Copyright Ted Nissen 2003
1.2 Cutaneous Nerves-Head 1 (31)
1.3 Cutaneous Nerves-Head 2 (32)
1.4 Cutaneous Nerves-Arms (33)
1.5 Cutaneous Nerves-Hands (34)
1.6 Cutaneous Nerves-Back (36)
1.7 Cutaneous Nerves-Front of Chest
(36)
1.8 Cutaneous Nerves-Foot (35)
1.9 Cutaneous Nerves-Legs (35)
2.18 ANSA CERVICALIS (ANSA HYPOGLOSSI)
2.20 RECTUS CAPITIS LATERALIS N.
2.21 RECTUS CAPITIS ANTERIOR N.
2.33 THORACODORSAL N. (MIDDLE
SUBSCAPULAR N.)
3.4 MEDIAL BRACHIAL CUT
N.(FLASH;MEDIAL CUT)(GRAY;LESSER INTERNAL CUT,N. OF WRISBERG)
3.7 MED ANTEBRACHIAL CUT
N.(FLASH;MEDIAL CUTANEOUS N. OF
FOREARM),(GRAY; INTERNAL CUT N.)
5.1 12TH THORACIC INTERCOSTAL (SUB
COSTAL) 35.01
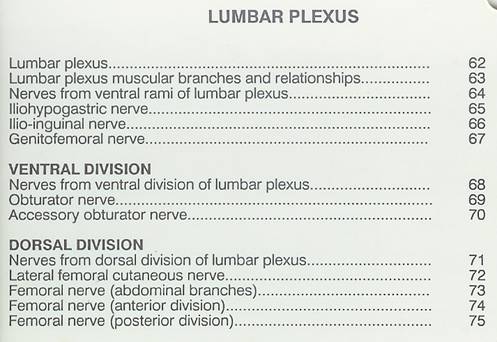
5.2 Lumbar Plexus (Spinal Segments
& Nerves) (61)
5.4 Lumbar Plexus (Muscular Branches
and Relationships) (63)
5.5 Nerves from Ventral Rami of
Lumbar Plexus (64)
5.6 Iliohypogastric Nerve (65)
(Blank)
5.8 Ilio-Inquinal Nerve (66) (Blank)
5.10 Genitofemoral Nerve (67) (Blank)
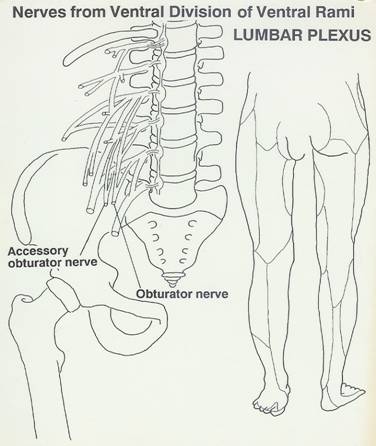
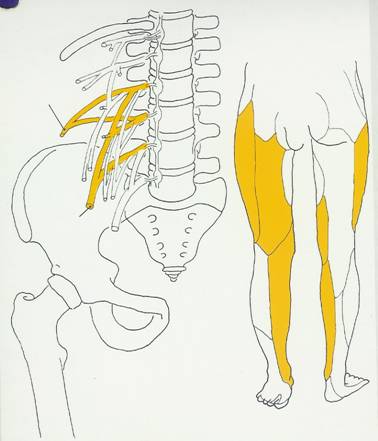
5.12 Nerves from Ventral Division of
Ventral Rami Lumbar Plexus (68)
5.13 Obturator Nerve (69) (Blank)
5.15 Accessory Obturator Nerve (70)
(Blank)
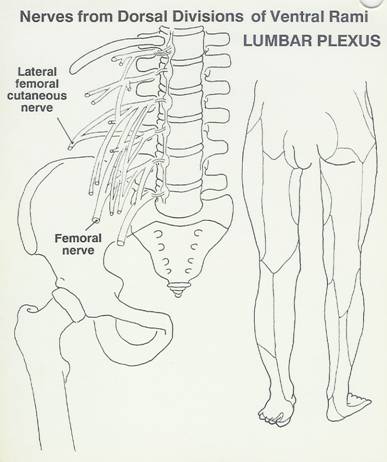
5.17 Lumbar Plexus (Nerves from Dorsal
Divisions-Ventral Rami (71)
5.18 Lateral Cutaneous Femoral Nerve
(72) (Blank)
5.19 Femoral Nerve (Abdominal Branches)
(73) (Blank)
5.20 Femoral Nerve (Anterior Division)
(74) (Blank)
5.23 Femoral Nerve (Posterior Division)
(75)
5.24 Sacral Plexus (Spinal Segments
& Nerves) (76)
5.25 Sacral Plexus (L4, L5, S1, S2, S3)
(77)
5.26 Sacral Plexus (Nerves from Ventral
Divisions of Ventral Rami) (78)
5.27 Sacral Plexus (Nerves from Dorsal
Divisions of Ventral Rami) (79)
5.28 QUADRATUS FEMORIS N. (80)
5.33 POSTERIOR FEMORAL CUTANEOUS (85)
5.35 Tibial Nerve (Branches Arising
between Gastrocnemius Heads) (87)
5.36 Tibial Nerve (Branches Arising in
the Leg) (88)
5.37 Tibial Nerve (Medial Sural and
Medial Calcanean Cutaneous Branches) (89)
5.38 Medial Plantar (Tibial) (90)
5.39 Lateral Plantar Nerve &
Superficial Branch (Tibial) (91)
5.40 Lateral Plantar Nerve Deep Branch
(Tibial) (92)
5.41 Common Peroneal (Fibular) Nerve
(93)
5.42 Deep Peroneal (Anterior Tibial)
Nerve (Branches Arising in the Leg) (94)
5.43 Deep Peroneal Medial and Lateral
Terminal Branches (95)
5.44 Superficial Peroneal Nerve (96)
5.45 Superficial Peroneal Nerve Medial
and Lateral Terminal Branches (97)
5.46 Perforating Cutaneous Nerve (98)
(Blank)
5.47 Sacral Muscular Branches (4th
Sacral) (99) (Blank)
5.48 Pudendal Nerve: Inferior Rectal
Branch (Inferior Hemeorrhoidal Nerve) (100) (Blank)
5.49 Pudendal Nerve (Perineal Branch)
(101) (Blank)
5.50 Pudendal Nerve (Dorsal Nerve of
Penis or Clitoris) (102) (Blank)
6.7 1ST DORSAL RAMUS(SUBOCCIPITAL N)
6.8 2ND DOR RAMUS(GREATER OCCIPITAL
N)
6.12 LOWR THOR DOR RAM (T7-12)
6.14 UPPER SACRAL DOR RAM (S1-3)
6.15 LWR SAC&COC DR R(ANOCOCCYGEAL
N) (S4,5,C01)
1 Cutaneous Nerves
All
1.1 Index
1.1.1 http://www.anatomyfacts.com/Muscle/cutaneousnerves.htm
1.2 Cutaneous
Nerves-Head 1 (31)
1.2.1 http://www.anatomyfacts.com/Muscle/Illustrations.htm#CNH1
1.3 Cutaneous
Nerves-Head 2 (32)
1.3.1 http://www.anatomyfacts.com/Muscle/Illustrations.htm#CNH2
1.4 Cutaneous
Nerves-Arms (33)
1.4.1 http://www.anatomyfacts.com/Muscle/Illustrations.htm#CNA
1.5 Cutaneous
Nerves-Hands (34)
1.5.1 http://www.anatomyfacts.com/Muscle/Illustrations.htm#CNH
1.6 Cutaneous
Nerves-Back (36)
1.6.1 http://www.anatomyfacts.com/Muscle/Illustrations.htm#CNB
1.7 Cutaneous
Nerves-Front of Chest (36)
1.7.1 http://www.anatomyfacts.com/Muscle/Illustrations.htm#CNFC
1.8 Cutaneous
Nerves-Foot (35)
1.8.1 http://www.anatomyfacts.com/Muscle/Illustrations.htm#CNF
1.9 Cutaneous
Nerves-Legs (35)
1.9.1 http://www.anatomyfacts.com/Muscle/Illustrations.htm#CNL
2 HEAD & NECK
2.1 OLFACTORY
Back
Table of Contents References
2.1.1 DESCRIPTION # 1:
PATH, FUNCTION
2.1.1.1
SMELL
2.1.2 ROOTS
2.1.2.1
CN 1
2.2
OPTIC
2.2.1 DESCRIPTION # 1: PATH,
FUNCTION
2.2.1.1
VISION
2.2.2 ROOTS
2.2.2.1
CN 2
2.3 OCULOMOTOR
2.3.1 DESCRIPTION # 1:
PATH, FUNCTION
2.3.1.1
EYE MOVEMENTS; MOVEMENT OF EYE BALL, EYELID, CONSTRICTION OF
LENS FOR NEAR VISION
2.3.2 MUSCULAR
BRANCHES(OCCULO)
2.3.2.1
SUPERIOR RECTUS
2.3.2.2
INFERIOR RECTUS
2.3.2.3
MEDIAL RECTUS
2.3.2.4
INFERIOR OBLIQUE
2.3.2.5
LEVATOR PALPEBRAE SUPERIORIS
2.3.3 ROOTS
2.3.3.1
CN 3
2.4 TROCHELEAR
Back
Table of Contents References
2.4.1 DESCRIPTION # 1:
PATH, FUNCTION
2.4.1.1
EYE MOVEMENTS; EYE BALL MEVEMENT
2.4.2 MUSCULAR BRANCHES(TROCH)
2.4.2.1
SUPERIOR OBLIQUE
2.4.3 ROOTS
2.4.3.1
CN4
2.5 TRIGEMINAL
Back
Table of Contents References
2.5.1 DESCRIPTION # 1:
PATH, FUNCTION
2.5.1.1
SENSATION TO FACE, CHEWING. SUPRFICIAL SEN=PONS VAROLII,
DEEP SEN= LONG TRACT OF MEDULLA,LWR SEN=SUBSTANIA GELATINOSA ROLANDO,
SEMILUNAR(GASSERIAN) GANGLION=LODGED IN AN OSTEO-FIBROUS SPACE THE CAVUM
MECKELII NEAR THE APEX OF THE PETROUS PORTION OF THE TEMPORAL BONE.
2.5.2 Illustration
2.5.2.1
Reference Number
2.5.2.1.1 31.01
2.5.2.2
Illustration Link
2.5.2.2.1 Trigeminal
2.5.3 NEUROLOGICAL
BRANCHES
2.5.3.1
OPHTHALMIC (TRI)
2.5.3.1.1
DESCRIPTION # 1: PATH, FUNCTION
2.5.3.1.1.1
PASSES
FORWARD ALONG OUTER WALL OF CAVERNOUS SINUS AND JUST BEFORE ENTERING THE ORBIT
THR T SPHENOIDAL FISSURE DIVIDES IN THRE BRANCHES LACHRYMAL, FRONTAL &
NASAL. IT THEN PASSES THRU SUP ORBITAL FISSURE
2.5.3.1.2
DESCRIPTION # 2: CUTANEOUS AREA, ADDITIONAL
COMMENTS
2.5.3.1.2.1
U
EYELID,MUCOUS LINING OF THE EYE,SKIN OF EYEBROW,EYEBALL,LACRIMAL GL,NAS CAVITY,
SIDE OF NOSE, FOREHEAD,A 1/2 OF SCLP.
2.5.3.1.3
Reference
Number
2.5.3.1.3.1 31.011
2.5.3.1.4 Illustration Link
2.5.3.1.4.1 Ophthalmic
2.5.3.2
MAXILLARY (TRI)
2.5.3.2.1
DESCRIPTION # 1: PATH, FUNCTION
2.5.3.2.1.1
FORAMEN
ROTUNDUM
2.5.3.2.2
DESCRIPTION # 2: CUTANEOUS AREA, ADDITIONAL
COMMENTS
2.5.3.2.2.1
MUCOSA
OF NOSE, PALATE, PHARYNX, U TEETH, U LIPL EYELID.
2.5.3.2.3
Reference
Number
2.5.3.2.3.1 31.012
2.5.3.2.4 Illustration Link
2.5.3.2.4.1 Maxillary
2.5.3.3
MANDIBULAR (TRI)
2.5.3.3.1
DESCRIPTION # 1: PATH, FUNCTION
2.5.3.3.1.1
FORAMEN
OVALE
2.5.3.3.2
DESCRIPTION # 2: CUTANEOUS AREA, ADDITIONAL
COMMENTS
2.5.3.3.2.1
A
2/3 TOUGUE L TEETH, SKIN O MANDIBLE,CHECK & MUCOSA,SIDE O HEAD IN F OF EAR,
2.5.3.3.3
Reference
Number
2.5.3.3.3.1 31.011
2.5.3.3.4 Illustration Link
2.5.3.3.4.1 Mandibular
2.5.4 MUSCULAR BRANCHES
(MANDIBULAR)
2.5.4.1
MASSETER
2.5.4.2
TEMPORALIS
2.5.4.3
MEDIAL PTERYGOID
2.5.4.4
LATERAL PTERYGOID
2.5.4.5
TENSOR VELI PALATINI
2.5.4.6
DIGASTRIC (ANTERIOR BELLY)
2.5.4.7
MYLOHYOID
2.5.5 ROOTS
2.5.5.1
CN 5
2.6 ABDUCENS
Back
Table of Contents References
2.6.1 DESCRIPTION # 1:
PATH, FUNCTION
EYE MOVEMENTS; EYE BALL MEVEMENT
2.6.2 MUSCULAR
BRANCHES(ABDUCENS)
2.6.2.1
LATERAL RECTUS
2.6.3 ROOTS
2.6.3.1
CN 6
2.7 FACIAL
Back
Table of Contents References
2.7.1 DESCRIPTION # 1:
PATH, FUNCTION
FACIAL EXPRESSION, TASTE,SALIVA SECRETION, TEARS.
2.7.2 MUSCULAR BRANCHES
(FACIAL)
2.7.2.1
FRONTALIS (EPICRANIUS 1)
2.7.2.2
OCCIPITALIS (EPICRANIUS 2)
2.7.2.3
ORBICULARIS ORIS
2.7.2.4
ZYGOMATICUS MAJOR
2.7.2.5
LEVATOR LABIL SUPERIORIS
2.7.2.6
DEPRESSOR LABII INFERIORIS
2.7.2.7
BUCCINATOR
2.7.2.8
MENTALIS
2.7.2.9
PLATYSMA
2.7.2.10
RISORIUS
2.7.2.11
ORBICULARIS OCULI
2.7.2.12
CORRUGATOR SUPERCILLI
2.7.2.13
STYLOHYOID
2.7.2.14
DIAGASTRIC (POSTERIOR BELLY)
2.7.2.15
STAPEDIUS
2.7.3 CUTANEOUS (FACIAL)
2.7.3.1
DESCRIPTION # 1: PATH, FUNCTION
TASTE IN ANTERIOR TWO-THIRDS OF TONGUE. SENSATION TO SOFT PALATE. INNERVATION OF SALIVARY GLANDS.
2.7.4 ROOTS
2.7.4.1
CN 7
2.8 ACOUSTIC
2.8.1 DESCRIPTION # 1:
PATH, FUNCTION
HEARING, EQUILIBRIUM
2.8.2 ROOTS
2.8.2.1
CN 8
2.9 GLOSSOPHARYNGEAL
Back
Table of Contents References
2.9.1 DESCRIPTION # 1:
PATH, FUNCTION
TASTE, SPEECH
2.9.2 MUSCULAR
BRANCHES(GLOSSO)
2.9.2.1
STYLOPHARYNGEUS
2.9.3 CUTANEOUS(GLOSSO)
TASTE IN POSTERIOR 2/3 RDS OF TONGUE. SENSATION TO FAUCES, TONSILS, PHARYNX, AND SOFT PALATE.
2.9.4 ROOTS
2.9.4.1
CN 9
2.10 VAGUS
Back
Table of Contents References
2.10.1
DESCRIPTION # 1: PATH, FUNCTION
PARASYMPATHETIC, VISERAL MUSCLE MOVEMENT, SENSATION FROM ORGANS
2.10.2
CUTANEOUS(VAGUS)
SENSORY FIBERS TO SKIN IN BACK OF AURICLE, POSTERIOR PORTION OF EXTERNAL ACOUSTIC MEATUS, PHARYNX, LARYNX, THORACIC AND ABDOMINAL VISCERA.
2.10.3
RECURRENT LARYNGEAL(VAGUS)
2.10.3.1
MUSCULAR BRANCHES(RECURR LARG)
2.10.3.1.1
POSTERIOR
CRICOARYTENOID
2.10.3.1.2
LATERAL
CRICOARYTENOID
2.10.3.1.3
ARYTENOID
2.10.3.1.4
THYROARYTENOID
2.10.4
EXTERNAL LARYNGEAL(VAGUS)
2.10.4.1
MUSCULAR BRANCHES(EXTER LARG)
2.10.4.1.1
CRICOTHYROID
2.10.5
PHARYNGEAL BRANCH(VAGUS)
2.10.5.1
MUSCULAR BRANCHES(PHARYN)
2.10.5.1.1
INFERIOR
CONSTRICTOR
ADDITIONAL INNERVATION: WITH FILIMENTS FROM SPINAL ACCESSARY NERVE WHICH TRAVELS THRU PHARYNGEAL PLEXUS.
2.10.5.1.2
MIDDLE
CONSTRICTOR
ADDITIONAL INNERVATION: WITH FILIMENTS FROM SPINAL ACCESSARY NERVE WHICH TRAVELS THRU PHARYNGEAL PLEXUS.
2.10.5.1.3
SUPERIOR
CONSTRICTOR
ADDITIONAL INNERVATION: WITH FILIMENTS FROM SPINAL ACCESSARY NERVE WHICH TRAVELS THRU PHARYNGEAL PLEXUS.
2.10.5.1.4
PALATOGLOSSUS
ADDITIONAL INNERVATION: WITH FILIMENTS FROM SPINAL ACCESSARY NERVE WHICH TRAVELS THRU PHARYNGEAL PLEXUS.
2.10.5.1.5
SALPINGOPHARYNGEUS
ADDITIONAL INNERVATION: WITH FILIMENTS FROM SPINAL ACCESSARY NERVE WHICH TRAVELS THRU PHARYNGEAL PLEXUS.
2.10.5.1.6
PALATOPHARYNGEUS
ADDITIONAL INNERVATION: WITH FILIMENTS FROM SPINAL ACCESSARY NERVE WHICH TRAVELS THRU PHARYNGEAL PLEXUS.
2.10.5.1.7
LEVATOR
VELI PALATINI
ADDITIONAL INNERVATION: WITH FILIMENTS FROM SPINAL ACCESSARY NERVE WHICH TRAVELS THRU PHARYNGEAL PLEXUS.
2.10.5.1.8
MUSCULUS
UVULAE
ADDITIONAL INNERVATION: WITH FILIMENTS FROM SPINAL ACCESSARY NERVE WHICH TRAVELS THRU PHARYNGEAL PLEXUS.
2.10.5.1.9
PALATOGLOSSUS
ADDITIONAL INNERVATION: WITH FILIMENTS FROM SPINAL ACCESSARY NERVE WHICH TRAVELS THRU PHARYNGEAL PLEXUS.
2.10.5.1.10
PALATOPHARYNGEUS
ADDITIONAL INNERVATION: WITH FILIMENTS FROM SPINAL ACCESSARY NERVE WHICH TRAVELS THRU PHARYNGEAL PLEXUS.
2.10.6
ROOTS
2.10.6.1
CN 10
2.10.7
References
2.10.7.1
2.11 SPINAL ACCESSORY
Back
Table of Contents References
2.11.1
DESCRIPTION # 1: PATH, FUNCTION
SWALLOWING, MOVEMENT OF HEAD
2.11.2
ROOTS
2.11.2.1
CN11
2.11.3
MUSCULAR BRANCHES(SPINL ACCES)
2.11.3.1
STERNOCLEIDOMASTOID
2.11.3.1.1
CARD=
21
2.11.3.1.2
INNERVATION
2.11.3.1.2.1
(XI(C1-5)
MOTOR)
2.11.3.2
TRAPEZIUS
2.11.3.2.1
CARD=
22
2.11.3.2.2
INNERVATION
2.11.3.2.2.1
(XI(C1-5)
MOTOR)
2.12 HYPOGLOSSAL
Back
Table of Contents References
2.12.1
DESCRIPTION # 1: PATH, FUNCTION
MOVEMENT OF TONGUE DURNING SPEECH AND SWALLOWING.
2.12.2
ROOTS
2.12.2.1
CN12
2.12.3
MUSCULAR BRANCHES(HYPO)
2.12.3.1
GENIOGLOSSUS
2.12.3.2
STYLOGLOSSUS
2.12.3.3
HYOGLOSSUS
2.12.3.4
STYLOHYOID
2.12.3.5
MYHLOHYOID
2.12.3.6
OMOHYOID(INFERIOR BELLY)
2.12.3.7
THYROHYOID(DECENDING HYPOGLOSSAL)
2.12.3.8
GENIOHYOID
2.12.3.9
INTRINSIC MUS OF TONGUE
2.13 LESSER OCCIPITAL
Back
Table of Contents References
2.13.1
DESCRIPTION # 1: PATH, FUNCTION-LESIONS
A FOCAL LESION WILL RESULT IN PARESTHESIA OR LACK OF SENSATION TO THE SKIN DESCRIBED IN THE CUTANEOUS SECTION OF THIS NERVE.
2.13.2
DESCRIPTION # 2: CUTANEOUS AREA, ADDITIONAL COMMENTS
MID NECK ALONG THE P BORDER OF SCM &PRT O MASTOID PRO A T SCALP BEH T LWAR & UPPER MEDIAN PRT O AURICLE.
2.13.3
ROOTS
2.13.3.1
C2-C3
2.13.3.2
SPINAL NERVE
2.13.3.3
VENTRAL
2.13.4
NUMBER
2.13.4.1
32.01
2.13.5
CARD
2.13.5.1
9
2.14 GREATER AURICULAR
Back
Table of Contents References
2.14.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
2.14.1.1
.
2.14.2
NUMBER
2.14.2.1
35
2.14.3
REFERENCE
2.14.3.1
2.14.4
ROOTS
2.14.4.1
2.14.4.2
Lumbar Plexus
2.14.4.3
VENTRAL
2.14.5
DIVISION
2.14.5.1
Dorsal Ventral
2.14.5.2
2.14.6
CUTANEOUS BRANCHES
2.14.6.1
2.14.6.1.1
2.14.6.2
2.14.6.2.1
.
2.14.7
ARTICULAR BRANCHES
2.14.7.1
2.14.7.1.1
2.14.8
MUSCULAR BRANCHES
2.14.8.1
2.14.8.2
2.14.8.3
2.14.8.4
2.14.8.5
2.14.8.6
2.15 TRANSVERSE (ANT)
CUT
Back
Table of Contents References
2.15.1
DESCRIPTION: PATH, FUNCTION,
LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
2.15.1.1
.
