kal-KĀ-nē-us)
6.3.1.6.1.2.3.1
6.3.1.6.1.3 Anterior Tarsus
6.3.1.6.1.3.1
6.3.1.6.1.3.2 Cuboid Bone
6.3.1.6.1.3.2.1
6.3.1.6.1.3.2.2 Dorsal Surface
6.3.1.6.1.3.2.2.1
6.3.1.6.1.3.2.3 Plantar Surface
6.3.1.6.1.3.2.3.1
6.3.1.6.1.3.2.4 Lateral Surface
6.3.1.6.1.3.2.4.1
6.3.1.6.1.3.2.5 Posterior Surface
6.3.1.6.1.3.2.5.1
6.3.1.6.1.3.2.6 Anterior Surface
6.3.1.6.1.3.2.6.1
6.3.1.6.1.3.2.7 Medial Surface
6.3.1.6.1.3.2.7.1
6.3.1.6.1.3.3 Navicular Bone
6.3.1.6.1.3.3.1
6.3.1.6.1.3.3.2 Anterior Surface
6.3.1.6.1.3.3.2.1
6.3.1.6.1.3.3.3 Posterior Surface
6.3.1.6.1.3.3.3.1
6.3.1.6.1.3.3.4 Dorsal Surface
6.3.1.6.1.3.3.4.1
6.3.1.6.1.3.3.5 Plantar Surface
6.3.1.6.1.3.3.5.1
6.3.1.6.1.3.3.6 Medial Surface
6.3.1.6.1.3.3.6.1
6.3.1.6.1.3.3.7 Lateral Surface
6.3.1.6.1.3.3.7.1
6.3.1.6.1.3.4 First Cuneiform Bone
6.3.1.6.1.3.4.1
6.3.1.6.1.3.5 Second Cuneiform Bone
6.3.1.6.1.3.5.1
6.3.1.6.1.3.6 Third Cuneiform Bone
6.3.1.6.1.3.6.1
6.3.1.6.2 Metatarsus (5)
6.3.1.6.2.1
6.3.1.6.3 Phalanges (14)
6.3.1.6.3.1
6.3.1.6.4 Total Bones of Foot=26
6.3.1.6.5 Arches of the Foot
6.3.1.6.5.1
6.3.1.6.5.2 Longitudinal Arch
6.3.1.6.5.2.1
6.3.1.6.5.2.2 Medial Longitudinal Arch
6.3.1.6.5.2.2.1
6.3.1.6.5.2.3 Lateral Longitudinal Arch
6.3.1.6.5.2.3.1
6.3.1.6.5.3 Transverse Arch
6.3.1.6.5.3.1
6.3.1.7 Arthrology (ar-THROL-ō-jē; arthro=joint; logos=sturdy of)
6.3.1.7.1 Introduction
6.3.1.7.1.1
6.3.1.7.2 Classification of Joints
6.3.1.7.2.1 Functional
6.3.1.7.2.1.1
6.3.1.7.2.1.2 Synarthroses (sin-ar-THRŌ-sēz))
6.3.1.7.2.1.2.1
6.3.1.7.2.1.3 Amphiarthroses (am-fē –ar-THRŌ-sēz)
6.3.1.7.2.1.3.1
6.3.1.7.2.1.4 Diarthroses
6.3.1.7.2.1.4.1
6.3.1.7.2.2 Structural
6.3.1.7.2.2.1
6.3.1.7.2.2.2 Fibrous Joints
6.3.1.7.2.2.2.1 Syndesmosis (Sin’-dez-MŌ-sis)
6.3.1.7.2.2.2.1.1
6.3.1.7.2.2.3 Synovial Joints
6.3.1.7.2.2.3.1 Structure
6.3.1.7.2.2.3.1.1
6.3.1.7.2.2.3.1.2 Accessory Ligaments
6.3.1.7.2.2.3.1.3
6.3.1.7.2.2.3.1.4 Bursae
6.3.1.7.2.2.3.1.5
6.3.1.7.3 Types of Synovial Joints
6.3.1.7.3.1
6.3.1.7.3.2 Gliding (arthrodia (ar-THRŌ-dē-a)
6.3.1.7.3.2.1
6.3.1.7.3.3 Hinge (JIN-gli-mus)
6.3.1.7.3.3.1
6.3.1.7.3.4 Ellipsoidal (KON-di-loyd)
6.3.1.7.3.4.1
6.3.1.7.3.5 Saddle (Reciprocal Reception)
6.3.1.7.3.5.1
6.3.1.7.3.6 Ball and Socket spheroid (SFĒ-royd)
6.3.1.7.3.6.1
6.3.1.7.4 Joints of the Foot