2.15.2
NUMBER
2.15.2.1
35
2.15.3
REFERENCE
2.15.3.1
2.15.4
ROOTS
2.15.4.1
2.15.4.2
Lumbar Plexus
2.15.4.3
VENTRAL
2.15.5
DIVISION
2.15.5.1
Dorsal Ventral
2.15.5.2
2.15.6
CUTANEOUS BRANCHES
2.15.6.1
2.15.6.1.1
2.15.6.2
2.15.6.2.1
.
2.15.7
ARTICULAR BRANCHES
2.15.7.1
2.15.7.1.1
2.15.8
MUSCULAR BRANCHES
2.15.8.1
2.15.8.2
2.15.8.3
2.15.8.4
2.15.8.5
2.15.8.6
2.16 SUPRACLAVICULAR
Back
Table of Contents References
2.16.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
2.16.1.1
.
2.16.2
NUMBER
2.16.2.1
35
2.16.3
REFERENCE
2.16.3.1
2.16.4
ROOTS
2.16.4.1
2.16.4.2
Lumbar Plexus
2.16.4.3
VENTRAL
2.16.5
DIVISION
2.16.5.1
Dorsal Ventral
2.16.5.2
2.16.6
CUTANEOUS BRANCHES
2.16.6.1
2.16.6.1.1
2.16.6.2
2.16.6.2.1
.
2.16.7
ARTICULAR BRANCHES
2.16.7.1
2.16.7.1.1
2.16.8
MUSCULAR BRANCHES
2.16.8.1
2.16.8.2
2.16.8.3
2.16.8.4
2.16.8.5
2.16.8.6
2.17 SUPRASCAPULAR
Back
Table of Contents References
2.17.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
2.17.1.1
.
2.17.2
NUMBER
2.17.2.1
35
2.17.3
REFERENCE
2.17.3.1
2.17.4
ROOTS
2.17.4.1
2.17.4.2
Lumbar Plexus
2.17.4.3
VENTRAL
2.17.5
DIVISION
2.17.5.1
Dorsal Ventral
2.17.5.2
2.17.6
CUTANEOUS BRANCHES
2.17.6.1
2.17.6.1.1
2.17.6.2
2.17.6.2.1
.
2.17.7
ARTICULAR BRANCHES
2.17.7.1
2.17.7.1.1
2.17.8
MUSCULAR BRANCHES
2.17.8.1
2.17.8.2
2.17.8.3
2.17.8.4
2.17.8.5
2.17.8.6
2.18
ANSA CERVICALIS (ANSA
HYPOGLOSSI)
Back
Table of Contents References
2.18.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
2.18.1.1
.
2.18.2
NUMBER
2.18.2.1
35
2.18.3
REFERENCE
2.18.3.1
2.18.4
ROOTS
2.18.4.1
2.18.4.2
Lumbar Plexus
2.18.4.3
VENTRAL
2.18.5
DIVISION
2.18.5.1
Dorsal Ventral
2.18.5.2
2.18.6
CUTANEOUS BRANCHES
2.18.6.1
2.18.6.1.1
2.18.6.2
2.18.6.2.1
.
2.18.7
ARTICULAR BRANCHES
2.18.7.1
2.18.7.1.1
2.18.8
MUSCULAR BRANCHES
2.18.8.1
2.18.8.2
2.18.8.3
2.18.8.4
2.18.8.5
2.18.8.6
2.19
PHRENIC (phrenic19)
Back
Table of Contents References
2.19.1
Spinal Roots C3, C4, & C5
2.19.1.1
.
2.19.2
Cutaneous Branches
2.19.2.1
None
2.19.3
Sensory Branches
2.19.3.1
The anterior, anterolateral and posterior branches supply
Proprioceptive endings in the diaphragm, parietal peritoneum of the diaphragm,
and diaphragmatic pleura related to the central tendon and musculature.
2.19.4
Muscular Branches-To the Diaphragm divided into three branches
2.19.4.1 A=Anterior (sternal) branches
2.19.4.1.1
Supply
the muscular fibers anterior to the central tendon.
2.19.4.2 B=Anterolateral branches
2.19.4.2.1
Supply
the muscular fibers anterior to the lateral leaf of the central tendon
2.19.4.3 C=Posterior branches
2.19.4.3.1
Supply
the muscular fibers posterior to the central tendon, including the crural
fibers.
2.19.5
Articular Branches
2.19.5.1
None
2.19.6
Lesions
2.19.6.1
Complete section of the phrenic nerve will produce paralysis
and atrophy of corresponding part of the diaphragm. Unilateral lesion: few or
no symptoms may be exhibited. Bilateral lesion: usually from damage to the
cervical spinal cords. Presents as severe dyspnea (difficult or laboured
respiration-shortness of breath) upon slightest exertion, over activity of
accessory respiratory muscles, difficulty in coughing and sneezing and atrophy
of diaphragm. If an accessory phrenic nerve exists and escapes damage the
paralysis will be incomplete.
2.19.7
Note
2.19.7.1
An accessory phrenic nerve would branch from the nerve to
the subclavius or ansa cervicalis.
2.19.8
Path Description
2.19.8.1
The Phrenic Nerve (n. phrenicus; internal respiratory nerve
of Bell) contains motor and sensory fibers in the proportion of about two to
one. It arises chiefly from the fourth cervical nerve, but receives a branch
from the third and another from the fifth; (the fibers from the fifth
occasionally come through the nerve to the Subclavius.) It descends to the root
of the neck, running obliquely across the front of the Scalenus anterior, and
beneath the Sternocleidomastoideus, the inferior belly of the Omohyoideus, and
the transverse cervical and transverse scapular vessels. It next passes in
front of the first part of the subclavian artery, between it and the subclavian
vein, and, as it enters the thorax, crosses the internal mammary artery near
its origin. Within the thorax, it descends nearly vertically in front of the
root of the lung, and then between the pericardium and the mediastinal pleura,
to the diaphragm, where it divides into branches, which pierce that muscle, and
are distributed to its under surface. In the thorax it is accompanied by the
pericardiacophrenic branch of the internal mammary artery.
2.19.8.2
The two phrenic
nerves differ in their length, and also in their relations at the upper part of
the thorax. 22
2.19.8.3
The right nerve is
situated more deeply, and is shorter and more vertical in direction than the
left; it lies lateral to the right innominate vein and superior vena cava. 23
2.19.8.4
The left nerve is
rather longer than the right, from the inclination of the heart to the left
side, and from the diaphragm being lower on this than on the right side. At the
root of the neck it is crossed by the thoracic duct; in the superior
mediastinal cavity it lies between the left common carotid and left subclavian
arteries, and crosses superficial to the vagus on the left side of the arch of
the aorta.
2.19.8.1
Each nerve supplies filaments to the pericardium
and pleura, and
at the root of the neck is joined by a filament from the sympathetic, and,
occasionally, by one from the ansa hypoglossi. Branches have been described as
passing to the peritoneum.
2.19.8.2
From the right
nerve, one or two filaments pass to join in a small phrenic ganglion with
phrenic branches of the celiac plexus; and branches from this ganglion are
distributed to the falciform and coronary ligaments of the liver, the
suprarenal gland, inferior vena cava, and right atrium. From the left nerve,
filaments pass to join the phrenic branches of the celiac plexus, but without
any ganglionic enlargement; and a twig is distributed to the left adrenal
gland (suprarenal gland).
2.19.8.3
The phrenic nerve arises from the
third, fourth, and fifth cervical spinal nerves (C3-C5). It provides motor innervation to the diaphragm and is thus responsible for
the act of breathing. In addition, it provides sensory innervation for many
components of the mediastinum and pleura,
as well as the upper abdomen, especially the liver
and gall bladder. Pain arising from structures served by the phrenic
nerve is often "referred" to other somatic regions served by spinal
nerves C3-C5. For instance, angina pectoris classically is felt both in
the chest and in the left arm. Likewise, a liver abscess close to the diaphragm
will be felt in the right shoulder.
2.19.8.4
Both phrenic nerves run from C3, C4 and C5 along the anterior scalene muscle deep to the carotid sheath. The right phrenic nerve passes over the right brachiocephalic artery, the subclavian vein, and the superior vena cava and then crosses the
root of the right lung and then leaves the thorax
by passing through the vena cava hiatus opening in the diaphragm at the level
of T10. The right phrenic nerve passes over the right atrium. The left phrenic
nerve passes over the left ventricle and pierces the diaphragm separately.
2.19.8.5
Both these nerves supply motor fibres to the diaphragm and
sensory fibres to the fibrous pericardium, mediastinal pleura and diaphragmatic peritoneum.
2.19.8.6
Irritation of the phrenic nerve leads to the Hiccup Reflex,
which is due to spasms of the diaphram pushing air that hits the closed folds
of the glottis.
2.19.1
Functional Anatomy
2.19.1.1
The Phrenic Nerve contains twice as many motor nerve fibers
as sensory fibers. The Phrenic Nerve arises mostly from fourth cervical nerve
(C4), but receives a branch from the third (C3) and another from the fifth
(C5). The phrenic nerve http://en.wikipedia.org/wiki/Phrenic_nerve
forms
from both the cervical http://www.bartleby.com/107/illus804.html
and Brachial Plexus http://www.bartleby.com/107/illus807.html. The motor fibers send nerve impulses from the
brain (efferent) to the diaphragm muscle, which then tightens. When the
diaphragm muscle contracts it increases the volume of the cavity in which the
lungs are contained. This expands the lungs and allows you to take a deep
breath, cough, or sneeze. If the phrenic nerve is completely cut (Complete
section) it becomes very difficult to breathe (Dyspnea (difficult or laboured
respiration)). The afferent sensory fibers of the Phrenic Nerve
send impulses to the spinal cord from the following structures; to the hearts pericardium and
pleura of the lungs, Mediastinum (non-delineated group of structures in the
thorax (chest)), inferior vena cava, and right atrium, peritoneum (smooth
transparent serous membrane that lines the cavity of the abdomen), falciform
and coronary ligaments of the liver, and adrenal gland (suprarenal gland). Some
references indicate phrenic sensory
nerve connections to the gall bladder (although one references
mentions=no specifics are given http://en.wikipedia.org/wiki/Phrenic_nerve), capsule of the
liver, and pancreas (As he stated in his article). I will then assume that
these do not exist until otherwise informed. The phrenic nerve sensory fibers
will refer pain from the aforementioned structures it supplies to other somatic
regions also supplied by the nerve roots that form the phrenic nerve (C3-5).
Dermatomal, sclerotomal and or proprioceptive pain referral is possible. For
example heart disease (angina pectoris) may be felt in the chest and or down
the left arm. Liver or Gall bladder problems near the diaphragm may be felt in
the right shoulder. Pain in the shoulder or down the arm from irritated
visceral structures does not constitute prima facie evidence for phrenic nerve
transmission of psychological stress nor does it necessarily imply a role in
more complex Orthopedic, muscular and or skeletal problems.
2.19.2
Theory WARNING LABEL; I am not a neurologist and THIS IS A
THEORY. When I’m not sure about something I will mark it with a (?=not sure)
2.19.2.1
The sensory fibers of the phrenic nerve supply structures,
which are related to increased exertion e.g. the heart, membranes in the chest
(Mediastinum), abdominal membranes attached to the diaphragm (?), ligaments which
are attached to the diaphragm (?), and endocrine glands, which give us the
energy for exertion. The phrenic nerve forms a reflex arc with its motor nerves
in the spinal cord (?). It does not need to be connected to the higher brain to
function properly and therefore does not serve as a conduit to disperse the
stress of negative thinking. The primary function of the phrenic nerves
Proprioceptive sensory fibers is to tell its motor nerves when we are exerting
ourselves; running walking fighting ect so as to give more juice to the
diaphragm (to increase O2 delivery). If the heart is pumping away because we
are on the last 100 yards of a killer marathon this feedback loop is just what
the doctor ordered. Its very much like an automatic pilot that instantly
without your conscious thought initiates a reflex arc with the motor fibers in
the spinal cord (?) to increase contraction of the diaphragm muscle during
heavy exertion. The function of the phrenic nerve as primarily a motor nerve is
evident in its neuroanatomy with twice as many motor fibers as sensory fibers.
None of its motor or sensory fibers are connected with rotator cuff, capsule of
the shoulder, ligaments or muscles of the neck ect. Because the phrenic nerve
forms from the cervical and brachial plexus (A plexus looks like macramé done
by someone with severe ADHD) and I am not intimately familiar with the
neuroanatomy of these structures so it is not clear to me if some connection
exists to the accessory nerve (Cranial Nerve). I will assume there is no
connection until otherwise informed. Therefore there is no mind body connection
with the phrenic nerve serving as a conduit displacing psychological stress.
Further because the motor portion of the phrenic doesn’t innervate any of the
sacs and tubes mentioned by Dr Alexander in his article [1] there
can be no cringing of sacs & shortening of tubes. The motor portion of the
phrenic nerve only innervates to the diaphragm muscle at least according to all
of the anatomical books I’ve looked at. I realize it feels that way when you
are anxious. Perhaps there are other explanations but the phrenic circuit is
not one of them. Perhaps though there are other connections, which I do not
have the neuroanatomical knowledge to explore. I believe (?) the shoulder joint
capsule both its tendons and perhaps connective tissue are innervated
dermatomally, sclerotomally (area of bone innervated by a single spinal
segment), and perhaps proprioceptivly (sensory nerves embedded with connective
tissue/muscle to provide joint positional information) by the C5 nerve. I don’t
think this should affect the simple reflex arc between the motor and sensory
fibers of the phrenic nerve whose primary purpose is to increase contraction of
the diaphragm during heavy exertion. I will assume it does not unless otherwise
informed.
2.19.3
Hypothesis
2.19.3.1
Complete section of the sensory fibers of the phrenic nerve
will significantly decrease aerobic capacity during heavy exertion.
2.19.4
Literature Review
2.19.4.1
I’m thinking a literature review rather than an experiment
simply because nobody I know would raise their hand to volunteer to have the
sensory fibers of their phrenic nerve cut. I am quite sure no one would
volunteer his or her pet hamster, dog, or cat for this experiment either. So a
review of the scientific literature is in order to determine the aerobic
capacity of people or animals that have a damaged phrenic sensory nerve.
2.19.5
Gray’s Anatomy and other references
2.19.5.1
Discussion
2.19.5.1.1
Cervical
Nerves
2.19.5.1.1.1
http://www.bartleby.com/107/210.html
2.19.5.1.2
Brachial
Plexus
2.19.5.1.2.1
http://www.bartleby.com/107/210.html#i807
2.19.5.1.3
Diaphragm
2.19.5.1.3.1
http://www.bartleby.com/107/illus391.html
2.19.5.1.3.2
Diaphragm
2.19.5.2
Illustrations
2.19.5.2.1
Thoracic
Cavity (or chest cavity)
2.19.5.2.1.1
http://www.bartleby.com/107/illus806.html
2.19.5.2.2
Cervical
Plexus
2.19.5.2.2.1
http://www.bartleby.com/107/illus804.html
2.19.5.2.3
Brachial
Plexus
2.19.5.2.3.1
http://www.bartleby.com/107/illus807.html
2.19.5.2.4
Vagus
Nerve
2.19.5.2.4.1
http://www.bartleby.com/107/205.html
2.19.5.2.5
Sympathetic
Nervous System
2.19.5.2.5.1
http://www.bartleby.com/107/214.html
2.19.5.2.6
Diaphragm
2.19.5.2.6.1
http://www.bartleby.com/107/illus391.html
2.19.6
Number
2.19.6.1
32.05
2.19.7
Reference
2.19.7.1
19
2.19.8
Illustration
2.19.8.1 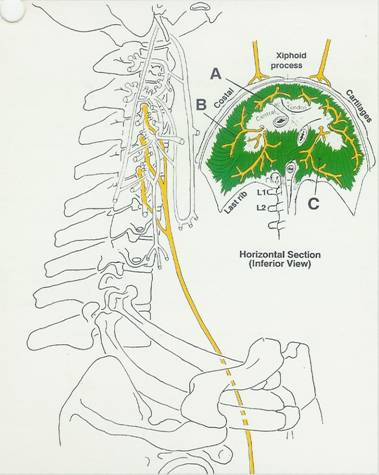
2.1 RECTUS CAPITIS
LATERALIS N.
Back
Table of Contents References
2.1.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
2.1.1.1
.
2.1.2 NUMBER
2.1.2.1
35
2.1.3 REFERENCE
2.1.3.1
2.1.4 ROOTS
2.1.4.1
2.1.4.2
Lumbar Plexus
2.1.4.3
VENTRAL
2.1.5 DIVISION
2.1.5.1
Dorsal Ventral
2.1.5.2
2.1.6 CUTANEOUS BRANCHES
2.1.6.1
2.1.6.1.1
2.1.6.2
2.1.6.2.1
.
2.1.7 ARTICULAR BRANCHES
2.1.7.1
2.1.7.1.1
2.1.8 MUSCULAR BRANCHES
2.1.8.1
2.1.8.2
2.1.8.3
2.1.8.4
2.1.8.5
2.1.8.6
2.2 RECTUS CAPITIS
ANTERIOR N.
Back
Table of Contents References
2.2.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
2.2.1.1
.
2.2.2 NUMBER
2.2.2.1
35
2.2.3 REFERENCE
2.2.3.1
2.2.4 ROOTS
2.2.4.1
2.2.4.2
Lumbar Plexus
2.2.4.3
VENTRAL
2.2.5 DIVISION
2.2.5.1
Dorsal Ventral
2.2.5.2
2.2.6 CUTANEOUS BRANCHES
2.2.6.1
2.2.6.1.1
2.2.6.2
2.2.6.2.1
.
2.2.7 ARTICULAR BRANCHES
2.2.7.1
2.2.7.1.1
2.2.8 MUSCULAR BRANCHES
2.2.8.1
2.2.8.2
2.2.8.3
2.2.8.4
2.2.8.5
2.2.8.6
2.3 LONGUS CAPITIS N
Back
Table of Contents References
2.3.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
2.3.1.1
.
2.3.2 NUMBER
2.3.2.1
35
2.3.3 REFERENCE
2.3.3.1
2.3.4 ROOTS
2.3.4.1
2.3.4.2
Lumbar Plexus
2.3.4.3
VENTRAL
2.3.5 DIVISION
2.3.5.1
Dorsal Ventral
2.3.5.2
2.3.6 CUTANEOUS BRANCHES
2.3.6.1
2.3.6.1.1
2.3.6.2
2.3.6.2.1
.
2.3.7 ARTICULAR BRANCHES
2.3.7.1
2.3.7.1.1
2.3.8 MUSCULAR BRANCHES
2.3.8.1
2.3.8.2
2.3.8.3
2.3.8.4
2.3.8.5
2.3.8.6
2.4 LONGUS COLI N.
Back
Table of Contents References
2.4.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
2.4.1.1
.
2.4.2 NUMBER
2.4.2.1
35
2.4.3 REFERENCE
2.4.3.1
2.4.4 ROOTS
2.4.4.1
2.4.4.2
Lumbar Plexus
2.4.4.3
VENTRAL
2.4.5 DIVISION
2.4.5.1
Dorsal Ventral
2.4.5.2
2.4.6 CUTANEOUS BRANCHES
2.4.6.1
2.4.6.1.1
2.4.6.2
2.4.6.2.1
.
2.4.7 ARTICULAR BRANCHES
2.4.7.1
2.4.7.1.1
2.4.8 MUSCULAR BRANCHES
2.4.8.1
2.4.8.2
2.4.8.3
2.4.8.4
2.4.8.5
2.4.8.6
2.5 STERNOCLEIDOMASTOID
N.
Back
Table of Contents References
2.5.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
2.5.1.1
.
2.5.2 NUMBER
2.5.2.1
35
2.5.3 REFERENCE
2.5.3.1
2.5.4 ROOTS
2.5.4.1
2.5.4.2
Lumbar Plexus
2.5.4.3
VENTRAL
2.5.5 DIVISION
2.5.5.1
Dorsal Ventral
2.5.5.2
2.5.6 CUTANEOUS BRANCHES
2.5.6.1
2.5.6.1.1
2.5.6.2
2.5.6.2.1
.
2.5.7 ARTICULAR BRANCHES
2.5.7.1
2.5.7.1.1
2.5.8 MUSCULAR BRANCHES
2.5.8.1
2.5.8.2
2.5.8.3
2.5.8.4
2.5.8.5
2.5.8.6
2.6 TRAPEZIUS N.
Back
Table of Contents References
2.6.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
2.6.1.1
.
2.6.2 NUMBER
2.6.2.1
35
2.6.3 REFERENCE
2.6.3.1
2.6.4 ROOTS
2.6.4.1
2.6.4.2
Lumbar Plexus
2.6.4.3
VENTRAL
2.6.5 DIVISION
2.6.5.1
Dorsal Ventral
2.6.5.2
2.6.6 CUTANEOUS BRANCHES
2.6.6.1
2.6.6.1.1
2.6.6.2
2.6.6.2.1
.
2.6.7 ARTICULAR BRANCHES
2.6.7.1
2.6.7.1.1
2.6.8 MUSCULAR BRANCHES
2.6.8.1
2.6.8.2
2.6.8.3
2.6.8.4
2.6.8.5
2.6.8.6
2.7 LEVATOR SCAPULAE
N.
Back
Table of Contents References
2.7.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
2.7.1.1
.
2.7.2 NUMBER
2.7.2.1
35
2.7.3 REFERENCE
2.7.3.1
2.7.4 ROOTS
2.7.4.1
2.7.4.2
Lumbar Plexus
2.7.4.3
VENTRAL
2.7.5 DIVISION
2.7.5.1
Dorsal Ventral
2.7.5.2
2.7.6 CUTANEOUS BRANCHES
2.7.6.1
2.7.6.1.1
2.7.6.2
2.7.6.2.1
.
2.7.7 ARTICULAR BRANCHES
2.7.7.1
2.7.7.1.1
2.7.8 MUSCULAR BRANCHES
2.7.8.1
2.7.8.2
2.7.8.3
2.7.8.4
2.7.8.5
2.7.8.6
2.8 SCALENUS NERVES.
Back
Table of Contents References
2.8.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
2.8.1.1
.
2.8.2 NUMBER
2.8.2.1
35
2.8.3 REFERENCE
2.8.3.1
2.8.4 ROOTS
2.8.4.1
2.8.4.2
Lumbar Plexus
2.8.4.3
VENTRAL
2.8.5 DIVISION
2.8.5.1
Dorsal Ventral
2.8.5.2
2.8.6 CUTANEOUS BRANCHES
2.8.6.1
2.8.6.1.1
2.8.6.2
2.8.6.2.1
.
2.8.7 ARTICULAR BRANCHES
2.8.7.1
2.8.7.1.1
2.8.8 MUSCULAR BRANCHES
2.8.8.1
2.8.8.2
2.8.8.3
2.8.8.4
2.8.8.5
2.8.8.6
2.9 BRACHIAL PLEXUS
Back
Table of Contents References
2.9.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
2.9.1.1
.
2.9.2 NUMBER
2.9.2.1
35
2.9.3 REFERENCE
2.9.3.1
2.9.4 ROOTS
2.9.4.1
2.9.4.2
Lumbar Plexus
2.9.4.3
VENTRAL
2.9.5 DIVISION
2.9.5.1
Dorsal Ventral
2.9.5.2
2.9.6 CUTANEOUS BRANCHES
2.9.6.1
2.9.6.1.1
2.9.6.2
2.9.6.2.1
.
2.9.7 ARTICULAR BRANCHES
2.9.7.1
2.9.7.1.1
2.9.8 MUSCULAR BRANCHES
2.9.8.1
2.9.8.2
2.9.8.3
2.9.8.4
2.9.8.5
2.9.8.6
2.10 DORSAL SCAPULAR N.
Back
Table of Contents References
2.10.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
2.10.1.1
.
2.10.2
NUMBER
2.10.2.1
35
2.10.3
REFERENCE
2.10.3.1
2.10.4
ROOTS
2.10.4.1
2.10.4.2
Lumbar Plexus
2.10.4.3
VENTRAL
2.10.5
DIVISION
2.10.5.1
Dorsal Ventral
2.10.5.2
2.10.6
CUTANEOUS BRANCHES
2.10.6.1
2.10.6.1.1
2.10.6.2
2.10.6.2.1
.
2.10.7
ARTICULAR BRANCHES
2.10.7.1
2.10.7.1.1
2.10.8
MUSCULAR BRANCHES
2.10.8.1
2.10.8.2
2.10.8.3
2.10.8.4
2.10.8.5
2.10.8.6
2.11 LONG THORACIC
NERVE
Back
Table of Contents References
2.11.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
2.11.1.1
.
2.11.2
NUMBER
2.11.2.1
35
2.11.3
REFERENCE
2.11.3.1
2.11.4
ROOTS
2.11.4.1
2.11.4.2
Lumbar Plexus
2.11.4.3
VENTRAL
2.11.5
DIVISION
2.11.5.1
Dorsal Ventral
2.11.5.2
2.11.6
CUTANEOUS BRANCHES
2.11.6.1
2.11.6.1.1
2.11.6.2
2.11.6.2.1
.
2.11.7
ARTICULAR BRANCHES
2.11.7.1
2.11.7.1.1
2.11.8
MUSCULAR BRANCHES
2.11.8.1
2.11.8.2
2.11.8.3
2.11.8.4
2.11.8.5
2.11.8.6
2.12 SUBCLAVIUS N.
Back
Table of Contents References
2.12.1
DESCRIPTION: PATH, FUNCTION,
LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
2.12.1.1
.
2.12.2
NUMBER
2.12.2.1
35
2.12.3
REFERENCE
2.12.3.1
2.12.4
ROOTS
2.12.4.1
2.12.4.2
Lumbar Plexus
2.12.4.3
VENTRAL
2.12.5
DIVISION
2.12.5.1
Dorsal Ventral
2.12.5.2
2.12.6
CUTANEOUS BRANCHES
2.12.6.1
2.12.6.1.1
2.12.6.2
2.12.6.2.1
.
2.12.7
ARTICULAR BRANCHES
2.12.7.1
2.12.7.1.1
2.12.8
MUSCULAR BRANCHES
2.12.8.1
2.12.8.2
2.12.8.3
2.12.8.4
2.12.8.5
2.12.8.6
2.13 UPPER SUBSCAPULAR
N.
Back
Table of Contents References
2.13.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
2.13.1.1
.
2.13.2
NUMBER
2.13.2.1
35
2.13.3
REFERENCE
2.13.3.1
2.13.4
ROOTS
2.13.4.1
2.13.4.2
Lumbar Plexus
2.13.4.3
VENTRAL
2.13.5
DIVISION
2.13.5.1
Dorsal Ventral
2.13.5.2
2.13.6
CUTANEOUS BRANCHES
2.13.6.1
2.13.6.1.1
2.13.6.2
2.13.6.2.1
.
2.13.7
ARTICULAR BRANCHES
2.13.7.1
2.13.7.1.1
2.13.8
MUSCULAR BRANCHES
2.13.8.1
2.13.8.2
2.13.8.3
2.13.8.4
2.13.8.5
2.13.8.6
2.14 THORACODORSAL N.
(MIDDLE SUBSCAPULAR N.)
Back
Table of Contents References
2.14.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
2.14.1.1
.
2.14.2
NUMBER
2.14.2.1
35
2.14.3
REFERENCE
2.14.3.1
2.14.4
ROOTS
2.14.4.1
2.14.4.2
Lumbar Plexus
2.14.4.3
VENTRAL
2.14.5
DIVISION
2.14.5.1
Dorsal Ventral
2.14.5.2
2.14.6
CUTANEOUS BRANCHES
2.14.6.1
2.14.6.1.1
2.14.6.2
2.14.6.2.1
.
2.14.7
ARTICULAR BRANCHES
2.14.7.1
2.14.7.1.1
2.14.8
MUSCULAR BRANCHES
2.14.8.1
2.14.8.2
2.14.8.3
2.14.8.4
2.14.8.5
2.14.8.6
2.15 LOWER SUBSCAPULAR
N.
Back
Table of Contents References
2.15.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
2.15.1.1
.
2.15.2
NUMBER
2.15.2.1
35
2.15.3
REFERENCE
2.15.3.1
2.15.4
ROOTS
2.15.4.1
2.15.4.2
Lumbar Plexus
2.15.4.3
VENTRAL
2.15.5
DIVISION
2.15.5.1
Dorsal Ventral
2.15.5.2
2.15.6
CUTANEOUS BRANCHES
2.15.6.1
2.15.6.1.1
2.15.6.2
2.15.6.2.1
.
2.15.7
ARTICULAR BRANCHES
2.15.7.1
2.15.7.1.1
2.15.8
MUSCULAR BRANCHES
2.15.8.1
2.15.8.2
2.15.8.3
2.15.8.4
2.15.8.5
2.15.8.6
1 Arms
1.1 SUPRACLAVICULAR
Back
Table of Contents References
1.1.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
1.1.1.1
.
1.1.2 NUMBER
1.1.2.1
35
1.1.3 REFERENCE
1.1.3.1
1.1.4 ROOTS
1.1.4.1
1.1.4.2
Lumbar Plexus
1.1.4.3
VENTRAL
1.1.5 DIVISION
1.1.5.1
Dorsal Ventral
1.1.5.2
1.1.6 CUTANEOUS BRANCHES
1.1.6.1
1.1.6.1.1
1.1.6.2
1.1.6.2.1
.
1.1.7 ARTICULAR BRANCHES
1.1.7.1
1.1.7.1.1
1.1.8 MUSCULAR BRANCHES
1.1.8.1
1.1.8.2
1.1.8.3
1.1.8.4
1.1.8.5
1.1.8.6
1.2 AXILLARY (U LAT
CUT N)
Back
Table of Contents References
1.2.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
1.2.1.1
.
1.2.2 NUMBER
1.2.2.1
35
1.2.3 REFERENCE
1.2.3.1
1.2.4 ROOTS
1.2.4.1
1.2.4.2
Lumbar Plexus
1.2.4.3
VENTRAL
1.2.5 DIVISION
1.2.5.1
Dorsal Ventral
1.2.5.2
1.2.6 CUTANEOUS BRANCHES
1.2.6.1
1.2.6.1.1
1.2.6.2
1.2.6.2.1
.
1.2.7 ARTICULAR BRANCHES
1.2.7.1
1.2.7.1.1
1.2.8 MUSCULAR BRANCHES
1.2.8.1
1.2.8.2
1.2.8.3
1.2.8.4
1.2.8.5
1.2.8.6
1.3 2ND THOR INTERCSL
N
Back
Table of Contents References
1.3.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
1.3.1.1
.
1.3.2 NUMBER
1.3.2.1
35
1.3.3 REFERENCE
1.3.3.1
1.3.4 ROOTS
1.3.4.1
1.3.4.2
Lumbar Plexus
1.3.4.3
VENTRAL
1.3.5 DIVISION
1.3.5.1
Dorsal Ventral
1.3.5.2
1.3.6 CUTANEOUS BRANCHES
1.3.6.1
1.3.6.1.1
1.3.6.2
1.3.6.2.1
.
1.3.7 ARTICULAR BRANCHES
1.3.7.1
1.3.7.1.1
1.3.8 MUSCULAR BRANCHES
1.3.8.1
1.3.8.2
1.3.8.3
1.3.8.4
1.3.8.5
1.3.8.6
1.4 MEDIAL BRACHIAL
CUT N.(FLASH;MEDIAL CUT)(GRAY;LESSER INTERNAL CUT,N. OF WRISBERG)
Back
Table of Contents References
1.4.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
1.4.1.1
.
1.4.2 NUMBER
1.4.2.1
35
1.4.3 REFERENCE
1.4.3.1
1.4.4 ROOTS
1.4.4.1
1.4.4.2
Lumbar Plexus
1.4.4.3
VENTRAL
1.4.5 DIVISION
1.4.5.1
Dorsal Ventral
1.4.5.2
1.4.6 CUTANEOUS BRANCHES
1.4.6.1
1.4.6.1.1
1.4.6.2
1.4.6.2.1
.
1.4.7 ARTICULAR BRANCHES
1.4.7.1
1.4.7.1.1
1.4.8 MUSCULAR BRANCHES
1.4.8.1
1.4.8.2
1.4.8.3
1.4.8.4
1.4.8.5
1.4.8.6
1.5 RADIAL
Back
Table of Contents References
1.5.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
1.5.1.1
.
1.5.2 NUMBER
1.5.2.1
35
1.5.3 REFERENCE
1.5.3.1
1.5.4 ROOTS
1.5.4.1
1.5.4.2
Lumbar Plexus
1.5.4.3
VENTRAL
1.5.5 DIVISION
1.5.5.1
Dorsal Ventral
1.5.5.2
1.5.6 CUTANEOUS BRANCHES
1.5.6.1
1.5.6.1.1
1.5.6.2
1.5.6.2.1
.
1.5.7 ARTICULAR BRANCHES
1.5.7.1
1.5.7.1.1
1.5.8 MUSCULAR BRANCHES
1.5.8.1
1.5.8.2
1.5.8.3
1.5.8.4
1.5.8.5
1.5.8.6
1.6 MUSCULOCUTANEOUS
Back
Table of Contents References
1.6.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
1.6.1.1
.
1.6.2 NUMBER
1.6.2.1
35
1.6.3 REFERENCE
1.6.3.1
1.6.4 ROOTS
1.6.4.1
1.6.4.2
Lumbar Plexus
1.6.4.3
VENTRAL
1.6.5 DIVISION
1.6.5.1
Dorsal Ventral
1.6.5.2
1.6.6 CUTANEOUS BRANCHES
1.6.6.1
1.6.6.1.1
1.6.6.2
1.6.6.2.1
.
1.6.7 ARTICULAR BRANCHES
1.6.7.1
1.6.7.1.1
1.6.8 MUSCULAR BRANCHES
1.6.8.1
1.6.8.2
1.6.8.3
1.6.8.4
1.6.8.5
1.6.8.6
1.7 MED ANTEBRACHIAL
CUT N.(FLASH;MEDIAL CUTANEOUS N. OF
FOREARM),(GRAY; INTERNAL CUT N.)
Back
Table of Contents References
1.7.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
1.7.1.1
.
1.7.2 NUMBER
1.7.2.1
35
1.7.3 REFERENCE
1.7.3.1
1.7.4 ROOTS
1.7.4.1
1.7.4.2
Lumbar Plexus
1.7.4.3
VENTRAL
1.7.5 DIVISION
1.7.5.1
Dorsal Ventral
1.7.5.2
1.7.6 CUTANEOUS BRANCHES
1.7.6.1
1.7.6.1.1
1.7.6.2
1.7.6.2.1
.
1.7.7 ARTICULAR BRANCHES
1.7.7.1
1.7.7.1.1
1.7.8 MUSCULAR BRANCHES
1.7.8.1
1.7.8.2
1.7.8.3
1.7.8.4
1.7.8.5
1.7.8.6
2 Hands
2.1 ULNAR
Back
Table of Contents References
2.1.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
2.1.1.1
.
2.1.2 NUMBER
2.1.2.1
35
2.1.3 REFERENCE
2.1.3.1
2.1.4 ROOTS
2.1.4.1
2.1.4.2
Lumbar Plexus
2.1.4.3
VENTRAL
2.1.5 DIVISION
2.1.5.1
Dorsal Ventral
2.1.5.2
2.1.6 CUTANEOUS BRANCHES
2.1.6.1
2.1.6.1.1
2.1.6.2
2.1.6.2.1
.
2.1.7 ARTICULAR BRANCHES
2.1.7.1
2.1.7.1.1
2.1.8 MUSCULAR BRANCHES
2.1.8.1
2.1.8.2
2.1.8.3
2.1.8.4
2.1.8.5
2.1.8.6
2.2 RADIAL
Back
Table of Contents References
2.2.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
2.2.1.1
.
2.2.2 NUMBER
2.2.2.1
35
2.2.3 REFERENCE
2.2.3.1
2.2.4 ROOTS
2.2.4.1
2.2.4.2
Lumbar Plexus
2.2.4.3
VENTRAL
2.2.5 DIVISION
2.2.5.1
Dorsal Ventral
2.2.5.2
2.2.6 CUTANEOUS BRANCHES
2.2.6.1
2.2.6.1.1
2.2.6.2
2.2.6.2.1
.
2.2.7 ARTICULAR BRANCHES
2.2.7.1
2.2.7.1.1
2.2.8 MUSCULAR BRANCHES
2.2.8.1
2.2.8.2
2.2.8.3
2.2.8.4
2.2.8.5
2.2.8.6
2.3 MEDIAN NERVE
Back
Table of Contents References
2.3.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
2.3.1.1
.
2.3.2 NUMBER
2.3.2.1
35
2.3.3 REFERENCE
2.3.3.1
2.3.4 ROOTS
2.3.4.1
2.3.4.2
Lumbar Plexus
2.3.4.3
VENTRAL
2.3.5 DIVISION
2.3.5.1
Dorsal Ventral
2.3.5.2
2.3.6 CUTANEOUS BRANCHES
2.3.6.1
2.3.6.1.1
2.3.6.2
2.3.6.2.1
.
2.3.7 ARTICULAR BRANCHES
2.3.7.1
2.3.7.1.1
2.3.8 MUSCULAR BRANCHES
2.3.8.1
2.3.8.2
2.3.8.3
2.3.8.4
2.3.8.5
2.3.8.6
2.4
2.5
3 HIP AND LEGS
3.1 12TH THORACIC
INTERCOSTAL (SUB COSTAL) 35.01
Back
Table of Contents References
3.1.1 DESCRIPTION # 1:
PATH, FUNCTION-LESIONS
3.1.1.1
A FOCAL LESION TO THE SUBCOSTAL NERVE WOULD NOT
SIGNIFICANTLY WEAKEN THE QUADRATUS LUMBORUM BUT WOULD PARALYZE THE PYRAMIDALIS
AND WEAKEN THE LOWER ABDOMINAL MUSCLES PRESENTING "BEAVOR'S SIGN".
THIS COULD ALSO PRESENT A BULGING OF THE LOWER ABDOMEN.
3.1.2 DESCRIPTION # 2:
CUTANEOUS AREA, ADDITIONAL COMMENTS
3.1.2.1
T12 IS OFTEN CONSIDERED PART OF THE LUMBAR PLEXUS.
3.1.3 CUTANEOUS BRANCHES
(12TH THOR)
3.1.3.1
LATERAL CUTANEOUS (CUT B) 35.011
3.1.3.1.1
ANTEROLATERAL
GLUTEAL SKIN SOME FILAMENTS REACHING THE SKIN OVER THE GREATER TROCHANTER
3.1.3.2
ANTERIOR CUTANEOUS(CUT BR) 35.012
3.1.3.2.1
SKIN
OF SUPRAPUBIC AREA.
3.1.4 Articular Branches
3.1.4.1
ARTICULAR(12 THOR)
3.1.4.1.1
12TH
COSTOVERTEBRAL(ART)
3.1.5 ROOTS
3.1.5.1
T12
3.1.5.2
SPINAL NERVE
3.1.5.3
VENTRAL
3.1.6 MUSCULAR BRANCHES
(12TH THORACIC)
3.1.6.1 QUADRATUS
LUMBORUM T12-L3,(L4)
3.1.6.2 TRANSVERSE
ABDOMINAL T7-L1
3.1.6.3 INTERNAL OBLIQUE
ABDOMINAL T7-L1
3.1.6.4 EXTERNAL OBLIQUE
ABDOMINAL T5-T12
3.1.6.4.1
T12
LATERAL CUTANEOUS BRANCH SUPPLIES THE LOWER SLIP
3.1.6.5 RECTUS ABDOMINAL
(T5),T6-T12
3.1.6.6 PYRAMIDALIS T12
3.1.7 NUMBER
3.1.7.1
35.01
3.1.8 REFERANCE
3.1.8.1
50
3.2 Lumbar Plexus
(Spinal Segments & Nerves) (61)
3.2.1 Spinal Segments
3.2.1.1
3.2.2 Nerves
3.2.2.1
3.2.3 Reference
3.2.3.1
61
3.3 Lumbar Plexus (62)
Back
Table of Contents References
3.3.1 Spinal Roots
3.3.1.1
L 1, L2, L3, L4 ventral rami with a
ramus from T12
3.3.1.1.1
They descend laterally into the psoas
major. The first three and most of the fourth form the lumbar plexus. The rest
of L4 splits to join L5 forming the Lumbosacral trunk
3.3.2 Named Branches
3.3.2.1 A=Muscular branches / T12,
L 1-L4.
3.3.2.2 B=Iliohypogastric
nerve /
T12, L 1.
3.3.2.3 C=llio-inguinal
nerve / L 1.
3.3.2.4
D=Genitofemoral
nerve /
L 1, L2.
3.3.3 From Ventral
Divisions
3.3.3.1 E=Obturator nerve / L2-L4.
3.3.3.2
F=Accessory
Obturator nerve / L3,
L4
3.3.4 From Dorsal
Divisions
3.3.4.1 G=Lateral femoral cutaneous nerve / L4,
L5.
3.3.4.2 H=Femoral nerve / L2-L4.
3.3.4.3
I=Lumbosacral
trunk to sacral plexus / L4, L5.
3.3.5 Cutaneous Branches
3.3.5.1
The areas of cutaneous innervation
are designated by the letters as described above
3.3.6 Lesions
3.3.6.1
Injury to the lumbar roots or the
cauda equina related to L 1, L2, L3 can result from neurofibromas, meningiomas
or other malignant disease. Disc herniations, although less common, can produce
focal lesions of the lumbar roots. Injury
to L1 results in weakness of abdominal musculature and
paresthesias to the skin region of the greater trochanter and upper groin. Injury to L2
produces weak hip flexion, due to deficits in psoas major and iliacus, and
paresthesias to skin of anterior thigh. Injury to L3 results in weak adduction of
leg and reduced knee jerk reflex and paresthesias to skin of anterior thigh
(femoral nerve), anteromedial knee, leg and foot (saphenous nerve). Injury to L4 is
the most common lesion of the lumbar plexus and typically results from a
herniated intervertebral disc between L4 and L5 or degenerative arthritis
(spondylosis) in the spine. Deficits resemble those of L3 except that cutaneous
fibers for the anterior thigh (via the femoral nerve) survive. Deficits to
tibialis anterior and posterior will result in a "foot drop" via L4
lumbosacral trunk deficit.
3.3.7 Path Description
3.3.7.1
The lumbar plexus is formed by the loops of communication
between the anterior divisions of the first three and the greater part of the
fourth lumbar nerves; the first lumbar often receives a branch from the last
thoracic nerve. It is situated in the posterior part of the Psoas major, in front
of the transverse processes of the lumbar vertebra. The mode in which the
plexus is arranged varies in different subjects. It differs from the brachial
plexus in not forming an intricate interlacement, but the several nerves of
distribution arise from one or more of the spinal nerves, in the
following manner: the first lumbar nerve, frequently supplemented by a twig
from the last thoracic, splits into an upper and lower branch; the upper and
larger branch divides into the Iliohypogastric and ilioinguinal nerves; the
lower and smaller branch unites with a branch of the second lumbar to form the
Genitofemoral nerve. The remainder of the second nerve, and the third and
fourth nerves, divide into ventral and dorsal divisions. The ventral division
of the second unites with the ventral divisions of the third and fourth nerves
to form the Obturator nerve. The dorsal divisions of the second and third
nerves divide into two branches, a smaller branch from each uniting to form the
lateral femoral cutaneous nerve, and a larger branch from each joining with the
dorsal division of the fourth nerve to form the femoral nerve. The accessory
Obturator, when it exists, is formed by the union of two small branches given
off from the third and fourth nerves.
3.3.8 Gray’s Anatomy
3.3.8.1
http://www.bartleby.com/107/212.html
3.3.8.2
Illustrations
3.3.8.2.1
http://www.bartleby.com/107/illus822.html
3.3.8.2.2
http://www.bartleby.com/107/illus823.html
3.3.8.2.3
http://www.bartleby.com/107/illus824.html
3.3.9 Number
3.3.9.1
3.3.10
Reference
3.3.10.1
62
3.3.11
Illustration
3.3.11.1
3.4 Lumbar Plexus
(Muscular Branches and Relationships) (63)
3.4.1 Spinal Roots
3.4.1.1
T12, L 1, L2, L3, L4 Ventral rami
3.4.2 Named Branches
3.4.2.1
None
3.4.3 Muscular Branches
3.4.3.1 A=Quadratus lumborum / T12,
L 1-L3.
3.4.3.2 B=Psoas
minor / L 1.
3.4.3.3
C=Psoas
major / L 1-L3
3.4.4 Articular Branches
3.4.4.1
None
3.4.5 Cutaneous Branches
3.4.5.1
None
3.4.6 Lumbar Plexus
Relations
3.4.6.1
The whole lumbar plexus pierces the psoas major,
divides into branches exiting from the:
3.4.6.2
Lateral Border of Psoas
3.4.6.2.1
D=Iliohypogastric nerve.
3.4.6.2.2
E=llio-inguinal nerve.
3.4.6.2.3
F=Lateral
femoral cutaneous nerve.
3.4.6.2.4
G=Femoral
nerve.
3.4.6.3
Anterolateral Border of Psoas
3.4.6.3.1
H=Genitofemoral
nerve
3.4.6.4
Anteromedial Border of Psoas
3.4.6.4.1
I=Obturator nerve.
3.4.6.4.2
J=Accessory Obturator nerve
(if present).
3.4.6.4.3
K=Upper
root of
lumbosacral trunk
3.4.7 Lesions
3.4.7.1
Root lesions to L2, L3 can weaken
the psoas major, however, L2 provides the greatest affect. Presents as weakness
or inability to flex the hip. Paresthesia or loss of sensation to the anterior
proximal thigh (femoral nerve L2) could further specify the root damage as L2
rather than L1.