6.3.1.7.4.1 Tibiofibular Joint
6.3.1.7.4.1.1
6.3.1.7.4.2 Talocrural (Ankle) Joint (ta’’lo-krōōr’al)
6.3.1.7.4.2.1
6.3.1.7.4.3 Subtalar/Talocalcaneal (ta’’lo-kal-ka-ne-al)
6.3.1.7.4.3.1
6.3.1.7.4.4 Talocalcaneonavicular (TCN)
6.3.1.7.4.4.1
6.3.1.7.4.5 Calcaneocuboid
6.3.1.7.4.5.1
6.3.1.7.4.6 Metatarsophalangeal Joints (MP)
6.3.1.7.4.6.1
6.3.1.7.4.7 Interphalangeal Joints of Toes (IP)
6.3.1.7.4.7.1
6.3.1.7.4.8 Intercuneiform and Cuneocuboid
6.3.1.7.4.8.1
6.3.1.7.4.9 Tarsometatarsal
6.3.1.7.4.9.1
6.3.1.7.4.10 Intermetatarsal
6.3.1.7.4.10.1
6.3.1.7.5 Synovial Membranes of Foot (Review)
6.3.1.7.5.1
6.3.1.7.5.2 Subtalar/Talocalcaneal
6.3.1.7.5.3 Talocalcaneal
6.3.1.7.5.4 Talocalcaneonavicular
6.3.1.7.5.5 Calcaneocuboid
6.3.1.7.5.6 Cuneonavicular
6.3.1.7.5.7 Intercuneiform, Cuneocuboid, and cuneiform (2nd & 3rd)/metatarsal (2nd, 3rd, & 4th)
6.3.1.7.5.8 1st cuneiform with great toe
6.3.1.7.5.9 Cuboid & Metatarsal (4th & 5th)
6.3.1.7.5.10 Navicular & Cuboid (Rare)
6.3.1.7.6 Achilles Tendon Bursa
6.3.1.7.6.1 Introduction
6.3.1.7.6.1.1
6.3.1.7.6.2 Retrocalcaneal Bursa
6.3.1.7.6.2.1
6.3.1.7.6.3 Calcaneal Bursa
6.3.1.8 Vascular
6.3.1.8.1 Arteries of the Foot
6.3.1.8.1.1 Dorsalis Pedis Artery (Dŏr-sălis Pēdĭs)
6.3.1.8.1.1.1
6.3.1.8.1.2 Medial And Lateral Plantar Arteries
6.3.1.8.1.2.1
6.3.1.8.2 Veins of the Foot
6.3.1.8.2.1 Dorsal Venous Arch (Medial)
6.3.1.8.2.1.1
6.3.1.8.2.2 Dorsal Venous Arch (Lateral)
6.3.1.8.2.2.1
6.3.1.9 Examination-Surface Anatomy
6.3.1.9.1 Bony Palpation
6.3.1.9.1.1 Head of the First Metatarsal Bone and the Metatarsophalangeal Joint
6.3.1.9.1.1.1
6.3.1.9.1.2 First Metatarsocuneiform
6.3.1.9.1.2.1
6.3.1.9.1.3 Navicular Tubercle
6.3.1.9.1.3.1
6.3.1.9.1.4 Head of the Talus
6.3.1.9.1.4.1
6.3.1.9.1.5 Medial Malleolus
6.3.1.9.1.5.1
6.3.1.9.1.6 Sustentaculum Tali
6.3.1.9.1.6.1
6.3.1.9.1.7 Medial Tubercle of the Talus
6.3.1.9.1.7.1
6.3.1.9.1.8 Fifth Metatarsal Bone; Fifth Metatarsophalangeal Joint
6.3.1.9.1.8.1
6.3.1.9.1.9 Calcaneus
6.3.1.9.1.9.1
6.3.1.9.1.10 Peroneal Tubercle
6.3.1.9.1.10.1
6.3.1.9.1.11 Dome of the Talus
6.3.1.9.1.11.1
6.3.1.9.1.12 Inferior Tibiofibular Joint
6.3.1.9.1.12.1
6.3.1.9.1.13 Dome of the Calcaneus
6.3.1.9.1.13.1
6.3.1.9.1.14 Medial Tubercle of Calcaneus
6.3.1.9.1.14.1