3.4.8 Gray’s Anatomy
3.4.8.1
http://www.bartleby.com/107/212.html
3.4.9 Number
3.4.9.1
3.4.10
Reference
3.4.10.1
63
3.4.11
Illustration
3.4.11.1
3.5 Nerves from
Ventral Rami of Lumbar Plexus (64)
3.5.1 Illustration A
3.5.1.1
3.5.2 Illustration B
3.5.2.1
3.5.3 Number
3.5.3.1
3.5.4 Reference
3.5.4.1
64
3.6 Iliohypogastric
Nerve (65) (Blank)
3.6.1 Spinal Roots
3.6.1.1
3.6.2 Named Branches
3.6.2.1
3.6.3 Muscular Branches
3.6.3.1
3.6.4 Articular Branches
3.6.4.1
3.6.5 Cutaneous Branches
3.6.5.1
3.6.6 Lesions
3.6.6.1
3.6.7 Gray’s Anatomy
3.6.7.1
http://www.bartleby.com/107/212.html
3.6.8 Number
3.6.8.1
3.6.9 Reference
3.6.9.1
3.6.10
Illustration
3.6.10.1
3.7 ILLIOHYPOGASTRIC
(65)
Back
Table of Contents References
3.7.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
3.7.1.1
. EXITS THROUGH THE LATERAL BORDER OF THE PSOAS MAJOR.
INJURY TO THIS NERVE CAN RESULT FROM AN INCISION FOR AN APPENDECTOMY. PRESENTS
AS A WEAKNESS IN THE ABDOMINAL AREA OF INQUINAL CANL AND PARESTHESIA OF LOSS OF
SENSATION TO THE SKIN DESCRIBED IN THE CUTANEOUS SECTION FOR THIS NERVE. THE ABDONIMAL
WEKNESS MAY RESULT IN THE DEVELOPMENT OF A DIRECT INQUINAL HERNIA.
3.7.2 CUTANEOUS BRANCHES
3.7.2.1
LATERAL CUTANEOUS
3.7.2.1.1
L GLUTEAL SKIN
3.7.2.2
ANTERIOR CUTANEOUS
3.7.2.2.1
.
SUPRAPUBIC SKIN (HYPOGASTRIC REGION)
3.7.3 ARTICULAR BRANCHES
3.7.3.1
NONE
3.7.3.1.1
3.7.4 ROOTS
3.7.4.1
T12-L1
3.7.4.2
Lumbar Plexus
3.7.4.3
VENTRAL
3.7.5 MUSCULAR BRANCHES
3.7.5.1 TRANSVERSE
ABDOMINIS
3.7.5.1.1
SUPPLIED
BY THE VENTRAL RAMI T7-T12 AND THE ILLIOINGUINAL NERVES.
3.7.5.2 INTERNAL ABDOMINAL
OBLIQUE
3.7.5.2.1
SUPPLIED
BY THE VENTRAL RAMI T7-T12 AND THE ILLIOINGUINAL NERVES.
3.7.6 NUMBER
3.7.6.1
. 35 .02
3.7.7 REFERENCE
3.7.7.1
66
3.8 Ilio-Inquinal
Nerve (66) (Blank)
3.8.1 Spinal Roots
3.8.1.1
3.8.2 Named Branches
3.8.2.1
3.8.3 Muscular Branches
3.8.3.1
3.8.4 Articular Branches
3.8.4.1
3.8.5 Cutaneous Branches
3.8.5.1
3.8.6 Lesions
3.8.6.1
3.8.7 Gray’s Anatomy
3.8.7.1
http://www.bartleby.com/107/212.html
3.8.8 Number
3.8.8.1
3.8.9 Reference
3.8.9.1
3.8.10
Illustration
3.8.10.1
3.9 ILLIO-INGUINAL
(66)
Back
Table of Contents References
3.9.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
3.9.1.1
. EXITS THROUGH THE LATERAL BORDER OF THE PSOAS MAJOR.
INJURY TO THIS NERVE CAN RESULT BY AN INCISION FOR AN APPENDECTOMY AND
HERNIORRHAPHIES, DURNING PLANNENSTIEL'S (HORIZONTAL SUPRAPUBIC) INCISIONS, OR
NEPHRECTOMIES. SOMETIMES NORMAL PREGNACY AND DELIVERY CAN STRETCH THE NERVE.
THE PATIENT USUALLY COMPLAINS OF PARESTHESIA OR LOSS OF S4ENSATION TO THE SKIN
DECRIBED IN THE CUTANEOUS XERCTION FOR THIS NERVE. LIOHYPOGASTRIC,
ILIO-INGUINAL AND GENITOFEMORAL NERVES IN AND OF THEMSELVES MAY NOT BE AS
IMPORTANT AS PARESTHESIAS AND PAIN IN DISTRIBUTION. THIS BEING AN INDICATOR
IDENTIFYING (LOCALIZING) SPINAL NERVE LESIONS. ALSO PAIN FROM DISEASE OF THE
URETER AND RENAL PELVIS MAY REFER HERE.
3.9.2 CUTANEOUS BRANCHES
3.9.2.1
GROIN 35.031
3.9.2.1.1
PROXIMOMEDIAL SKIN OF THE THIGH(GROIN).
3.9.2.2
BASE O PENIS/MONS PUBIS 35.032
3.9.2.2.1
.
IN MALES THE SKIN OVER THE PENILE ROOT AND UPPER PART OF SCROTUM. IN FEMALES,
THE SKIN COVERING THE MONS PUBIS AND THE ADJOINING LABIUM MARORUS.
3.9.3 ARTICULAR BRANCHES
3.9.3.1
NONE
3.9.4 ROOTS
3.9.4.1
L1
3.9.4.2
Lumbar Plexus
3.9.4.3
VENTRAL
3.9.5 MUSCULAR BRANCHES
3.9.5.1 TRANSVERSE
ABDOMINIS
3.9.5.1.1
THIS
NERVE IS SUPPLIED BY THE VENTRAL RAMI T7-T12 AND THE ILLIOHYPOGASTRIC NERVES.
3.9.5.2 INTERNAL ABDOMINAL
OBLIQUE
3.9.5.2.1
THIS
NERVE IS SUPPLIED BY THE VENTRAL RAMI T7-T12 AND THE ILLIOHYPOGASTRIC NERVES.
3.9.6 NUMBER
3.9.6.1
. 35 .03
3.9.7 REFERENCE
3.9.7.1
67
3.10 Genitofemoral
Nerve (67) (Blank)
3.10.1
Spinal Roots
3.10.1.1
3.10.2
Named Branches
3.10.2.1
3.10.3
Muscular Branches
3.10.3.1
3.10.4
Articular Branches
3.10.4.1
3.10.5
Cutaneous Branches
3.10.5.1
3.10.6
Lesions
3.10.6.1
3.10.7
Gray’s Anatomy
3.10.7.1
http://www.bartleby.com/107/212.html
3.10.8
Number
3.10.8.1
3.10.9
Reference
3.10.9.1
3.10.10
Illustration
3.10.10.1
3.11 GENITAL FEMORAL
(67)
Back
Table of Contents References
3.11.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
3.11.1.1
. SCARRING AND ADHESIONS FROM APPENDECTOMIES CAN CONSTRICT
THE NERVE AND RESULT IN PARALYSIS OF THE CREMASTER MUSCLE. CREMASTERIC ACTIONS
ARE NOT USUALLY VOLUNTARY, RAISING TESTES, ESSENTIAL TO TESTICULAR
THERMOREGULATION. STIMULATION OF MEDIAL FEMORAL SKIN EVODES A REFLEX
CONTRACTION; THIS WOULD BE LOST. HOWEVER, THIS IS NOT CONSIDERED A
RELIABLETEST. PRESENTS AS A PARESTHESIA OR LOSS OF SENSATION TO THE SKIN IN THE
CUTANEOUS DESCRIPTION FOR THIS NERVE.
3.11.2
NUMBER
3.11.2.1
35.04
3.11.3
REFERENCE
3.11.3.1
68
3.11.4
ROOTS
3.11.4.1
L1-L2
3.11.4.2
Lumbar Plexus
3.11.4.3
VENTRAL
3.11.5
CUTANEOUS BRANCHES
3.11.5.1
GENITAL BR 35.041
3.11.5.1.1
SUPPLIES THE SCROTAL SKIN IN MALES AND IN FEMALES THE SKIN
OF THE MONS PUBIS, LABIUM MAJORUS AND PARTS OF VULVA INCLUDING THE CLITORIS,
LABIA MINOR VVAGINA GREATER VESTIBULE(BARTHOLIN) GLANDS, AND BULB OF VESTIBULA.
3.11.5.2
FEMORAL BR 35.042
3.11.5.2.1
.
SKIN OVER THE UPPER PART OF THE FEMORAL TRIANGLE.
3.11.6
ARTICULAR BRANCHES
3.11.6.1
NONE
3.11.7
MUSCULAR BRANCHES
3.11.7.1.1
CREMASTER
3.12 Nerves from
Ventral Division of Ventral Rami Lumbar Plexus (68)
3.12.1
Illustration A
3.12.1.1
3.12.2
Illustration B
3.12.2.1
3.12.3
Number
3.12.3.1
3.12.4
Reference
3.12.4.1
68
3.13 Obturator Nerve
(69) (Blank)
3.13.1
Spinal Roots
3.13.1.1
3.13.2
Named Branches
3.13.2.1
3.13.3
Muscular Branches
3.13.3.1
3.13.4
Articular Branches
3.13.4.1
3.13.5
Cutaneous Branches
3.13.5.1
3.13.6
Lesions
3.13.6.1
3.13.7
Gray’s Anatomy
3.13.7.1
http://www.bartleby.com/107/212.html
3.13.8
Number
3.13.8.1
3.13.9
Reference
3.13.9.1
3.13.10
Illustration
3.13.10.1
3.14 OBTURATOR (69)
Back
Table of Contents References
3.14.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
3.14.1.1
. L2-L4 VENTRAL DIVISION OF THE VENTRAL RAMI, EXITING
THROUGH THE MEDIAL BORDER OF THE PSOAS MAJOR. BEFORE PASSING THROUGH THE OBTURATOR
FORAMEN IT BIFURCATES INTO ANTERIOR AND POSTERIOR DIVISIONS.
3.14.1.2
INJURY TO THIS NERVE IS RARE. IT IS VULNERABLE TO SURGICAL
DAMAGE DURING PELVIC INTRUSION TO REMOVE MALIGNANT LYMPH NODES. PRESSURE FROM A
GRAVID UTERUS AND DAMAGE FROM SEVERE LABOUR IS NOT UNCOMMON. IT MAY ALSO BE
IRRITATED BY DISEASE OF AN OVARY.
3.14.1.3
PRESSENTS A WEAKNESS OR INABLIITY TO STABILIZE THE HIP.
PARALYSIS OF ADDUCTORS AND OBTURATOR EXTERNUS WEAKEN BY ADDUCTION AND EXTERNAL
ROTATION OF THE THIGH, MAKING CROSSING OF LEGS DIFFICULT. PARESTHESIA OR LOSS
OF SENSATION TO THE SKIN AREAS DESCRIBED.
3.14.1.4
HIP JOINT DISEASE MAY CAUSE REFERRED PAIN TO THE MEDIAL SIDE
OF THE THIGH. THE NERVE IS SOMETIMES SEVERED TO RELIEVE ADDUCTOR SPASM IN
SPASTIC PARALYSIS, PARAPLEGIA OR MULTIPLE SCLEROSIS. TO DIFFERENTIATE A FOCAL
OBTURATOR NERVE LESION FROM LUMBAR ROOT LESION, TEST THE FEMORAL NERVE, WHICH
IS ALSO DERIVES FROM L2-L4.
3.14.2
NUMBER
3.14.2.1
35.06
3.14.3
REFERENCE
3.14.3.1
85
3.14.4
ROOTS
3.14.4.1
S1-S2 S2-S3
3.14.4.2
Lumbar Plexus
3.14.4.3
VENTRAL
3.14.5
DIVISION
3.14.5.1
Anterior Posterior
3.14.6
ANT DIVISION(OBTURATOR) 35.061
3.14.6.1 MUSCULAR BRANCHES
(Ant Div)
3.14.6.1.1.1
ADDUCTOR
LONGUS L2,L3,L4
3.14.6.1.1.2
GRACILLIS
L2,L3
3.14.6.1.1.3
ADDUCTOR
BREVIS L3,L4
3.14.6.1.1.3.1SOMETIMES FROM POSTERIOR BRANCH OF OBTURATOR NERVE ALSO
3.14.6.1.1.4
PECTINEUS L2,L3
3.14.6.1.1.4.1THIS USUALLY RECEIVES FROM THE FEMORAL NERVE OR SOMETIMES THE ACCESSORY OBTURATOR NERVE WHEN PRESENT
3.14.6.1.1.5
3.14.6.2 ARTICULAR
BRANCHES(ANT DIV)
3.14.6.2.1
HIP
3.14.6.3 CUTANEOUS BRANCHES(ANT DIV)
3.14.6.3.1
TO
THE SKIN ON THE MEDIAL SIDE OF THIGH.
3.14.7
POSTERIOR DIVISION(OBTURATOR)
3.14.7.1
MUSCULAR BRANCHES (Posterior Div)
3.14.7.1.1
OBTURATOR
EXXTERNUS L3,L4
3.14.7.1.2
ABDUCTOR
MAGNUS (PROXIMAL HORIZONTAL) L2,L3,L4
3.14.7.1.2.1
THE
DISTAL (ISCHIOCONDYLAR) MUSCULAR FIBERS ARE SUPPLIED BY TIBIAL DIVISION OF
SCIATIC NERVE.
3.14.7.1.3
ADDUCTOR
BREVIS (SOMETIMES) L3,L4
3.14.7.2
ARTICULAR BRANCHES(POST DIV)
3.14.7.2.1
KNEE
(SOMETIMES ABSENT)
3.15 Accessory
Obturator Nerve (70) (Blank)
3.15.1
Spinal Roots
3.15.1.1
3.15.2
Named Branches
3.15.2.1
3.15.3
Muscular Branches
3.15.3.1
3.15.4
Articular Branches
3.15.4.1
3.15.5
Cutaneous Branches
3.15.5.1
3.15.6
Lesions
3.15.6.1
3.15.7
Gray’s Anatomy
3.15.7.1
http://www.bartleby.com/107/212.html
3.15.8
Number
3.15.8.1
3.15.9
Reference
3.15.9.1
3.15.10
Illustration
3.15.10.1
3.16 ACCESSORY
OBTURATOR (70)
Back
Table of Contents References
3.16.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
3.16.1.1
. EXITING THROUGH THE MEDIAL BOARDER OF PSOAS MAJOR. THIS
NERVE IS PRESENT ABOUT 30% OF THE TIME WITH VARIATIONS.
3.16.1.2
IF PRESENT AND INJURED IT COULD MINIMALLY WEKEN ADDUCTION
AND FLEXION OF THE HIP JOINT.
3.16.2
NUMBER
3.16.2.1
None
3.16.3
REFERENCE
3.16.3.1
71
3.16.4
ROOTS
3.16.4.1
L3, L4
3.16.4.2
Lumbar Plexus
3.16.4.3
VENTRAL
3.16.5
DIVISION
3.16.5.1
None
3.16.6
CUTANEOUS BRANCHES
3.16.6.1
None
3.16.7
ARTICULAR BRANCHES
3.16.7.1
None
3.16.7.1.1
3.16.8
MUSCULAR BRANCHES
3.16.8.1 PECTINEUS
3.16.8.1.1
THE
PECTINEUS MAY BE DIVIDED INTO ANTERIOR AND POSTERIOR STRATA. THE ACCESSORY
OBTURATOR OR OBTURATOR NERVES SUPPLYING THE POSTERIOR STRATUM; THE FEMORAL NERVE
SUPPLIES THE ANTERIOR STRATUM.
3.16.8.2 ADDUCTOR
LONGUS (SOMETIMES)
3.17 Lumbar Plexus
(Nerves from Dorsal Divisions-Ventral Rami (71)
3.17.1
Illustration # A
3.17.1.1
3.17.2
Illustration # B
3.17.2.1
3.17.3
REFERENCE
3.17.3.1
71
3.18 Lateral Cutaneous
Femoral Nerve (72) (Blank)
3.18.1
Spinal Roots
3.18.1.1
3.18.2
Named Branches
3.18.2.1
3.18.3
Muscular Branches
3.18.3.1
3.18.4
Articular Branches
3.18.4.1
3.18.5
Cutaneous Branches
3.18.5.1
3.18.6
Lesions
3.18.6.1
3.18.7
Gray’s Anatomy
3.18.7.1
http://www.bartleby.com/107/212.html
3.18.8
Number
3.18.8.1
3.18.9
Reference
3.18.9.1
3.18.10
Illustration
3.18.10.1
3.19 Femoral Nerve
(Abdominal Branches) (73) (Blank)
3.19.1
Spinal Roots
3.19.1.1
3.19.2
Named Branches
3.19.2.1
3.19.3
Muscular Branches
3.19.3.1
3.19.4
Articular Branches
3.19.4.1
3.19.5
Cutaneous Branches
3.19.5.1
3.19.6
Lesions
3.19.6.1
3.19.7
Gray’s Anatomy
3.19.7.1
http://www.bartleby.com/107/212.html
3.19.8
Number
3.19.8.1
3.19.9
Reference
3.19.9.1
3.19.10
Illustration
3.19.10.1
3.20 Femoral Nerve
(Anterior Division) (74) (Blank)
3.20.1
Spinal Roots
3.20.1.1
3.20.2
Named Branches
3.20.2.1
3.20.3
Muscular Branches
3.20.3.1
3.20.4
Articular Branches
3.20.4.1
3.20.5
Cutaneous Branches
3.20.5.1
3.20.6
Lesions
3.20.6.1
3.20.7
Gray’s Anatomy
3.20.7.1
http://www.bartleby.com/107/212.html
3.20.8
Number
3.20.8.1
3.20.9
Reference
3.20.9.1
3.20.10
Illustration
3.20.10.1
3.21 LAT FEM CUT (?)
Back
Table of Contents References
3.21.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
3.21.1.1
. L2-3 DORSAL DIVISION FROM THE VENTRAL RAMI EXITING THROUGH
THE LATYERAL BAORDER OF PSOAS MAJOR.
3.21.1.2
PRESENTS AS PARESTHESIA OR LOSS OF SENSATION TO THE SKIN
AREA DESCRIBED.
3.21.2
NUMBER
3.21.2.1
35.07
3.21.3
REFERENCE
3.21.3.1
73
3.21.4
ROOTS
3.21.4.1
L2, L3
3.21.4.2
Lumbar Plexus
3.21.4.3
VENTRAL
3.21.5
DIVISION
3.21.5.1
Dorsal
3.21.6
CUTANEOUS BRANCHES
3.21.6.1
ANTERIOR 35.071
3.21.6.1.1
SUPPLIES THE SKIN OF THE ANTEROLATERAL THIGH
AS FAR DISTAL AS THE KNEE AND FORMS PART OF PATELLAR PLEXUS.
3.21.6.2
POSTERIOR 35.072
3.21.6.2.1
.
SUPPLIES THE SKIN OF THE LATERAL THIGH FROM THE GREATER TROCHANTER TO ABOUT THE
MID-THIGH: IT MAY ALSO SUPPLY SOME OF THE GLUTEAL SKIN.
3.21.7
ARTICULAR BRANCHES
3.21.7.1
None
3.21.8
MUSCULAR BRANCHES
3.21.8.1 None
3.22 FEMORAL NERVE (?)
Back
Table of Contents References
3.22.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
3.22.1.1
. Femoral nerve: injuries to the femoral nerve are usually
due to trauma in the area of the femoral triangle. however, a tubercular
abscess involving the psoas muscles can cause nerve compression, and disease
from intervertebral lumbar discs and sacroiliac joints may cause spasm of the
Iliopsoas, a Hematoma in the psoas muscle or beneath the iliacus fascia, can
compress the femoral nerve between the inguinal ligament and the iliac bone.
consequently, the iliacus and pectineus muscles could be weakened or paralysed,
presenting as weak hip flexion. see also lesions of femoral nerve, anterior and
posterior divisions, for further deficits.
femoral nerve(anterior div): injury to the anterior division of the
femoral nerve alone would result in paralysis of the Sartorius muscle,
presenting as weak knee flexion and contributing to instability of the
anteromedial knee. Additionally, decreased strength in hip adduction, lateral
rotation and flexion may bve seen. paresthesia or loss of sensation also occurs
in the skin areas described above. a lesion proximal to the ingunal ligament
would affect paralysis to both the anterior and posterior branches. femoral
nerve(post div): (posterior branch); injury to the posterior branch of the
femoral nerve is usually a result of trauma to the femoral triangle. this would
produce wek hip flexion due to paralysis of rectus Femoris. knee extension will
be all but obliterated due to paralysis to the entire quadriceps group; loss of
patella tendon reflex is also seen. to isolate focal femoral nerve lseion from
lumbar root, test the Obturator nerve, both derive from l2-l4. often both
obturator and femoral nerves are affected. (saphenous nerv); trauma is the
typical cause of injury to the saphenous nerve. it is in particular danger
during operations on varicose veins, and the infrapatellar granch can be
damaged during knee surgery. injury will present paresthesia or loss of
sensation to the skin areas described above. l4 is the primary root of the saphenous nerve. for
focal differential diagnosis, check hip adductors (obturator enrve) and the
Tibialis anterior (common Peroneal nerve) for l4 radiculopathy as opposed to
femoral focal neuropathy.
3.22.1.2
3.22.2
NUMBER
3.22.2.1
35.08
3.22.3
REFERENCE
3.22.3.1
74 75 76
3.22.4
ROOTS
3.22.4.1
L2, L3, L4
3.22.4.2
Lumbar Plexus
3.22.4.3
VENTRAL
3.22.5
DIVISION
3.22.5.1
Dorsal
3.22.6
FEMORAL (ANT DIV)(FEM N.) 35.081
3.22.6.1 CUTANEOUS BRANCHES
3.22.6.1.1
INTERMED
FEM CUT L2, L3 35.0811
3.22.6.1.1.1
L2 & L3 divides into medial and lateral
branches
3.22.6.1.1.2
MEDIAL
(Intermediate Femoral Cutaneous) 35.08111
3.22.6.1.1.2.1Supplies the anteromedial thigh as far distal as the knee and terminating the the patellar plexus
3.22.6.1.1.3
.
LATERAL(INT FEM CUT) 35.08112
3.22.6.1.1.3.1Supplies the anterolateral thigh as far distal as the knee and terminating the the patellar plexus
3.22.6.1.2
MEDIAL
FEM CUT L2, L3 35.0812
3.22.6.1.2.1
L2
& L3 SENDS A FEW RAMI TO SUPPLY THE SKIN (SEE NEXT COLLUM). THE NERVE THEN
DIVIDES INO ANTERIOR AND POSTERIOR.
3.22.6.1.2.2
SKIN
OF THE MEDIAL SIDE OF THE THIGH.
3.22.6.1.2.3
ANTERIOR(MED
FEM CUT) 35.08121
3.22.6.1.2.3.1SKIN OVER THE SARTORIUS BEYOND THE MID-THIGH.
3.22.6.1.2.4
POSTERIOR(MED
FEM CUT) 35.08122
3.22.6.1.2.4.1SKIN OVER THE ANTEROMEDIAL AND POSTEROMEDIAL ASPECTS OF THE KNEE AS FAR DISTAL AS THE LEG, FORMING PQART OF THE PATTELLAR PLEXUS.
3.22.6.2 ARTICULAR BRANCHES
3.22.6.2.1
None
3.22.6.3 MUSCULAR BRANCHES
(FEM ANT DIV)
3.22.6.3.1
SARTORIUS
L2, L3
3.22.6.3.1.1
Arising
in common with the lateral branch of intermediate femoral cutaneous nerve
3.22.7
FEMORAL(ABDOMINAL BRANCHES)(FEM N.)
3.22.7.1 MUSCULAR
BRANCHES(FEM ABD B)
3.22.7.1.1
ILLIACUS
L2, L3
3.22.7.1.2
PECTINEUS
L2, L3
3.22.7.1.2.1
THE
PECTINEUS MAY ALSO BE SUP[PLIED BY THE OBTURATOR AND OR ACCESSORY OBTURATOR
NERVES.
3.23 Femoral Nerve
(Posterior Division) (75)
3.23.1
Spinal Roots
3.23.1.1
L2, L3, L4
3.23.1.1.1
Dorsal divisions of the ventral
rami. It exits through he lateral border of the psoas major, passing deep to,
and branching distal to, the inguinal ligament.
3.23.2
Named Branches
3.23.2.1
A=Anterior
division of femoral nerve
3.23.3
Muscular Branches
3.23.3.1
B=Rectus femoris /
L2, L3, L4.
3.23.3.2
C=Vastus
Lateralis / L2, L3, L4.
3.23.3.3
D=Vastus
Medialis / L2, L3, L4.
3.23.3.4 E=Vastus Intermedius / L2,
L3,
L4.
3.23.3.5
F=Articular
genus, from a branch to Vastus Intermedius
3.23.4
Articular Branches
3.23.4.1
G=To the hip from a
branch to rectus femoris.
3.23.4.2
H=Three
branches to knee (lateral, medial and intermediate) from the Vastus muscles of the
same name
3.23.5
Cutaneous Branches
3.23.5.1
I=Saphenous nerve /
L3, L4
3.23.5.1.1
Path
Description
3.23.5.1.1.1
Summary
3.23.5.1.1.1.1Enters adductor canal and emerges on the medial side of the knee forming part of the patellar plexus. Between sartorius and gracilis it becomes cutaneous, supplying the skin over the medial tibial border to the ankle and medial side of the foot.
3.23.5.1.1.2
Detailed
3.23.5.1.1.2.1The Saphenous Nerve (n. saphenous; long or internal saphenous nerve) (Fig. 827) is the largest cutaneous branch of the femoral nerve. It approaches the femoral artery where this vessel passes beneath the Sartorius, and lies in front of it, behind the aponeurotic covering of the adductor canal, as far as the opening in the lower part of the Adductor magnus. Here it quits the artery, and emerges from behind the lower edge of the aponeurotic covering of the canal; it descends vertically along the medial side of the knee behind the Sartorius, pierces the fascia lata, between the tendons of the Sartorius and Gracilis, and becomes subcutaneous. The nerve then passes along the tibial side of the leg, accompanied by the great saphenous vein, descends behind the medial border of the tibia, and, at the lower third of the leg, divides into two branches: one continues its course along the margin of the tibia, and ends at the ankle; the other passes in front of the ankle, and is distributed to the skin on the medial side of the foot, as far as the ball of the great toe, communicating with the medial branch of the superficial peroneal nerve.
3.23.5.2
J=Infrapatellar branch
3.23.5.2.1
Supplies prepatellar skin with
branches to patellar plexus.
3.23.6
Lesions
3.23.6.1
: To Posterior branch
3.23.6.1.1
Injury
to the posterior branch of the femoral nerve is usually a result of trauma to
the femoral triangle. This would produce weak hip flexion due to paralysis of
rectus femoris. Knee extension will be all but obliterated due to paralysis to
the entire quadriceps group; loss of patella tendon reflex is also seen. To
isolate focal femoral nerve lesion from lumbar root, test the Obturator nerve;
both derive from L2-L4. Often both Obturator and femoral nerves are affected
3.23.6.2
. To Saphenous nerve
3.23.6.2.1
Trauma is the typical cause of
injury to the Saphenous nerve. It is in particular danger during operations on
varicose veins, and the Infrapatellar branch can be damaged during knee
surgery. Injury will present paresthesia or loss of sensation to the skin areas
as described above. L4 is primary root of Saphenous nerve. For focal
differential diagnosis, check hip adductors (Obturator nerve) and the tibialis
anterior (common peroneal nerve) for L4 Radiculopathy as opposed to femoral
focal neuropathy.
3.23.7
Path Description
3.23.7.1
The Femoral Nerve (n. femoralis; anterior crural nerve)
(Fig. 827), the largest branch of the lumbar plexus, arises from the dorsal
divisions of the second, third, and fourth lumbar nerves. It descends through
the fibers of the Psoas major, emerging from the muscle at the lower part of
its lateral border, and passes down between it and the Iliacus, behind the
iliac fascia; it then runs beneath the inguinal ligament, into the thigh, and
splits into an anterior and a posterior division. Under the inguinal ligament,
it is separated from the femoral artery by a portion of the Psoas major.
3.23.7.2
Within the abdomen
the femoral nerve gives off small branches to the Iliacus, and a branch, which
is distributed upon the upper part of the femoral artery; the latter branch may
arise in the thigh.
3.23.7.3
In the thigh the
anterior division of the femoral nerve gives off anterior cutaneous and
muscular branches. The anterior cutaneous branches comprise the intermediate
and medial cutaneous nerves (Fig. 825).
3.23.8
Gray’s Anatomy
3.23.8.1
http://www.bartleby.com/107/212.html
3.23.8.2
Illustrations
3.23.8.2.1
http://www.bartleby.com/107/illus827.html
3.23.8.2.2
http://www.bartleby.com/107/illus825.html
3.23.9
Number
3.23.9.1
35.082
3.23.10
Reference
3.23.10.1
75
3.23.11
Illustration
3.23.11.1
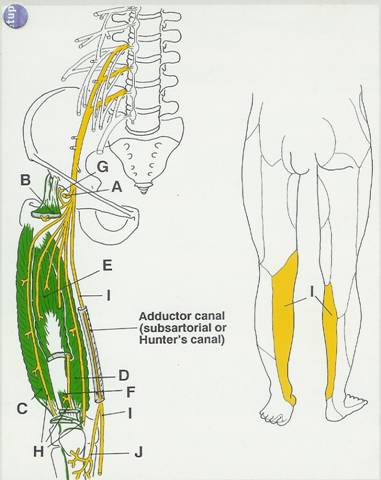
3.24
Sacral Plexus
(Spinal Segments & Nerves) (76)
3.24.1
Spinal Segments
3.24.1.1
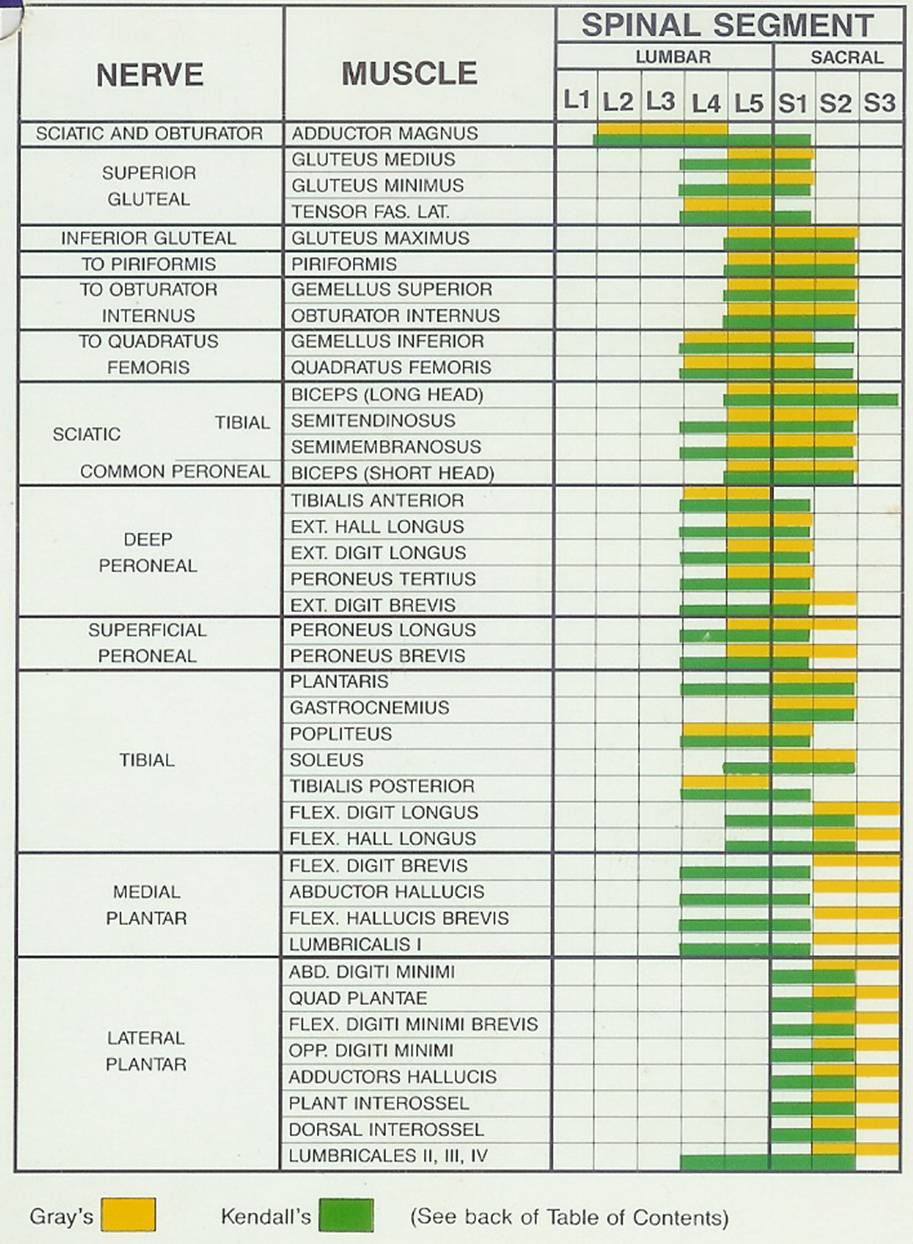
3.24.2
Nerves
3.24.2.1
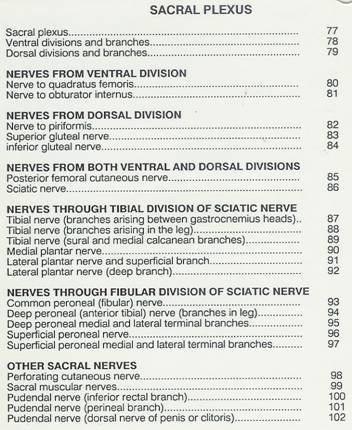
3.24.3
Number
3.24.3.1
3.24.4
Reference
3.24.4.1
76
3.25 Sacral Plexus (L4,
L5, S1, S2, S3) (77)
Back
Table of Contents References
3.25.1
Named Branches
3.25.1.1
A=Nerve to quadratus
femoris
I L4, L5, S1.
3.25.1.2
B=Nerve to
Obturator Internus; L5, S1, S2.
3.25.1.3
C=Nerve to
Piriformis; S1, S2.
3.25.1.4
D=Superior Gluteal
nerve; L4, L5, S1.
3.25.1.5
E=Inferior Gluteal
nerve; L5, S1, S2.
3.25.1.6
F=Posterior femoral
cutaneous nerve; S1-S3.
3.25.1.7
G=Sciatic nerve;
L4, L5, S1-S3.
3.25.1.8
H=Tibial division;
L4, L5, S1-S3.
3.25.1.9
I=Common
peroneal; L4, L5,
S1, S2.
3.25.2
Cutaneous Branches
3.25.2.1
J=Sural nerve; L5,
S1, S2.
3.25.2.2
K=Medial calcanean;
S1, S2.
3.25.2.3
L=Medial plantar
nerve; L4, L5.
3.25.2.4
M=Lateral plantar nerve;
S1, S2.
3.25.2.5
N=Lateral sural
nerve; L4, L5, S1.
3.25.2.6
0=Medial terminal
branch of deep peroneal; S1, S2.
3.25.2.7
P=Superficial
peroneal segments
3.25.3
Lesions
3.25.3.1
: Injury to L4 (lumbosacral trunk):
3.25.3.1.1
Produces
weak knee extension (Obturator nerve) with reduced patellar tendon reflex and
paresthesia to the skin of the medial leg (femoral and saphenous
nerves), weak hip adduction (sciatic nerve), "foot drop" from loss of
tibialis anterior and posterior (tibial and deep peroneal nerves) and
paresthesias to the skin of the medial side of the sole of the foot (medial
plantar nerve).
3.25.3.2
Injury to L5: "Trendelenburg's
sign" (superior Gluteal nerve),
3.25.3.2.1
Weak
knee flexion (tibial nerve), weak dorsiflexion ("foot drop") and
eversion of foot at the subtalar and intertarsal joints weak extension of toes
and paresthesias to the skin of lateral leg, Dorsum of foot and middle sole of
foot (common, deep and superficial peroneal nerves).
3.25.3.3
Injury to S1:
3.25.3.3.1
Weak
hip extension (tibial nerve), plantarflexion and toe flexion (deep peroneal
nerve)
3.25.3.4
Injury of S2-Sj
3.25.3.4.1
Paresthesia
to skin of posterior thigh and leg (posterior femoral cutaneous nerve), weak
plantar flexion and inversion of foot weak flexion adduction/abduction of toe
(tibial nerve), and loss of voluntary control of pelvic floor and anal
sphincter (pudendal nerve)
3.25.4
Path Description
3.25.4.1
The sacral plexus is formed by the lumbosacral trunk, the
anterior division of the first, and portions of the anterior divisions of the
second and third sacral nerves.
3.25.4.2
The lumbosacral
trunk comprises the whole of the anterior division of the fifth and a part of
that of the fourth lumbar nerve; it appears at the medial margin of the Psoas
major and runs downward over the pelvic brim to join the first sacral nerve.
The anterior division of the third sacral nerve divides into an upper and a
lower branch, the former entering the sacral and the latter the pudendal
plexus.
3.25.4.3
The nerves forming
the sacral plexus converge toward the lower part of the greater sciatic
foramen, and unite to form a flattened band, from the anterior and posterior
surfaces of which several branches arise. The band itself is continued as the
sciatic nerve. which splits on the back of the thigh into the tibial and common
peroneal nerves; these two nerves sometimes arise separately from the plexus,
and in all cases their independence can be shown by dissection.
3.25.4.4
Relation
3.25.4.4.1
The
sacral plexus lies on the back of the pelvis between the Piriformis and the
pelvic fascia (Fig. 829); in front of it are the hypogastric vessels, the
ureter and the sigmoid colon. The superior gluteal vessels run between the
lumbosacral trunk and the first sacral nerve, and the inferior gluteal vessels
between the second and third sacral nerves.
3.25.4.4.2
All the nerves entering the plexus, with the
exception of the third sacral, split into ventral and dorsal divisions,
3.25.5
Gray’s Anatomy
3.25.5.1
http://www.bartleby.com/107/213.html
3.25.5.2
Illustration
3.25.5.2.1
http://www.bartleby.com/107/illus828.html
3.25.5.2.2
http://www.bartleby.com/107/illus829.html
3.25.6
Number
3.25.6.1
?
3.25.7
Reference
3.25.7.1
77
3.25.8
Illustration
3.25.8.1
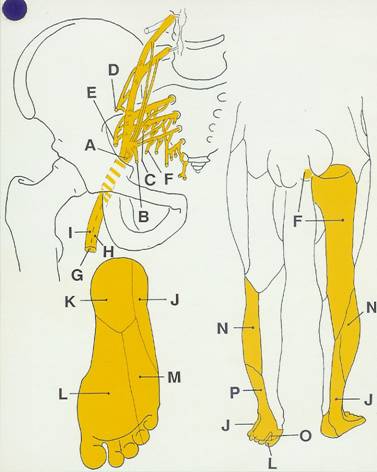
3.26 Sacral Plexus
(Nerves from Ventral Divisions of Ventral Rami) (78)
3.26.1
Illustration # A
3.26.1.1
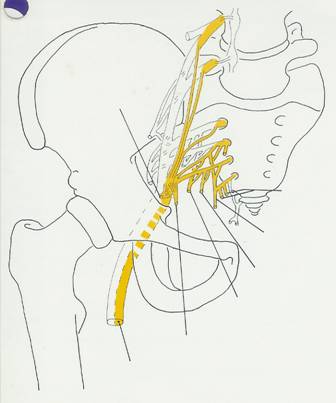
3.26.2
Illustration # B
3.26.2.1
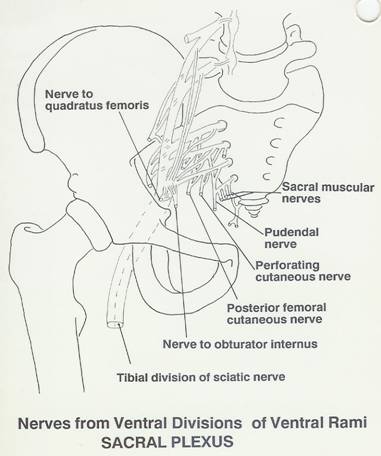
3.26.3
Number
3.26.3.1
?
3.26.4
Reference
3.26.4.1
78
3.27 Sacral Plexus
(Nerves from Dorsal Divisions of Ventral Rami) (79)
3.27.1
Illustration # A
3.27.1.1
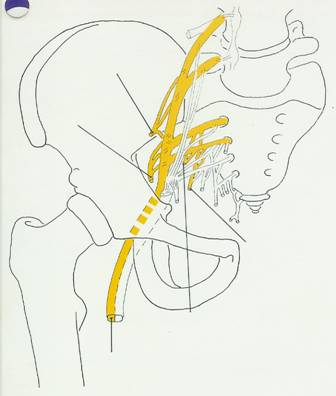
3.27.2
Illustration # B
3.27.2.1
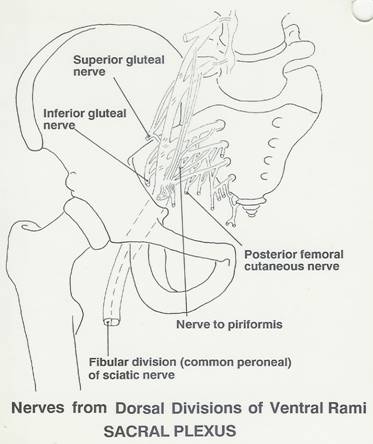
3.27.3
Number
3.27.3.1
?
3.27.4
Reference
3.27.4.1
79
3.28 QUADRATUS FEMORIS
N. (80)
Back
Table of Contents References
3.28.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
3.28.1.1
. Very seldom injured by itself. a focal loss of this nerve
would weaken external rotation of the extended thigh. posssible causes are trauma,
hip dislocation, or malignant tumors arising from the pelvis, abdomen, or
retroperitoneal structures. a herniated intervertebral disc or bony
abnormalities from degenerative arthritis (spondyliosis) can also compress the
lumbosacral trunk. each of the donditions above could show multiple deficits
pertaining to l4 and l5. all nerves exiting from pelvic cavity may be
vulnerable to these same traumas/etiologies; depending on the actual location
various effects are seen.
3.28.2
NUMBER
3.28.2.1
None
3.28.3
REFERENCE
3.28.3.1
80
3.28.4
ROOTS
3.28.4.1
L4,L5,S1
3.28.4.2
Sacral Plexus
3.28.4.3
VENTRAL
3.28.5
DIVISION
3.28.5.1
Ventral
3.28.6
CUTANEOUS BRANCHES
3.28.6.1
None
3.28.7
ARTICULAR BRANCHES
3.28.7.1
HIP
3.28.8
MUSCULAR BRANCHES
3.28.8.1 QUADRATUS FEMORIS
L4-S1
3.28.8.2 GEMEILUS INFERIOR
L4-S1
3.29 OBTURATOR INTERNUS
(81)
Back
Table of Contents References
3.29.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
3.29.1.1
. VERY SELDOM INJURED BY ITSELF. A FOCAL LOSS OF THIS NERVE
WOULD WEAKEN EXTERNAL ROTATION OF THE EXTENDED THIGH AND ABDUCTION OF THE
FLEXED HIP. POSSIBLE CAUSES ARE TRAUMA, HIP DISLOCATION OR MALIGNANT TUMORS
ARISING FROM PELVIC, ABDOMINAL OR RETROPERITONEAL STRUCTURES. A HERNIATED
INTERVERTEBRAL DISC OR BONY ABNORMALITIES FROM DEGENERATIVE ARTHRITIS
(SPONDYLOSIS) CAN COMPRESS LUMBOSACRAL TRUNK ROOTS OR CAUDA EQUINA. ALL OF
WHICH WOULD SHOW MULITIPLE DEFICITS PERTQAINING TO L-L5. ALL NERVES EXITING
FROM PELVIC CAVITY MAY BE VULNERABLE TO THESE SAME TRAMAS/ETIOLOGIES, DEPENDING
ON DISTRIBUTION VARIOUS EFFECTS ARE SEEN.
3.29.2
NUMBER
3.29.2.1
3.29.3
REFERENCE
3.29.3.1
81
3.29.4
ROOTS
3.29.4.1
L5-S2
3.29.4.2
Sacral Plexus
3.29.4.3
VENTRAL
3.29.5
DIVISION
3.29.5.1
Ventral
3.29.6
CUTANEOUS BRANCHES
3.29.6.1
None
3.29.7
ARTICULAR BRANCHES
3.29.7.1
None
3.29.8
MUSCULAR BRANCHES (OBTUR INTER)
3.29.8.1 OBTURATOR INTERNUS
L5-S2
3.29.8.2 GEMEILUS SUPERIOR
L5-S2
3.30 PIRIFORMIS (82)
Back
Table of Contents References
3.30.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
3.30.1.1
. FOCAL LOSS OF THIS NERVE WOULD PARALYZE THE PIRIFORMIS
MUSCLE, RESULTIN IN WEAK LATERL ROTATION OF THE EXTENDED HIP AND ABDUCTION OF
THE FLEXED HIP.