6.3.1.9.1.15 Metatarsal Heads
6.3.1.9.1.15.1
6.3.1.9.2 Soft Tissue Palpation
6.3.1.9.2.1 Head of the First Metatarsal Bone
6.3.1.9.2.1.1
6.3.1.9.2.2 Navicular Tubercle and the Talar Head
6.3.1.9.2.2.1
6.3.1.9.2.3 Medial Malleolus Structures
6.3.1.9.2.3.1
6.3.1.9.2.3.2 Tibialis Posterior Tendon
6.3.1.9.2.3.2.1
6.3.1.9.2.3.3 Flexor Digitorum Longus Tendon
6.3.1.9.2.3.3.1
6.3.1.9.2.3.4 Flexor Hallucis Longus Tendon
6.3.1.9.2.3.4.1
6.3.1.9.2.3.5 Posterior Tibial Artery
6.3.1.9.2.3.5.1
6.3.1.9.2.3.6 Tibial Nerve
6.3.1.9.2.3.6.1
6.3.1.9.2.3.7 Long Saphenous Vein
6.3.1.9.2.3.7.1
6.3.1.9.2.4 Peroneus Longus and Brevis Tendons
6.3.1.9.2.4.1
6.3.1.9.2.5 Head of Fifth Metatarsal
6.3.1.9.2.5.1
6.3.1.9.2.6 Achilles Tendon
6.3.1.9.2.6.1
6.3.1.9.2.7 Retrocalcaneal Bursa
6.3.1.9.2.7.1
6.3.1.9.2.8 Calcaneal Bursa
6.3.1.9.2.8.1
6.3.1.9.2.9 Plantar Aponeurosis
6.3.1.9.2.9.1
6.3.1.9.3 Muscle Testing
6.3.1.9.3.1
6.3.1.10 Biomechanics
6.3.1.10.1 Introduction
6.3.1.10.1.1 Planes
6.3.1.10.1.1.1
6.3.1.10.1.1.2 Sagittal Plane
6.3.1.10.1.1.2.1
6.3.1.10.1.1.3 Coronal (Frontal) Plane
6.3.1.10.1.1.3.1
6.3.1.10.1.1.4 Transverse (Horizontal) Plane
6.3.1.10.1.1.4.1
6.3.1.10.1.2 Axes
6.3.1.10.1.2.1
6.3.1.10.1.2.2 Sagittal Axis
6.3.1.10.1.2.2.1
6.3.1.10.1.2.3 Coronal (Frontal) Axis
6.3.1.10.1.2.3.1
6.3.1.10.1.2.4 Longitudinal Axis
6.3.1.10.1.2.4.1
6.3.1.10.1.2.5 Exceptions
6.3.1.10.1.2.5.1
6.3.1.10.1.3 Center of Gravity
6.3.1.10.1.3.1
6.3.1.10.1.4 Line of Gravity
6.3.1.10.1.4.1
6.3.1.10.1.5 Lever Systems and Leverage
6.3.1.10.1.5.1
6.3.1.10.1.5.2 First-class Levers
6.3.1.10.1.5.2.1
6.3.1.10.1.5.3 Second-class levers
6.3.1.10.1.5.3.1
6.3.1.10.1.5.4 Third-class Levers
6.3.1.10.1.5.4.1
6.3.1.10.1.5.5 Leverage
6.3.1.10.1.5.5.1
6.3.1.10.1.6 Gait Analysis
6.3.1.10.1.6.1
6.3.1.10.1.6.2 Stance Phase
6.3.1.10.1.6.2.1
6.3.1.10.1.6.3 Swing Phase
6.3.1.10.1.6.3.1
6.3.1.10.1.6.4 Width of the base (2”-4”)
6.3.1.10.1.6.4.1
6.3.1.10.1.6.5 Body’s center of gravity (2” S2) (Oscillates vertically 2”)
6.3.1.10.1.6.5.1
6.3.1.10.1.6.6 Knee remains flexed during all components of stance phase (except heel strike)
6.3.1.10.1.6.6.1
6.3.1.10.1.6.7 Pelvis and trunk shift laterally (1” Laterally)
6.3.1.10.1.6.7.1
6.3.1.10.1.6.8 Average length of a step is approximately 15 inches
6.3.1.10.1.6.8.1