3.30.2
NUMBER
3.30.2.1
None
3.30.3
REFERENCE
3.30.3.1
82
3.30.4
ROOTS
3.30.4.1
S1-S2
3.30.4.2
Sacral Plexus
3.30.4.3
VENTRAL
3.30.5
DIVISION
3.30.5.1
Dorsal
3.30.6
CUTANEOUS BRANCHES
3.30.6.1
None
3.30.7
ARTICULAR BRANCHES
3.30.7.1
None
3.30.8
MUSCULAR BRANCHES
3.30.8.1 PIRIFORMIS L5-S2
3.31 SUPERIOR GLUTEAL
(83)
Back
Table of Contents References
3.31.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
3.31.1.1
. THIS IS THE ONLY NERVE TO PASS THROUGH THE GREATER SCIATIC
FORAMEN ABOVE THE PIRIFORMIS MUSCLE, SO IT MAY BE DAMAGED WHEN OTHER NERVES ARE
SPARED; SUPERIOR GHLUTEAL NERVE IS RARELY INJURED ALONE. A RARE MISPLACEN
INJECTION MAY BE AT FAULT. A FOCAL LESION WOULD RESULT IN THE PARALYSIS OF THE
GLUTEUS MEDIUS AND MINIMUS AND TENSOR FASCIA LATAE MUSCLES. ALL ARE ABDUCTORS
OF THE HIP AND THE ANTERIOR FIBERS OF THE GLUTEAL MUSCLES INTERNALLY ROTATE
HIP/THIGH. THE GLUTEAL MUSCLES ARE ESSENTIAL FOR STABILIZING THE TRUNK WHEN THE
OPPOSITE FOOT IS RAISED WHILE STANDING OR IN WALKING. A LESION PRESENT S AS A
DROPPING OF THE PELVIS TO OPPOSITE SIDE WHEN THE AFFECTED LIMB IS ELEVATED
(I.E. TRENDELENBURG'S SIGN OR GAIT). A SIMILAR GAIT OCCURS IN UNILATERAL
POSTERIOR DISLOCATION OF THEHIP OR A PAINFUL SACROILIAC JOINT BOTH LEADING TO
TRENDELENBURG'S SIGN THROUGH INABILITY OR REFLEX INHIBITION OF GLUTEUS MEDIUS
AND MINIMUS ACTION.
3.31.2
NUMBER
3.31.2.1
3.31.3
REFERENCE
3.31.3.1
83
3.31.4
ROOTS
3.31.4.1
L4-S1
3.31.4.2
Sacral Plexus
3.31.4.3
VENTRAL
3.31.5
DIVISION
3.31.5.1
Dorsal
3.31.6
CUTANEOUS BRANCHES
3.31.6.1
None
3.31.7
ARTICULAR BRANCHES
3.31.7.1
ARTICULAR BRANCH(S. GLUTEAL)
3.31.7.1.1
SACROILIAC
3.31.8
SUPERIOR BRANCH(S. GLUTEAL)
3.31.8.1 MUSCULAR BRANCHES
3.31.8.1.1
GLUTEUS
MEDIUS L5-S1
3.31.8.1.2
GLUTEUS
MINIMUS L5-S1
3.31.8.1.2.1
RARE
3.31.8.1.3
3.31.9
INFERIOR BRANCH(S. GLUTEAL)
3.31.9.1 MUSCULAR BRANCHES
3.31.9.1.1
GLUTEUS
MEDIUS L5-S1
3.31.9.1.2
GLUTEUS
MINIMUS L5-S1
3.31.9.1.3
TENSOR
FASCIA LATA L4-S1
3.32 INFERIOR GLUTEAL
(84)
Back
Table of Contents References
3.32.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
3.32.1.1
. The inferior gluteal nerve is injured more ferquently than
the superior gluteal nerve, and is almost never damaged without associated
lesions of the sciatic, pudendal, or posterior femoral cutaneous nerves of the
thigh. Focal lesions would present weakness to extend the flexed hip, causing
difficulty in climbing stairs, standing from a seated position, and running or
jumping.
3.32.2
NUMBER
3.32.2.1
None
3.32.3
REFERENCE
3.32.3.1
84
3.32.4
ROOTS
3.32.4.1
L5-S2
3.32.4.2
Sacral Plexus
3.32.4.3
VENTRAL
3.32.5
DIVISION
3.32.5.1
Dorsal
3.32.6
CUTANEOUS BRANCHES
3.32.6.1
None
3.32.7
ARTICULAR BRANCHES
3.32.7.1
3.32.7.1.1
3.32.8
MUSCULAR BRANCHES
3.32.8.1 GLUTEUS MAXIMUS
L5-S2
3.32.8.1.1
Deep
surface after exiting greater sciatic foramen descending around the pirformis
muscle.
3.33 POSTERIOR FEMORAL
CUTANEOUS (85)
Back
Table of Contents References
3.33.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
3.33.1.1
. AFOCAL LESION TH THIS NERVE WILL PRODUCE PARESTHESIA OR LOSS
OF SENSATION TO THE SKIN AREA OF THIS NERVE. PROLONGED BICYCLE RIDING CAN
COMPRESS THE CLUNEAL BRANCHES RESULTING IN TEMPORARY NUMBNESS OF THE ARES
SUPPLIED.
3.33.2
NUMBER
3.33.2.1
35.05
3.33.3
REFERENCE
3.33.3.1
85
3.33.4
ROOTS
3.33.4.1
S1-S2 S2-S3
3.33.4.2
Sacral Plexus
3.33.4.3
VENTRAL
3.33.5
DIVISION
3.33.5.1
Dorsal Ventral
3.33.6
CUTANEOUS BRANCHES
3.33.6.1
INFERIOR CLUNEAL(GLUTEAL)
3.33.6.1.1
3
OR 4 BRANCHES CURL AROUND THE LOWERBORDER OF THE GLUTEUS MAXIMUS
3.33.6.1.2
Supplies SKIN OVER INFERIOR ASPEXT OF BUTTOCKS
(LOWER MEDIAL AUADRANT OF BUTTOCKS).
3.33.6.2
PERINEAL
3.33.6.2.1
.
SUPEROMEDIAL SKIN OF THE THIGH BELOW THE ISCHIAL TUBEROSITY TO THE SUPERFICIAL
PERINEAL FAXCIA SUPPLYING THE POSTERIOR SCROTAL OR LABIAL SKIN.
3.33.6.2.2
COMMUNICATING(PERINEAL)
3.33.6.2.2.1
PUDENDAL(COM)
3.33.6.2.2.1.1
3.33.6.3
BACK O THIGH BR
3.33.6.3.1
SUPERFICIAL
TO THE LONGG HEAD OF THE BICEPS FEMORIS WITH NUMEROUS BRANCHES FROM BOTH SIDES
OF IT.
3.33.6.3.2
SUPPLIES
THE SKIN OF THE BACK AND MEDIAL THIGH, THE POPLITEAL FOSSA AND THE PROXIMAL
PART OF THE BACK OF THE LEG.
3.33.7
ARTICULAR BRANCHES
3.33.7.1
NONE
3.33.8
MUSCULAR BRANCHES
3.33.8.1 NONE
3.34 Sciatic Nerve (86)
Back
Table of Contents References
3.34.1
Spinal Roots
3.34.1.1
A=Tibial
division (Ventral division): L4, LS, S1, S2, S3
3.34.1.1.1
Through
the ventral division of the sacral plexus
3.34.1.2
B=Common
peroneal (fibular) division (Dorsal division): L4, LS, S1,
S2
3.34.1.2.1
Through the dorsal division of the
sacral plexus
3.34.2
Muscular Branches
3.34.2.1
C=
Biceps femoris (short head) common peroneal LS, S1, S2
3.34.2.2
D=
Biceps femoris (long head) tibial division LS, 51, S2, S3
3.34.2.3
E=
Semitendinosus / tibial
division, L5, 51, S2
3.34.2.4
F=
Semimembranosus / tibial
division, LS, S1, S2
3.34.2.5
G=
Adductor magnus / tibial division, L4
3.34.3
Note
3.34.3.1
The horizontal fibers of the
adductor magnus are supplied by the Obturator nerve L2-L4
3.34.4
Articular Branches
3.34.4.1
To the hip joint
3.34.5
Cutaneous Branches
3.34.5.1
8ee cutaneous branches of tibia and
common peroneal divisions of the sciatic nerve
3.34.6
Lesions
3.34.6.1
Trauma, fractures or posterior dislocations of the hip
(coxal) joint, and attempts to repair them, often damage this nerve. Damage is
common in vehicle accidents with impact to the knees, thus causing the head of
the femur through the acetabulum. More common would be: herniated
intervertebral disc, misplaced injection or Osteoarthritis of spine or
sacroiliac joint. A complete lesion produces total paralysis of the hamstrings
and of all muscles below the knee, with additional weakness to adductor magnus.
A sensory loss will also occur in the distributions of the tibia and common
peroneal nerves leaving only the Saphenous nerve distribution below the knee
joint. A partial lesion of the lateral trunk, i.e.,
the source of the common peroneal nerve, is more common of the two. . Care
must. be taken to distinguish from a focal lesion of the common peroneal
nerves (Note: See lesions for both tibia
and common peroneal nerves).
3.34.7
Path Description
3.34.7.1
The Sciatic (n. ischiadicus; great sciatic nerve) (Fig. 832)
supplies nearly the whole of the skin of the leg, the muscles of the back of
the thigh, and those of the leg and foot. It is the largest nerve in the body,
measuring 2 cm. in breadth, and is the continuation of the flattened band of
the sacral plexus. It passes out of the pelvis through the greater sciatic
foramen, below the Piriformis muscle. It descends between the greater
trochanter of the femur and the tuberosity of the ischium, and along the back
of the thigh to about its lower third, where it divides into two large
branches, the tibial and common peroneal nerves. This division may take place
at any point between the sacral plexus and the lower third of the thigh. When
it occurs at the plexus, the common peroneal nerve usually pierces the
Piriformis.
3.34.7.2
In the upper part of
its course the nerve rests upon the posterior surface of the ischium, the nerve
to the Quadratus femoris, the Obturator internus and Gemelli, and the Quadratus
femoris; it is accompanied by the posterior femoral cutaneous nerve and the
inferior gluteal artery, and is covered by the Glutæus maximus. Lower down, it
lies upon the Adductor magnus, and is crossed obliquely by the long head of the
Biceps femoris.
3.34.7.3
The nerve gives off
articular and muscular branches.
3.34.7.4
The articular
branches (rami articulares) arise from the upper part of the nerve and supply
the hip-joint, perforating the posterior part of its capsule; they are
sometimes derived from the sacral plexus.
3.34.7.5
The muscular
branches (rami musculares) are distributed to the Biceps femoris,
Semitendinosus, Semimembranosus, and Adductor magnus. The nerve to the short
head of the Biceps femoris comes from the common peroneal part of the sciatic,
while the other muscular branches arise from the tibial portion, as may be seen
in those cases where there is a high division of the sciatic nerve.
3.34.8
Gray’s Anatomy
3.34.8.1
http://www.bartleby.com/107/213.html
3.34.8.2
Illustrations
3.34.8.2.1
http://www.bartleby.com/107/illus832.html
3.34.9
Number
3.34.9.1
3.34.10
Reference
3.34.10.1
86
3.34.11
Illustration
3.34.11.1
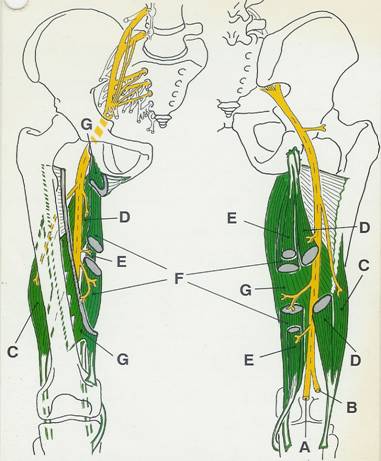
3.35
Tibial Nerve (Branches
Arising between Gastrocnemius Heads) (87)
Back
Table of Contents References
3.35.1
Spinal Roots L4, L5, S1, S2, S3
3.35.1.1
Through the ventral divisions from the lumbar and sacral
ventral rami of the sacral plexus.
3.35.2
Cutaneous Branches
3.35.2.1
A=Medial Cutaneous Sural
Nerve
3.35.2.1.1
Descends
superficially between the heads of the gastrocnemius muscle and is joined by
the lateral sural or communicating branches from the common peroneal nerve;
supplies the posterolateral skin of the distal third of the calf and lateral
side of foot and little toe.
3.35.3
Muscular Branches
3.35.3.1
B=Gastrocnemius,
lateral head / S1, 52.
3.35.3.2
C=Gastrocnemius,
medial head / S1, 52.
3.35.3.3
D=Plantaris /
S1, 52.
3.35.3.4
E=Soleus
/ 51, S2.
3.35.3.5
F=Popliteus / L4,
L5, 51.
3.35.3.6
G=Tibialis
posterior / L4, L5
3.35.3.6.1
From
branch to Popliteus
3.35.4
Articular Branches
3.35.4.1
H=Three branches to
the knee joint (genicular).
3.35.4.2
I=Tibiofibular, interosseous
and distal tibiofibular joints via branches to the Popliteus muscle.
3.35.5
Note
3.35.5.1
See sural and medial calcaneal
branches of the tibial nerve
3.35.6
Lesions
3.35.6.1
Sacral plexus and sciatic nerve injuries usually involve
tibial fibers; distal focal lesions, although rare, are less likely than common
peroneal nerve lesions due to deeper tibial nerve pathway. Trauma is the most
likely etiology of focal tibial paralysis. Presents as weak knee flexion due to
paralysis of the gastrocnemius (a secondary action of this muscle). This action
is saved by the hamstrings. Loss of plantar flexion, and supination of foot due
to paralysis of the posterior compartment musculature of the leg. Peroneus
longus and brevis would be the only muscles left for plantar flexion
(superficial peroneal nerve). Further, there is an inability to flex,
adduct/abduct the toes, due to paralysis of all intrinsic plantar foot muscles
(medial and lateral plantar nerves). Paresthesia or loss of sensation to
plantar nerve distribution would also occur.
3.35.7
Path Description
3.35.7.1
The Tibial Nerve (n. tibialis; internal popliteal nerve)
(Fig. 832) the larger of the two terminal branches of the sciatic, arises from
the anterior branches of the fourth and fifth lumbar and first, second, and
third sacral nerves. It descends along the back of the thigh and through the
middle of the popliteal fossa, to the lower part of the Popliteus muscle, where
it passes with the popliteal artery beneath the arch of the Soleus. It then
runs along the back of the leg with the posterior tibial vessels to the
interval between the medial malleolus and the heel, where it divides beneath
the laciniate ligament into the medial and lateral plantar nerves. In the thigh
it is overlapped by the hamstring muscles above, and then becomes more superficial,
and lies lateral to, and some distance from, the popliteal vessels;opposite the
knee-joint, it is in close relation with these vessels, and crosses to the
medial side of the artery. In the leg it is covered in the upper part of its
course by the muscles of the calf; lower down by the skin, the superficial and
deep fasciæ. It is placed on the deep muscles, and lies at first to the medial
side of the posterior tibial artery, but soon crosses that vessel and descends
on its lateral side as far as the ankle. In the lower third of the leg it runs
parallel with the medial margin of the tendo calcaneus.
3.35.7.2
The branches of this nerve are: articular, muscular, medial
sural cutaneous, medial calcaneal, medial and lateral plantar. 23
3.35.7.3
Articular branches
(rami articulares), usually three in number, supply the knee-joint; two of
these accompany the superior and inferior medial genicular arteries; and a
third, the middle genicular artery. Just above the bifurcation of the nerve an
articular branch is given off to the ankle-joint. 24
3.35.7.4
Muscular branches
(rami musculares), four or five in number, arise from the nerve as it lies
between the two heads of the Gastrocnemius muscle; they supply that muscle, and
the Plantaris, Soleus, and Popliteus. The branch for the Popliteus turns around
the lower border and is distributed to the deep surface of the muscle. Lower
down, muscular branches arise separately or by a common trunk and supply the
Soleus, Tibialis posterior, Flexor digitorum longus, and Flexor hallucis
longus; the branch to the last muscle accompanies the peroneal artery; that to
the Soleus enters the deep surface of the muscle.
3.35.7.5
3.35.8
Gray’s Anatomy
3.35.8.1 http://www.bartleby.com/107/213.html
3.35.8.2 Illustrations
3.35.8.2.1
http://www.bartleby.com/107/illus832.html
3.35.8.2.2
http://www.bartleby.com/107/illus830.html
3.35.8.2.3
http://www.bartleby.com/107/illus831.html
3.35.9
NUMBER
3.35.9.1 35.10
3.35.10
REFERENCE
3.35.10.1
87
3.35.11
Illustration
3.35.11.1
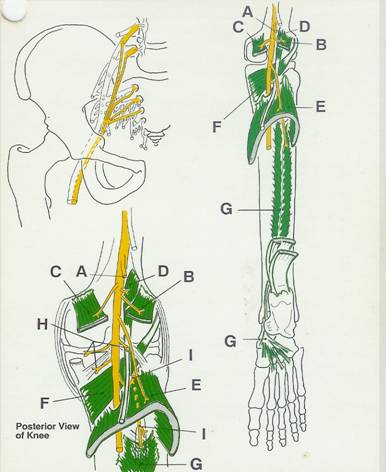 ``
``
3.36
Tibial Nerve
(Branches Arising in the Leg) (88)
3.36.1
Spinal Roots L4, L5, S1, S2, S3
3.36.1.1
Through ventral divisions from the
lumbar and sacral ventral rami of the sacral plexus
3.36.2
Named Branches
3.36.2.1
A=Medial
calcanean nerve
3.36.2.2
B=Medial
plantar nerve
3.36.2.3
C=Lateral
plantar nerve
3.36.2.4
D=Sural
nerve
3.36.2.4.1
Path
Description
3.36.2.4.1.1
The
sural nerve (n. suralis; short saphenous nerve), formed by the
junction of the medial sural cutaneous with the peroneal anastomotic branch,
passes downward near the lateral margin of the tendo calcaneus, lying close to
the small saphenous vein, to the interval between the lateral malleolus and the
calcaneus. It runs forward below the lateral malleolus, and is continued as the
lateral dorsal cutaneous nerve along the lateral side of
the foot and little toe, communicating on the dorsum of the foot with the
intermediate dorsal cutaneous nerve, a branch of the superficial peroneal. In
the leg, its branches communicate with those of the posterior femoral
cutaneous.
3.36.2.4.2
Illustration
3.36.2.4.2.1
http://www.bartleby.com/107/illus831.html
3.36.3
Muscular Branches
3.36.3.1 E=Soleus / S1, S2
3.36.3.1.1
To
it's deep surface.
3.36.3.2 F=Tibialis posterior / L4,
L5
3.36.3.3 G=Flexor digitorum longus / S2, S3
3.36.3.4 H=Flexor
hallucis longus / S2,
S3
3.36.4
Articular Branches
3.36.4.1
:
To the ankle
before it bifurcates as medial and lateral plantar nerves
3.36.5
Cutaneous Branches
3.36.5.1
The medial calcanean nerve supplies
the skin of the heal and medial side of the sole (See also sural and medial
calcanean nerves).
3.36.6
Lesions
3.36.6.1
Injury to the tibial nerve is uncommon due to its deep
location in the calf. A focal lesion would present weakness in plantar flexion.
Plantar flexion is not lost if gastrocnemius is intact. Paralysis of the deep
posterior crural muscles would present weakness in foot inversion; this
movement is saved by the tibialis anterior (deep peroneal nerve). Flexion,
adduction and abduction of toes would be lost due to distal innervation of the
same nerve branches to plantar foot. Patient will be, unable to
stand on tip toes (Note: See also medial and lateral plantar nerves)
3.36.7
Gray’s Anatomy
3.36.7.1
http://www.bartleby.com/107/213.html
3.36.8
NUMBER
3.36.8.1
35.10
3.36.9
REFERENCE
3.36.9.1
88
3.36.10
Illustration
3.36.10.1
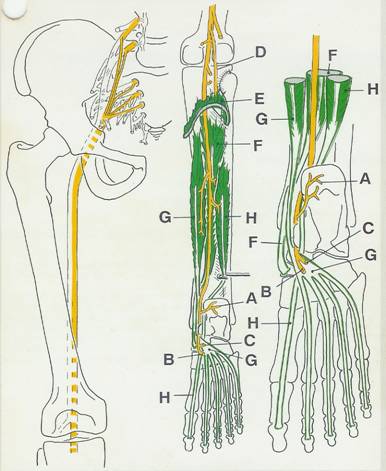
3.37 Tibial Nerve
(Medial Sural and Medial Calcanean Cutaneous Branches) (89)
3.37.1
Spinal Roots
3.37.1.1
L5 S1 S2 (Sural Nerve) S1 S2 (Medial Calcanean Nerve)
3.37.1.1.1
Both
branches are via the ventral divisions from the lumbar and sacral ventral rami
of the sacral plexus through the sciatic nerve as the sural and medial
Calcanean branches of the tibial nerve, respectively
3.37.1.2
NUMBER
3.37.1.2.1
35.101
3.37.1.3
REFERENCE
3.37.1.3.1
89
3.37.2
Muscular Branches
3.37.2.1
None
3.37.3
Articular Branches
3.37.3.1
None
3.37.4
Cutaneous Branches
3.37.4.1 A=Medial Sural Cutaneous Nerve L5 S1 S2
3.37.4.1.1
Descends
superficially between the heads of the gastrocnemius and is joined by the communicating
branch of the lateral sural nerve of common peroneal nerve. Supplies the
posterolateral skin of the distal third of the calf and the lateral side of the
foot and little toe The communicating branch may descend separately, and join
medial sural as far distal as the heel.
3.37.4.2
B=Medial Calcaneal
Nerve S1 S2
3.37.4.2.1
Arises
proximal to the tarsal tunnel, perforating the flexor retinaculum (laciniate
ligament ) to supply the skin of the medial side of the plantar surface of the
foot and heel.
3.37.5
Gray’s Anatomy
3.37.5.1
http://www.bartleby.com/107/213.html
3.37.5.2
Illustration
3.37.5.2.1
http://www.bartleby.com/107/illus832.html
3.37.6
NUMBER
3.37.6.1
35.102
3.37.7
REFERENCE
3.37.7.1
89
3.37.8
Lesions
3.37.8.1
Presents as Paresthesia or loss of sensation to the skin
described above. Testing these areas can help in differential diagnosis of
focal tibial lesions
3.37.9
Illustration
3.37.9.1
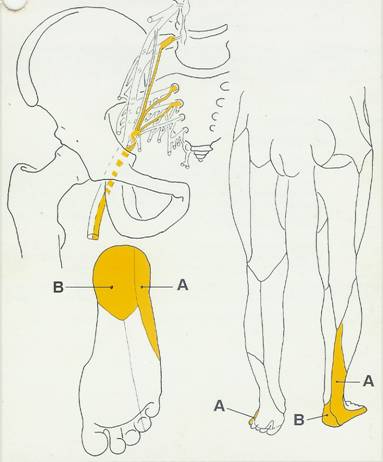
3.38
Medial Plantar
(Tibial) (90)
3.38.1
NUMBER
3.38.1.1
35.103
3.38.2
REFERENCE
3.38.2.1
90
3.38.3
SPINAL ROOTS
3.38.3.1
L4, L5, S1, S2, S3 through ventral divisions from the
ventral sacral rami of the sacral plexus through the sciatic nerve as the
medial terminal branch of the tibial nerve
3.38.4
Named Branches
3.38.4.1
A= Hallucial medial
Digital nerve
3.38.4.2
B=Common Plantar
Digital Nerves
3.38.4.3
C=Proper plantar
digital nerves
3.38.5
Muscular Branches
3.38.5.1
D=Abductor Hallucis
3.38.5.1.1
S2
S3
3.38.5.2
E=Flexor Digitorum
Brevis
3.38.5.2.1
S2
S3
3.38.5.3
F=Flexor Hallucis
Brevis
3.38.5.3.1
S2
S3
3.38.5.3.2
From
the Hallucial medial digital nerve
3.38.5.4
G=1st
Lumbrical
3.38.5.4.1
S2,
S3
3.38.5.4.2
From
the 1st common plantar digital nerve. The rest of the Lumbricals are
supplied by the deep branch of the lateral plantar nerve.
3.38.6
ARTICULAR BRANCHES(MED PLANTAR)
3.38.6.1
To the tarsus and metatarsus. Each proper digital nerve
provides articular branches to it’s respective phalangeal joints
3.38.7
Cutaneous Branches
3.38.7.1
L4 L5 supply the skin of the medial side of the sole of the
foot. Each proper digital nerve provides cutaneous branches to its’s respective
phalanx with a dorsal branch to around the nail. The terminal branches supply
the ball of the toes.
3.38.8
Lesions
3.38.8.1
Tarsal tunnel syndrome (Jogger’s foot)
3.38.8.1.1
Damage
to the tibial nerve within the tarsal tunnel can occur due to external pressure
from foot wear and/or thickened flexor retinaculum.
3.38.8.1.2
Trauma
and dislocations can produce the same results.
3.38.8.1.3
Either
or both plantar nerves can be affected, but usually the medial plantar nerve.
Focal medial plantar nerve injury presents weak toe flexion and inability to
abduct the big toe. Additionally, pain and Paresthesia or loss of sensation to
the skin described above will occur. If sensory loss affects the heel, the
calcaneal sensory nerve is involved, therefore the lesion must be proximal to
the tarsal tunnel.
3.38.9
Path Description
3.38.9.1
The medial plantar nerve (n. plantaris medialis; internal
plantar nerve) (Fig. 833), the larger of the two terminal divisions of the
tibial nerve, accompanies the medial plantar artery. From its origin under the
laciniate ligament it passes under cover of the Abductor hallucis, and,
appearing between this muscle and the Flexor digitorum brevis, gives off a
proper digital plantar nerve and finally divides opposite the bases of the
metatarsal bones into three common digital plantar nerves. 29
3.38.9.2
3.38.9.3
BRANCHES.—The branches of the medial plantar nerve are: (1)
cutaneous, (2) muscular, (3) articular, (4) a proper digital nerve to the
medial side of the great toe, and (5) three common digital nerves. 30
3.38.9.4
The cutaneous
branches pierce the plantar aponeurosis between the Abductor hallucis and the
Flexor digitorum brevis and are distributed to the skin of the sole of the
foot. 31
3.38.9.5
The muscular
branches supply the Abductor hallucis, the Flexor digitorum brevis, the Flexor
hallucis brevis, and the first Lumbricalis; those for the Abductor hallucis and
Flexor digitorum brevis arise from the trunk of the nerve near its origin and
enter the deep surfaces of the muscles; the branch of the Flexor hallucis
brevis springs from the proper digital nerve to the medial side of the great
toe, and that for the first Lumbricalis from the first common digital
nerve. 32
3.38.9.6
The articular
branches supply the articulations of the tarsus and metatarsus. 33
3.38.9.7
The proper digital
nerve of the great toe (nn. digitales plantares proprii; plantar digital branches)
supplies the Flexor hallucis brevis and the skin on the medial side of the
great toe. 34
3.38.9.8
The three common
digital nerves (nn. digitales plantares communes) pass between the divisions of
the plantar aponeurosis, and each splits into two proper digital nerves—those
of the first common digital nerve supply the adjacent sides of the great and
second toes; those of the second, the adjacent sides of the second and third
toes; and those of the third, the adjacent sides of the third and fourth toes.
The third common digital nerve receives a communicating branch from the lateral
plantar nerve; the first gives a twig to the first Lumbricalis. Each proper
digital nerve gives off cutaneous and articular filaments; and opposite the
last phalanx sends upward a dorsal branch, which supplies the structures around
the nail, the continuation of the nerve being distributed to the ball of the
toe. It will be observed that these digital nerves are similar in their
distribution to those of the median nerve in the hand.
3.38.10
Gray’s Anatomy
3.38.10.1
http://www.bartleby.com/107/213.html
3.38.10.2
Illustration
3.38.10.2.1
http://www.bartleby.com/107/illus833.html
3.38.10.2.2
http://www.bartleby.com/107/illus834.html
3.38.11
Illustration
3.38.11.1
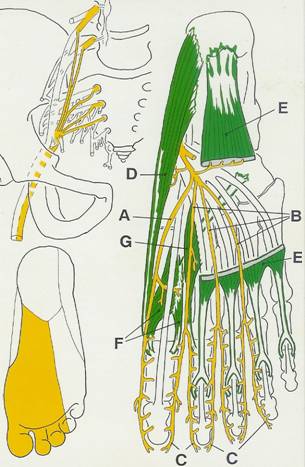
3.39
Lateral Plantar
Nerve & Superficial Branch (Tibial) (91)
3.39.1
NUMBER
3.39.1.1
35.104
3.39.2
REFERENCE
3.39.2.1
91
3.39.3
Spinal Roots
3.39.3.1
L4 L5 S1 S2 S3
3.39.3.2
Through ventral divisions of the sacral plexus through the
sciatic nerve as the lateral terminal branch of the tibial nerve.
3.39.4
Named Branches
3.39.4.1
A=Superficial
Branch
3.39.4.2
B=Deep Branch
3.39.4.3
C=Common Plantar
Digital Nerves
3.39.4.4
D=Proper Plantar
Digital Nerves
3.39.5
Muscular Branches
3.39.5.1
E=Quadratus Plantae
3.39.5.1.1
S2
S3
3.39.5.2
F=Abductor Digiti
Minimi
3.39.5.2.1
S2
S3
3.39.5.3
G=Flexor Digiti
Minimi Brevis
3.39.5.3.1
S2
S3
3.39.5.4
H=The 3rd
Plantar interosseous Muscle
3.39.5.4.1
S2
S3
3.39.5.5
I=The 4th
Dorsal Interosseous Muscle
3.39.5.5.1
S2
S3
3.39.6
Articular Branches
3.39.6.1
To the metatarsophalangeal and Interphalangeal joints of the
4th and 5th digits
3.39.7
Cutaneous Branches
3.39.7.1
S1, S2 supplies the dkin of the lateral part of the sole
3.39.7.2
Common and proper plantar digital nerves supply the plantar
skin on the lateral side of the 4th and both sides of the 5th
digit
3.39.8
Lesions
3.39.8.1
Focal lateral plantar nerve injury presents an inability to
abduct the 4th and 5th digits due to paralysis of the
abductor digiti minimi and the 4th dorsal interosseous muscle,
respectively. A slight weakness on flexion of the small toe due to paralysis to
flexor digiti minimi brevis and quadratus plantae. Loss of quadratus plantae
may affect flexion of the 2nd, 3rd, and 4th
toes. Paresthesia or loss of sensation to the skin described above also occurs.
3.39.9
Path Description
3.39.9.1
The Lateral Plantar Nerve (n. plantaris lateralis; external
plantar nerve) (Fig. 833) supplies the skin of the fifth toe and lateral half
of the fourth, as well as most of the deep muscles, its distribution being
similar to that of the ulnar nerve in the hand. It passes obliquely forward
with the lateral plantar artery to the lateral side of the foot, lying between
the Flexor digitorum brevis and Quadratus plantæ and, in the interval between
the former muscle and the Abductor digiti quinti, divides into a superficial
and a deep branch. Before its division, it supplies the Quadratus plantæ and
Abductor digiti quinti. 36
3.39.9.2
The superficial
branch (ramus superficialis) splits into a proper and a common digital nerve;
the proper digital nerve supplies the lateral side of the little toe, the
Flexor digiti quinti brevis, and the two Interossei of the fourth
intermetatarsal space; the common digital nerve communicates with the third
common digital branch of the medial plantar nerve and divides into two proper
digital nerves which supply the adjoining sides of the fourth and fifth toes.
3.39.10
Gray’s Anatomy
3.39.10.1
http://www.bartleby.com/107/213.html
3.39.10.2
Illustration
3.39.10.2.1
http://www.bartleby.com/107/illus833.html
3.39.10.2.2
http://www.bartleby.com/107/illus834.html
3.39.11
Illustration
3.39.11.1
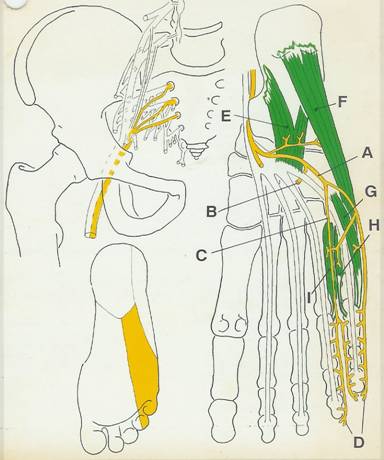
3.40 Lateral Plantar
Nerve Deep Branch (Tibial) (92)
3.40.1
NUMBER
3.40.2
REFERENCE
3.40.2.1
92
3.40.3
Spinal Roots
3.40.3.1
S2 S3
3.40.3.2
Through ventral divisions from the sacral rami of the sacral
plexus through the sciatic nerve as the deep branch fo the lateral terminal
branch of the tibial nerve
3.40.4
Muscular Branches
3.40.4.1
A=Adductor Hallucis
(Oblique Head)
3.40.4.1.1
S2
S3
3.40.4.2
B=Adductor Hallucis (Transverse Head)
3.40.4.2.1
S2
S3
3.40.4.3
C=1st
and 2nd Plantar Interossei
3.40.4.3.1
S2
S3
3.40.4.4
D=1st, 2nd,
and 3rd Lumbricals
3.40.4.4.1
S2
S3
3.40.4.5
E=1st, 2nd,
and 3rd Dorsal Interossei
3.40.4.5.1
S2
S3
3.40.4.6
Note
3.40.4.6.1
The
4th dorsal interosseous and 3rd plantar interosseous,
those of the 4th Intermetatarsal space and the 4th
Lumbricals, are supplied by the superficial branch of the lateral plantar
nerve. The 1st and 2nd dorsal Interossei may receive
supply from the deep peroneal nerve also
3.40.5
Articular Branches
3.40.5.1
To the plantar Intermetatarsal and tarsometatarsal joints
3.40.6
Cutaneous Branches
3.40.6.1
None
3.40.7
Lesions
3.40.7.1
A focal injury to this nerve would be uncommon. In tarsal
tunnel syndrome, the nerve compression could relate to these fibers only.
Presents as a loss of adduction of the big toe. Loss of innervation to
Lumbricals and Interossei may cause weakness in flexion of proximal phalanx of
2nd, 3rd and 4th toes. In addition, weakness
in abduction (dorsal Interossei) and adduction (plantar Interossei) of toes.
3.40.8
Path Description
3.40.8.1
The deep branch (ramus profundus; muscular branch)
accompanies the lateral plantar artery on the deep surface of the tendons of
the Flexor muscles and the Adductor hallucis, and supplies all the Interossei
(except those in the fourth metatarsal space), the second, third, and fourth
Lumbricales, and the Adductor hallucis.
3.40.9
Gray’s Anatomy
3.40.9.1
http://www.bartleby.com/107/213.html
3.40.9.2
Illustration
3.40.9.2.1
http://www.bartleby.com/107/illus833.html
3.40.9.2.2
http://www.bartleby.com/107/illus834.html
3.40.10
Illustration
3.40.10.1
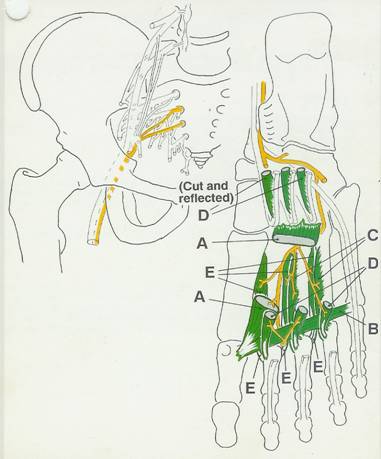
3.41
Common Peroneal
(Fibular) Nerve (93)
Back
Table of Contents References
3.41.1
Spinal Roots
3.41.1.1
L4, L5, S1, S2
3.41.1.1.1
Through dorsal divisions from the
lumbar and sacral ventral rami of the sacral plexus as the fibular division of
the sciatic nerve
3.41.2
Named Branches
3.41.2.1
A=Deep peroneal
(anterior tibial) nerve,
3.41.2.2
B=Superficial
peroneal (musculocutaneous) nerve
3.41.3
Muscular Branches
3.41.3.1
None
3.41.4
Articular Branches
3.41.4.1
Three branches to the anterolateral
part of the knee capsule and the proximal tibiofibular joint that pass with the
following arteries
3.41.4.1.1
C=Superior
lateral
genicular artery
3.41.4.1.2
D=Lateral
genicular artery
3.41.4.1.3
E=Anterior
tibial recurrent arter,y
3.41.5
Cutaneous Branches
3.41.5.1
F=Lateral Sural
Nerve
3.41.5.1.1
Summary
3.41.5.1.1.1
The lateral sural nerve (lateral
cutaneous nerve of the
calf, L4, L5, S1) supplies the skin of the anterior, lateral, and
posterior aspects of the proximal leg. A communicating branch arises and
connects with the medial sural nerve of the tibial to form sural and continues
to distribute to lateral foot
3.41.5.2
The lateral sural cutaneous nerve (n. cutaneus suræ
lateralis; lateral cutaneous branch) supplies the skin on the posterior and lateral
surfaces of the leg; one branch, the peroneal anastomotic (n. communicans
fibularis), arises near the head of the fibula, crosses the lateral head of the
Gastrocnemius to the middle of the leg, and joins with the medial sural
cutaneous to form the sural nerve. The peroneal anastomotic is occasionally
continued down as a separate branch as far as the heel.
3.41.6
Lesions
3.41.6.1
: This is the most commonly injured
nerve in the lower leg. Primary causes are from direct impact, especially at
the fibular head, or by fractures of the fibula and compression from prolonged
kneeling or sitting with legs crossed. Sacral plexus and sciatic nerve lesions
frequently affect the common peroneal nerve. Focal lesion to this nerve would
produce paresthesia or loss of sensation to the skin described above
3.41.7
Note
3.41.7.1
See deep peroneal
and superficial peroneal nerves
3.41.8
Path Description
3.41.8.1
The Common Peroneal Nerve (n. peronæus communis; external
popliteal nerve; peroneal nerve) (Fig. 832), about one-half the size of the
tibial, is derived from the dorsal branches of the fourth and fifth lumbar and
the first and second sacral nerves. It descends obliquely along the lateral
side of the popliteal fossa to the head of the fibula, close to the medial
margin of the Biceps femoris muscle. It lies between the tendon of the Biceps
femoris and lateral head of the Gastrocnemius muscle, winds around the neck of
the fibula, between the Peronæus longus and the bone, and divides beneath the
muscle into the superficial and deep peroneal nerves. Previous to its division
it gives off articular and lateral sural cutaneous nerves. 39
3.41.8.2
The articular
branches (rami articulares) are three in number; two of these accompany the
superior and inferior lateral genicular arteries to the knee; the upper one
occasionally arises from the trunk of the sciatic nerve. The third (recurrent)
articular nerve is given off at the point of division of the common peroneal
nerve; it ascends with the anterior recurrent tibial artery through the
Tibialis anterior to the front of the knee.
3.41.9
Gray’s Anatomy
3.41.9.1
http://www.bartleby.com/107/213.html
3.41.9.2
Illustrations
3.41.9.2.1
http://www.bartleby.com/107/illus832.html
3.41.10
Number
3.41.10.1
35.09
3.41.11
Reference
3.41.11.1
93
3.41.12
Illustration
3.41.12.1
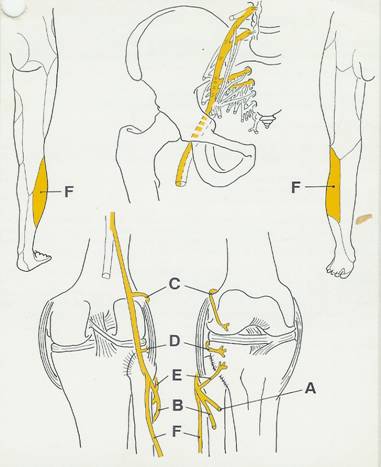
3.42
Deep Peroneal
(Anterior Tibial) Nerve (Branches Arising in the Leg) (94)
3.42.1
Spinal Roots
3.42.1.1
L4, LS, S1, S2
3.42.1.1.1
Through dorsal divisions of the
sacral plexus through the sciatic nerve; branches within the peroneus longus
muscle (not illustrated) into deep and superficial peroneal nerve
3.42.2
Named Branches
3.42.2.1
A=Superficial
peroneal nerve
3.42.2.2
B=Lateral
terminal branch
3.42.2.3
C=Medial
terminal branch
3.42.3
Muscular Branches
3.42.3.1 D=Tibialis Anterior / L4,
L5,
3.42.3.2
E=Extensor
hallucis longus / LS,
S 1,
3.42.3.3
F=Extensor
digitorum longus / LS,
S 1,
3.42.3.4
G=Peroneus
Tertius / LS, S1
3.42.4
Articular Branches
3.42.4.1
To the Talocrural joint
3.42.5
Cutaneous Branches
3.42.5.1
None
3.42.6
Lesions
3.42.6.1
Focal lesions to this nerve are
usually caused by trauma. The superficial peroneal would most likely be
affected. Injury would present "drop foot inability to dorsiflex and weak
eversion at the subtalar and intertarsal joints. The action is saved if
peroneus longus muscle and superficial peroneal nerve survive.
3.42.7
Path Description
3.42.7.1
The Deep Peroneal Nerve (n. peronæus profundus; anterior
tibial nerve) (Fig. 827) begins at the bifurcation of the common peroneal
nerve, between the fibula and upper part of the Peronæus longus, passes
obliquely forward beneath the Extensor digitorum longus to the front of the
interosseous membrane, and comes into relation with the anterior tibial artery
above the middle of the leg; it then descends with the artery to the front of
the ankle-joint, where it divides into a lateral and a medial terminal branch.
It lies at first on the lateral side of the anterior tibial artery, then in
front of it, and again on its lateral side at the ankle-joint. 42
3.42.7.2
In the leg, the deep
peroneal nerve supplies muscular branches to the Tibialis anterior, Extensor
digitorum longus, Peronæus tertius, and Extensor hallucis prop ius, and an
articular branch to the ankle-joint.
43
3.42.7.3
The lateral terminal
branch (external or tarsal branch) passes across the tarsus, beneath the
Extensor digitorum brevis, and, having become enlarged like the dorsal
interosseous nerve at the wrist, supplies the Extensor digitorumbrevis. From
the enlargement three minute interosseous branches are given off, which supply
the tarsal joints and the metatarsophalangeal joints of the second, third, and
fourth toes. The first of these sends a filament to the second Interosseus
dorsalis muscle.
3.42.7.4
The medial terminal
branch (internal branch) accompanies the dorsalis pedis artery along the dorsum
of the foot, and, at the first interosseous space, divides into two dorsal
digital nerves (nn. digitales dorsales hallucis lateralis et digiti secundi
medialis) which supply the adjacent sides of the great and second toes,
communicating with the medial dorsal cutaneous branch of the superficial
peroneal nerve. Before it divides it gives off to the first space an
interosseous branch which supplies the metatarsophalangeal joint of the great
toe and sends a filament to the first Interosseous dorsalis muscle.
3.42.8
Gray’s Anatomy
3.42.8.1
http://www.bartleby.com/107/213.html
3.42.8.2
Illustration
3.42.8.2.1
http://www.bartleby.com/107/illus827.html
3.42.8.2.2
http://www.bartleby.com/107/illus835.html
3.42.8.2.3
http://www.bartleby.com/107/illus836.html
3.42.9
Number
3.42.9.1
35.092
3.42.10
Reference
3.42.10.1
94
3.42.11
Illustration
3.42.11.1
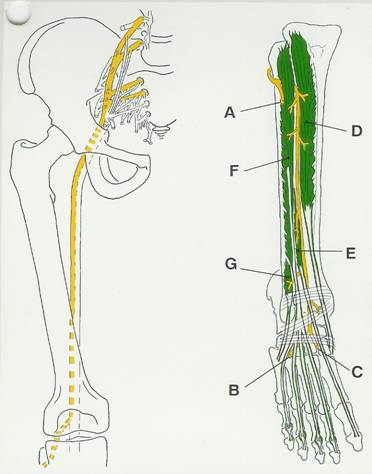
3.43 Deep Peroneal
Medial and Lateral Terminal Branches (95)
3.43.1
Spinal Roots
3.43.1.1
S1, S2
3.43.1.1.1
Through dorsal divisions from the
lumbar and sacral ventral rami of the sacral plexus, through the sciatic and
common peroneal and branches of the deep peroneal nerves
3.43.2
Named Branches
3.43.2.1
3.43.3
Muscular Branches
3.43.3.1
A=1st Dorsal
interosseus muscle / S1, S2
3.43.3.2
B=Extensor
digitorum brevis / S1, S 2
3.43.3.3
C=Extensor hallucis
brevis / S1, S2
3.43.3.4
D=2nd
Dorsal interosseous muscle / S1, S2
3.43.4
Articular Branches
3.43.4.1
E=Medial terminal
branch: To
the hallucial metatarsophalangeal joints.
3.43.4.2
F=Lateral
terminal branch: By three interosseous branches to
the tarsal and metatarsophalangeal joints of the middle three toes.
3.43.5
Cutaneous Branches
3.43.5.1
From the medial terminal branch there
are two dorsal digital nerves supplying the adjacent sides of the big and
second toe (1st interdigital cleft)
3.43.6
Lesions
3.43.6.1
The terminal branches may be injured
where they cross the ankle and on the dorsum of the foot by trauma, ankle
fractures, dislocations and sprains. Spontaneous entrapment beneath the
inferior extensor retinaculum has been termed anterior tarsal tunnel syndrome.
This focal lesion can go undetected, the cutaneous distribution being so small
and the extensor action of the toe musculature minimal.