6.3.1.10.1.6.9 Average adult walks at a cadence of approximately 90 to 120 steps per minute
6.3.1.10.1.6.9.1
6.3.1.10.1.6.10 During swing phase, the pelvis rotates 40° forward
6.3.1.10.1.6.10.1
6.3.1.10.1.6.11 Stance phase
6.3.1.10.1.6.11.1 Heel Strike-Foot
6.3.1.10.1.6.11.1.1
6.3.1.10.1.6.11.2 Midstance=Foot
6.3.1.10.1.6.11.2.1
6.3.1.10.1.6.11.3 Push-Off=Foot
6.3.1.10.1.6.11.3.1
6.3.1.10.1.7 Movements of Specific Joints
6.3.1.10.1.7.1 Ankle Joint
6.3.1.10.1.7.1.1
6.3.1.10.1.7.1.2 Flexion (Plantar Flexion) and Extension (Dorsiflexion)
6.3.1.10.1.7.1.2.1
6.3.1.10.1.7.2 Subtalar Joint and Transverse Tarsal Joints
6.3.1.10.1.7.2.1
6.3.1.10.1.7.2.2 Supination and Pronation
6.3.1.10.1.7.2.2.1
6.3.1.10.1.7.3 Transverse Tarsal Joints
6.3.1.10.1.7.3.1
6.3.1.10.1.7.3.2 Adduction and Abduction
6.3.1.10.1.7.3.2.1
6.3.1.10.1.7.3.3 Inversion
6.3.1.10.1.7.3.3.1
6.3.1.10.1.7.3.4 Eversion
6.3.1.10.1.7.3.4.1
6.3.1.10.1.7.4 Metatarsophalangeal Joints
6.3.1.10.1.7.4.1
6.3.1.10.1.7.4.2 Flexion and extension
6.3.1.10.1.7.4.2.1
6.3.1.10.1.7.4.3 Adduction and Abduction
6.3.1.10.1.7.4.3.1
6.3.1.10.1.7.5 Interphalangeal Joints of toes
6.3.1.10.1.7.5.1
6.3.1.10.1.7.5.2 Flexion and extension
6.3.1.10.1.7.5.2.1
6.3.1.10.1.8 Structural Alignment
6.3.1.10.1.8.1
6.3.1.10.1.9 Arthrokinematics of the Ankle-
6.3.1.10.1.9.1 Foot Complex
6.3.1.10.1.9.1.1 Ankle Mortise Joint
6.3.1.10.1.9.1.1.1
6.3.1.10.1.9.1.2 Subtalar Joint
6.3.1.10.1.9.1.2.1
6.3.1.10.1.9.1.3 Neutral Position of a Joint
6.3.1.10.1.9.1.3.1
6.3.1.10.1.9.1.4 Transverse Tarsal Joints: Talonavicular and Calcaneocuboid Joints
6.3.1.10.1.9.1.4.1
6.3.1.10.1.10 Osteokinematics of the Ankle-Foot Complex
6.3.1.10.1.10.1 Terminology
6.3.1.10.1.10.1.1 Inversion-Eversion
6.3.1.10.1.10.1.1.1
6.3.1.10.1.10.1.2 Abduction-Adduction
6.3.1.10.1.10.1.2.1
6.3.1.10.1.10.1.3 Internal-External Rotation
6.3.1.10.1.10.1.3.1
6.3.1.10.1.10.1.4 Plantar flexion-Dorsiflexion
6.3.1.10.1.10.1.4.1
6.3.1.10.1.10.1.5 Pronation-Supination
6.3.1.10.1.10.1.5.1
6.3.1.10.1.10.1.6 Pronated Foot-Supinated Foot
6.3.1.10.1.10.1.6.1
6.3.1.10.1.10.1.7 Valgus-Varus
6.3.1.10.1.10.1.7.1
6.3.1.10.1.10.2 Orientation of Joint Axes and the Effect on Movement
6.3.1.10.1.10.2.1
6.3.1.10.1.10.3 Ankle and Foot During Gait
6.3.1.10.1.10.3.1