3.43.7
Gray’s Anatomy
3.43.7.1
http://www.bartleby.com/107/213.html
3.43.8
Number
3.43.8.1
35.0921
3.43.9
Reference
3.43.9.1
95
3.43.10
Illustration
3.43.10.1
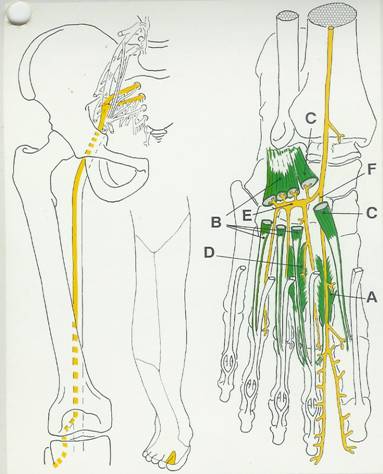
3.44
Superficial
Peroneal Nerve (96)
3.44.1
Spinal Roots
3.44.1.1
L5, S1, S2
3.44.1.1.1
Through dorsal divisions from lumbar
and sacral ventral rami of the sacral plexus, through the sciatic nerve and
branching superficial from the deep peroneal nerve
3.44.2
Named Branches
3.44.2.1
A=Medial
branch
3.44.2.2
B=Lateral
branch
3.44.3
Muscular Branches
3.44.3.1
C=Peroneus
Longus L5,
S1, S2
3.44.3.2
D=Peroneus brevis
L5, S1, S2.
3.44.4
Articular Branches
3.44.4.1
None
3.44.5
Cutaneous Branches
3.44.5.1
None
3.44.5.2
Note
3.44.5.2.1
See medial and lateral branches of superficial
peroneal nerve
3.44.6
Lesions
3.44.6.1
Focal lesions to this nerve are common because of its
superficial location. However, the common peroneal is more vulnerable and
likely .to be damaged, affecting both deep and superficial peroneal nerves.
Focal lesions will present an inverted foot by the unopposed action of the deep
crural muscle group (tibia innervation). Weakness in eversion of the subtalar
and intertarsal joints. This action is saved by the extensor digitorum longus,
and is present if peroneus Tertius survives.
3.44.7
Path Description
3.44.7.1
The Superficial Peroneal Nerve (n. peronæus superficialis;
musculocutaneous nerve) (Figs. 827, 835) supplies the Peronei longus and brevis
and the skin over the greater part of the dorsum of the foot. It passes forward
between the Peronæi and the Extensor digitorum longus, pierces the deep fascia
at the lower third of the leg, and divides into a medial and an intermediate
dorsal cutaneous nerve. In its course between the muscles, the nerve gives off
muscular branches to the Peronæi longus and brevis, and cutaneous filaments to
the integument of the lower part of the leg.
3.44.8
Gray’s Anatomy
3.44.8.1
http://www.bartleby.com/107/213.html
3.44.8.2
Illustrations
3.44.8.2.1
http://www.bartleby.com/107/illus827.html
3.44.8.2.2
http://www.bartleby.com/107/illus835.html
3.44.8.2.3
http://www.bartleby.com/107/illus836.html
3.44.9
Number
3.44.9.1
35.093
3.44.10
Reference
3.44.10.1
96
3.44.11
Illustration
3.44.11.1
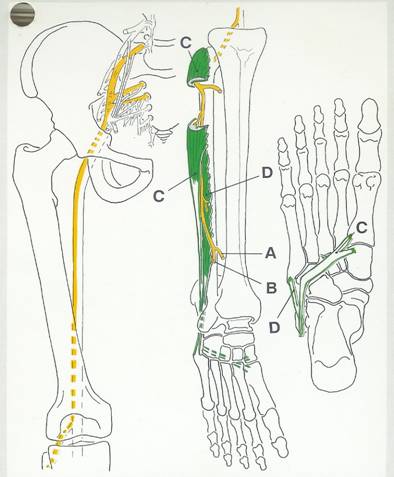
3.45 Superficial
Peroneal Nerve Medial and Lateral Terminal Branches (97)
3.45.1
Spinal Roots
3.45.1.1
L4, L5, S1
3.45.1.1.1
Through dorsal divisions from lumbar
and sacral ventral rami of the sacral plexus, through the sciatic, the common
peroneal and bifurcating from the superficial peroneal nerve
3.45.2
Named Branches
3.45.2.1
A=Medial
branch
3.45.2.2
B=Lateral
branch
3.45.2.3
C=Dorsal
digital branches
3.45.3
Muscular Branches
3.45.3.1
None
3.45.4
Articular Branches
3.45.4.1
None
3.45.5
Cutaneous Branches
3.45.5.1
Medial branch
3.45.5.1.1
To
the skin of
the anterior central lower leg, ankle and foot then dividing into dorsal
digital nerves to supply the medial side of the big toe and the adjacent sides
of the second and third toes
3.45.5.2
Lateral
branch
3.45.5.2.1
To the skin of the anterolateral
lower leg, ankle and foot. It then
divides into dorsal digital nerves to supply the medial side of the big toe and
the adjacent sides of the third and forth, and forth and fifth toes.
3.45.6
Lesions
3.45.6.1
Focal lesions distal to the muscular
branches of the superficial peroneal nerve would result in paresthesias to the
skin areas described above. Either or both medial and lateral branches may be
subject to trauma.
3.45.7
Path Description
3.45.7.1
The medial dorsal cutaneous nerve (n. cutaneus dorsalis
medialis; internal dorsal cutaneous branch) passes in front of the ankle-joint,
and divides into two dorsal digital branches, one of which supplies the medial
side of the great toe, the other, the adjacent side of the second and third
toes. It also supplies the integument of the medial side of the foot and ankle,
and communicates with the saphenous nerve, and with the deep peroneal nerve
(Fig. 825). 47
3.45.7.2
The intermediate
dorsal cutaneous nerve (n. cutaneus dorsalis intermedius; external dorsal
cutaneous branch), the smaller, passes along the lateral part of the dorsum of
the foot, and divides into dorsal digital branches, which supply the contiguous
sides of the third and fourth, and of the fourth and fifth toes. It also
supplies the skin of the lateral side of the foot and ankle, and communicates
with the sural nerve (Fig. 825). The branches of the superficial peroneal nerve
supply the skin of the dorsal surfaces of all the toes excepting the lateral
side of the little toe, and the adjoining sides of the great and second toes,
the former being supplied by the lateral dorsal cutaneous nerve from the sural
nerve, and the latter by the medial branch of the deep peroneal nerve.
Frequently some of the lateral branches of the superficial peroneal are absent,
and their places are then taken by branches of the sural nerve.
3.45.8
Gray’s Anatomy
3.45.8.1
http://www.bartleby.com/107/213.html
3.45.8.2
Illustration
3.45.8.2.1
http://www.bartleby.com/107/illus825.html
3.45.9
Number
3.45.9.1
35.0931 & 35.0932
3.45.10
Reference
3.45.10.1
97
3.45.11
Illustration
3.45.11.1
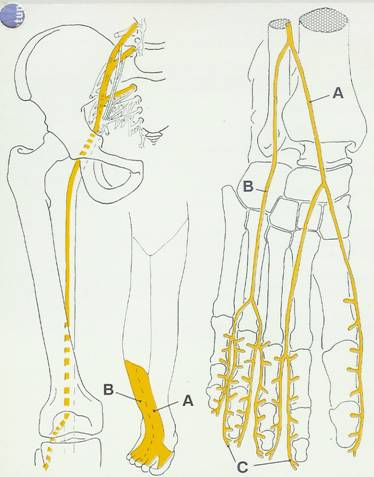
3.46 Perforating
Cutaneous Nerve (98) (Blank)
Back
Table of Contents References
3.46.1
Spinal Roots
3.46.1.1
3.46.2
Named Branches
3.46.2.1
3.46.3
Muscular Branches
3.46.3.1
3.46.4
Articular Branches
3.46.4.1
3.46.5
Cutaneous Branches
3.46.5.1
3.46.6
Lesions
3.46.6.1
3.46.7
Gray’s Anatomy
3.46.7.1
http://www.bartleby.com/107/213.html
3.46.8
Number
3.46.8.1
35
3.46.9
Reference
3.46.9.1
3.46.10
Illustration
3.46.10.1
3.47 Sacral Muscular
Branches (4th Sacral) (99) (Blank)
Back
Table of Contents References
3.47.1
Spinal Roots
3.47.1.1
3.47.2
Named Branches
3.47.2.1
3.47.3
Muscular Branches
3.47.3.1
3.47.4
Articular Branches
3.47.4.1
3.47.5
Cutaneous Branches
3.47.5.1
3.47.6
Lesions
3.47.6.1
3.47.7
Gray’s Anatomy
3.47.7.1
http://www.bartleby.com/107/213.html
3.47.8
Number
3.47.8.1
35
3.47.9
Reference
3.47.9.1
3.47.10
Illustration
3.47.10.1
3.48 Pudendal Nerve:
Inferior Rectal Branch (Inferior Hemeorrhoidal Nerve) (100) (Blank)
Back
Table of Contents References
3.48.1
Spinal Roots
3.48.1.1
3.48.2
Named Branches
3.48.2.1
3.48.3
Muscular Branches
3.48.3.1
3.48.4
Articular Branches
3.48.4.1
3.48.5
Cutaneous Branches
3.48.5.1
3.48.6
Lesions
3.48.6.1
3.48.7
Gray’s Anatomy
3.48.7.1
http://www.bartleby.com/107/213.html
3.48.8
Number
3.48.8.1
35
3.48.9
Reference
3.48.9.1
3.48.10
Illustration
3.48.10.1
3.49 Pudendal Nerve
(Perineal Branch) (101) (Blank)
Back
Table of Contents References
3.49.1
Spinal Roots
3.49.1.1
3.49.2
Named Branches
3.49.2.1
3.49.3
Muscular Branches
3.49.3.1
3.49.4
Articular Branches
3.49.4.1
3.49.5
Cutaneous Branches
3.49.5.1
3.49.6
Lesions
3.49.6.1
3.49.7
Gray’s Anatomy
3.49.7.1
http://www.bartleby.com/107/213.html
3.49.8
Number
3.49.8.1
3.49.9
Reference
3.49.9.1
3.49.10
Illustration
3.49.10.1
3.50 Pudendal Nerve
(Dorsal Nerve of Penis or Clitoris) (102) (Blank)
Back
Table of Contents References
3.50.1
Spinal Roots
3.50.1.1
3.50.2
Named Branches
3.50.2.1
3.50.3
Muscular Branches
3.50.3.1
3.50.4
Articular Branches
3.50.4.1
3.50.5
Cutaneous Branches
3.50.5.1
3.50.6
Lesions
3.50.6.1
3.50.7
Gray’s Anatomy
3.50.7.1
http://www.bartleby.com/107/213.html
3.50.8
Number
3.50.8.1
3.50.9
Reference
3.50.9.1
3.50.10
Illustration
3.50.10.1
3.51 Blank
3.51.1
Spinal Roots
3.51.1.1
3.51.2
Named Branches
3.51.2.1
3.51.3
Muscular Branches
3.51.3.1
3.51.4
Articular Branches
3.51.4.1
3.51.5
Cutaneous Branches
3.51.5.1
3.51.6
Lesions
3.51.6.1
3.51.7
Number
3.51.7.1
3.51.8
Reference
3.51.8.1
3.51.9
Illustration
3.51.9.1
4 TORSO
4.1 LATERAL PECTORAL
Back
Table of Contents References
4.1.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
4.1.1.1
.
4.1.2 NUMBER
4.1.2.1
35
4.1.3 REFERENCE
4.1.3.1
4.1.4 ROOTS
4.1.4.1
4.1.4.2
Lumbar Plexus
4.1.4.3
VENTRAL
4.1.5 DIVISION
4.1.5.1
Dorsal Ventral
4.1.5.2
4.1.6 CUTANEOUS BRANCHES
4.1.6.1
4.1.6.1.1
4.1.6.2
4.1.6.2.1
.
4.1.7 ARTICULAR BRANCHES
4.1.7.1
4.1.7.1.1
4.1.8 MUSCULAR BRANCHES
4.1.8.1
4.1.8.2
4.1.8.3
4.1.8.4
4.1.8.5
4.1.8.6
4.2 MEDIAL PECTORAL
Back
Table of Contents References
4.2.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
4.2.1.1
.
4.2.2 NUMBER
4.2.2.1
35
4.2.3 REFERENCE
4.2.3.1
4.2.4 ROOTS
4.2.4.1
4.2.4.2
Lumbar Plexus
4.2.4.3
VENTRAL
4.2.5 DIVISION
4.2.5.1
Dorsal Ventral
4.2.5.2
4.2.6 CUTANEOUS BRANCHES
4.2.6.1
4.2.6.1.1
4.2.6.2
4.2.6.2.1
.
4.2.7 ARTICULAR BRANCHES
4.2.7.1
4.2.7.1.1
4.2.8 MUSCULAR BRANCHES
4.2.8.1
4.2.8.2
4.2.8.3
4.2.8.4
4.2.8.5
4.2.8.6
4.3 1ST THOR INTERCSTL
N
Back
Table of Contents References
4.3.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
4.3.1.1
.
4.3.2 NUMBER
4.3.2.1
35
4.3.3 REFERENCE
4.3.3.1
4.3.4 ROOTS
4.3.4.1
4.3.4.2
Lumbar Plexus
4.3.4.3
VENTRAL
4.3.5 DIVISION
4.3.5.1
Dorsal Ventral
4.3.5.2
4.3.6 CUTANEOUS BRANCHES
4.3.6.1
4.3.6.1.1
4.3.6.2
4.3.6.2.1
.
4.3.7 ARTICULAR BRANCHES
4.3.7.1
4.3.7.1.1
4.3.8 MUSCULAR BRANCHES
4.3.8.1
4.3.8.2
4.3.8.3
4.3.8.4
4.3.8.5
4.3.8.6
4.4 2ND THOR INTRCSTL
N
Back
Table of Contents References
4.4.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
4.4.1.1
.
4.4.2 NUMBER
4.4.2.1
35
4.4.3 REFERENCE
4.4.3.1
4.4.4 ROOTS
4.4.4.1
4.4.4.2
Lumbar Plexus
4.4.4.3
VENTRAL
4.4.5 DIVISION
4.4.5.1
Dorsal Ventral
4.4.5.2
4.4.6 CUTANEOUS BRANCHES
4.4.6.1
4.4.6.1.1
4.4.6.2
4.4.6.2.1
.
4.4.7 ARTICULAR BRANCHES
4.4.7.1
4.4.7.1.1
4.4.8 MUSCULAR BRANCHES
4.4.8.1
4.4.8.2
4.4.8.3
4.4.8.4
4.4.8.5
4.4.8.6
4.5 UPPER
INTERCSTL=T3-6
Back
Table of Contents References
4.5.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
4.5.1.1
.
4.5.2 NUMBER
4.5.2.1
35
4.5.3 REFERENCE
4.5.3.1
4.5.4 ROOTS
4.5.4.1
4.5.4.2
Lumbar Plexus
4.5.4.3
VENTRAL
4.5.5 DIVISION
4.5.5.1
Dorsal Ventral
4.5.5.2
4.5.6 CUTANEOUS BRANCHES
4.5.6.1
4.5.6.1.1
4.5.6.2
4.5.6.2.1
.
4.5.7 ARTICULAR BRANCHES
4.5.7.1
4.5.7.1.1
4.5.8 MUSCULAR BRANCHES
4.5.8.1
4.5.8.2
4.5.8.3
4.5.8.4
4.5.8.5
4.5.8.6
4.6 LWR INTCSTL
N.=T7-11
Back
Table of Contents References
4.6.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
4.6.1.1
.
4.6.2 NUMBER
4.6.2.1
35
4.6.3 REFERENCE
4.6.3.1
4.6.4 ROOTS
4.6.4.1
4.6.4.2
Lumbar Plexus
4.6.4.3
VENTRAL
4.6.5 DIVISION
4.6.5.1
Dorsal Ventral
4.6.5.2
4.6.6 CUTANEOUS BRANCHES
4.6.6.1
4.6.6.1.1
4.6.6.2
4.6.6.2.1
.
4.6.7 ARTICULAR BRANCHES
4.6.7.1
4.6.7.1.1
4.6.8 MUSCULAR BRANCHES
4.6.8.1
4.6.8.2
4.6.8.3
4.6.8.4
4.6.8.5
4.6.8.6
4.7 1ST DORSAL
RAMUS(SUBOCCIPITAL N)
Back
Table of Contents References
4.7.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
4.7.1.1
.
4.7.2 NUMBER
4.7.2.1
35
4.7.3 REFERENCE
4.7.3.1
4.7.4 ROOTS
4.7.4.1
4.7.4.2
Lumbar Plexus
4.7.4.3
VENTRAL
4.7.5 DIVISION
4.7.5.1
Dorsal Ventral
4.7.5.2
4.7.6 CUTANEOUS BRANCHES
4.7.6.1
4.7.6.1.1
4.7.6.2
4.7.6.2.1
.
4.7.7 ARTICULAR BRANCHES
4.7.7.1
4.7.7.1.1
4.7.8 MUSCULAR BRANCHES
4.7.8.1
4.7.8.2
4.7.8.3
4.7.8.4
4.7.8.5
4.7.8.6
4.8 2ND DOR
RAMUS(GREATER OCCIPITAL N)
Back
Table of Contents References
4.8.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
4.8.1.1
.
4.8.2 NUMBER
4.8.2.1
35
4.8.3 REFERENCE
4.8.3.1
4.8.4 ROOTS
4.8.4.1
4.8.4.2
Lumbar Plexus
4.8.4.3
VENTRAL
4.8.5 DIVISION
4.8.5.1
Dorsal Ventral
4.8.5.2
4.8.6 CUTANEOUS BRANCHES
4.8.6.1
4.8.6.1.1
4.8.6.2
4.8.6.2.1
.
4.8.7 ARTICULAR BRANCHES
4.8.7.1
4.8.7.1.1
4.8.8 MUSCULAR BRANCHES
4.8.8.1
4.8.8.2
4.8.8.3
4.8.8.4
4.8.8.5
4.8.8.6
4.9 3RD DORSAL RAMUS
Back
Table of Contents References
4.9.1 DESCRIPTION: PATH, FUNCTION, LESIONS, CUTANEOUS AREA, AND
ADDITIONAL COMMENTS
4.9.1.1
.
4.9.2 NUMBER
4.9.2.1
35
4.9.3 REFERENCE
4.9.3.1
4.9.4 ROOTS
4.9.4.1
4.9.4.2
Lumbar Plexus
4.9.4.3
VENTRAL
4.9.5 DIVISION
4.9.5.1
Dorsal Ventral
4.9.5.2
4.9.6 CUTANEOUS BRANCHES
4.9.6.1
4.9.6.1.1
4.9.6.2
4.9.6.2.1
.
4.9.7 ARTICULAR BRANCHES
4.9.7.1
4.9.7.1.1
4.9.8 MUSCULAR BRANCHES
4.9.8.1
4.9.8.2
4.9.8.3
4.9.8.4
4.9.8.5
4.9.8.6
4.10 LOWR CER DOR RAM
(C4-8)
Back
Table of Contents References
4.10.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
4.10.1.1
.
4.10.2
NUMBER
4.10.2.1
35
4.10.3
REFERENCE
4.10.3.1
4.10.4
ROOTS
4.10.4.1
4.10.4.2
Lumbar Plexus
4.10.4.3
VENTRAL
4.10.5
DIVISION
4.10.5.1
Dorsal Ventral
4.10.5.2
4.10.6
CUTANEOUS BRANCHES
4.10.6.1
4.10.6.1.1
4.10.6.2
4.10.6.2.1
.
4.10.7
ARTICULAR BRANCHES
4.10.7.1
4.10.7.1.1
4.10.8
MUSCULAR BRANCHES
4.10.8.1
4.10.8.2
4.10.8.3
4.10.8.4
4.10.8.5
4.10.8.6
4.11 UPP THOR DOR RAM
(T1-6)
Back
Table of Contents References
4.11.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
4.11.1.1
.
4.11.2
NUMBER
4.11.2.1
35
4.11.3
REFERENCE
4.11.3.1
4.11.4
ROOTS
4.11.4.1
4.11.4.2
Lumbar Plexus
4.11.4.3
VENTRAL
4.11.5
DIVISION
4.11.5.1
Dorsal Ventral
4.11.5.2
4.11.6
CUTANEOUS BRANCHES
4.11.6.1
4.11.6.1.1
4.11.6.2
4.11.6.2.1
.
4.11.7
ARTICULAR BRANCHES
4.11.7.1
4.11.7.1.1
4.11.8
MUSCULAR BRANCHES
4.11.8.1
4.11.8.2
4.11.8.3
4.11.8.4
4.11.8.5
4.11.8.6
4.12 LOWR THOR DOR RAM
(T7-12)
Back
Table of Contents References
4.12.1
DESCRIPTION: PATH, FUNCTION,
LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
4.12.1.1
.
4.12.2
NUMBER
4.12.2.1
35
4.12.3
REFERENCE
4.12.3.1
4.12.4
ROOTS
4.12.4.1
4.12.4.2
Lumbar Plexus
4.12.4.3
VENTRAL
4.12.5
DIVISION
4.12.5.1
Dorsal Ventral
4.12.5.2
4.12.6
CUTANEOUS BRANCHES
4.12.6.1
4.12.6.1.1
4.12.6.2
4.12.6.2.1
.
4.12.7
ARTICULAR BRANCHES
4.12.7.1
4.12.7.1.1
4.12.8
MUSCULAR BRANCHES
4.12.8.1
4.12.8.2
4.12.8.3
4.12.8.4
4.12.8.5
4.12.8.6
4.13 LUMBAR DOR RAM
(L1-5)
Back
Table of Contents References
4.13.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
4.13.1.1
.
4.13.2
NUMBER
4.13.2.1
35
4.13.3
REFERENCE
4.13.3.1
4.13.4
ROOTS
4.13.4.1
4.13.4.2
Lumbar Plexus
4.13.4.3
VENTRAL
4.13.5
DIVISION
4.13.5.1
Dorsal Ventral
4.13.5.2
4.13.6
CUTANEOUS BRANCHES
4.13.6.1
4.13.6.1.1
4.13.6.2
4.13.6.2.1
.
4.13.7
ARTICULAR BRANCHES
4.13.7.1
4.13.7.1.1
4.13.8
MUSCULAR BRANCHES
4.13.8.1
4.13.8.2
4.13.8.3
4.13.8.4
4.13.8.5
4.13.8.6
4.14 UPPER SACRAL DOR
RAM (S1-3)
Back
Table of Contents References
4.14.1
DESCRIPTION: PATH,
FUNCTION, LESIONS, CUTANEOUS AREA, AND ADDITIONAL COMMENTS
4.14.1.1
.
4.14.2
NUMBER
4.14.2.1
35
4.14.3
REFERENCE
4.14.3.1
4.14.4
ROOTS
4.14.4.1
4.14.4.2
Lumbar Plexus
4.14.4.3
VENTRAL
4.14.5
DIVISION
4.14.5.1
Dorsal Ventral
4.14.5.2
4.14.6
CUTANEOUS BRANCHES
4.14.6.1
4.14.6.1.1
4.14.6.2
4.14.6.2.1
.
4.14.7
ARTICULAR BRANCHES
4.14.7.1
4.14.7.1.1
4.14.8
MUSCULAR BRANCHES
4.14.8.1
4.14.8.2
4.14.8.3
4.14.8.4
4.14.8.5
4.14.8.6
4.15 LWR SAC&COC DR
R(ANOCOCCYGEAL N) (S4,5,C01)
Back
Table of Contents References